Trigeminal Nerve
ABSTRACT
The objective of this study is to review surgical anatomy of the trigeminal nerve. We also demonstrate some pictures involving the trigeminal nerve and its surrounding connective and neurovascular structures. Ten adult cadaveric heads were studied, using a magnification ranging from 33 to 403, after perfusion of the arteries and veins with colored latex. The trigeminal nerve is the largest and most complex of the cranial nerves. It serves as a major conduit of sensory input from the face and provides motor innervation to the muscles of mastication. Because of its size and complexity, it is essential to have thorough knowledge of the nerve before diagnoses and treatment of the pathologic processes in the orofacial, temporomandibular, infratemporal, and pterygopalatine areas. The trigeminal nerve is encountered with imaging or surgery of the skull base surgery. Thus, a comprehensive knowledge of the anatomy of the trigeminal nerve is crucial for performing the surgical procedures without significant complication.
INTRODUCTION
The trigeminal, the largest cranial nerve, is the sensory supply to the face, the major part of the scalp, the teeth, the oral and nasal cavity, and the motor supply to the masticatory and some other muscle. It also contains proprioceptive nerve fibers from the masticatory and probably the extraocular muscle. The trigeminal nerve has three divisions: ophthalmic, maxillary, and mandibular. We divide the trigeminal nerve along its course into brainstem, cisternal segment, Meckel’s cave segment, trigeminal ganglion, and peripheral divisions (ophthalmic, maxillary, and mandibular divisions).
MATERIALS AND METHODS
Ten adult cadaveric heads in which the arteries and veins were injected with colored silicone were examined under the microscope with magnifications varying from 33 to 403. The cadaveric heads were donated to the Department of Neurosurgery at the University of Florida by the State of Florida Anatomical Board. All bone work was performed with a high-speed drill (Midas Rex Institute, Fort Worth, TX).
ANATOMY
Brainstem
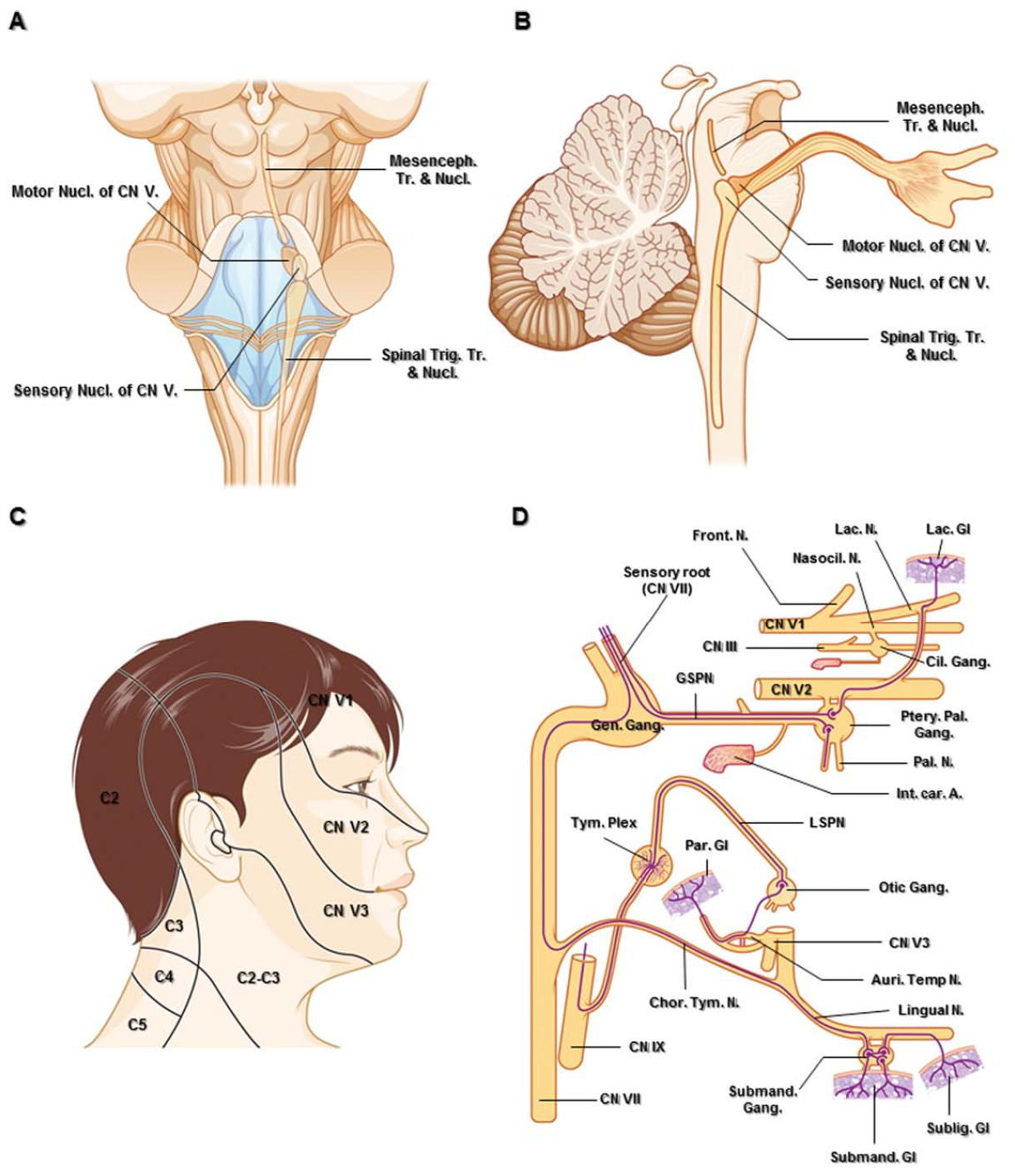
The four central nuclei of the trigeminal nerve are within the brainstem: the mesencephalic nucleus, the principal sensory nucleus, the motor nucleus, and the spinal trigeminal tract and nucleus (Figs. 1A and 1B). The mesencephalic nucleus is responsible for conveying proprioceptive fibers from the extraocular muscles and masticatory muscles and modulating the bite. Afferent fibers of the mesencephalic nucleus convey pressure and kinesthesis sense from the teeth, periodontium, hard palate, and temporomandibular joint capsule. This nucleus is concerned with mechanisms that control the force of the bite (Carpenter, 1991b). It is located within the lower midbrain and upper pons lateral to the sylvian aqueduct along the lateral margin of the periaqueductal gray matter and anterolateral to the fourth ventricle, medial to the sensory nucleus (Figs. 1A and 1B) (Go et al., 2001).
Figure 1. A. Posterior schematic anatomic view and superimposed diagram of the brain stem showing nuclei of the trigeminal nerve. The motor nucleus is situated medial to the sensory nucleus of the trigeminal nerve. B. Sagittal schematic view passing the right trigeminal nuclei. C. The cutaneous innervation of the head and upper neck. There is little overlap between the three dermatomes of the trigeminal nerve. D. Parasympathetic connections of the pterygopalatine, otic, and submandibular ganglia. The parasympathetic fibers are shown as purple lines. Abbreviations: Auri. Temp. N., auriculotemporal nerve; C., cervical; Car., carotid; Chor.Tym. N., chorda tympani nerve; Cil., ciliary; CN., cranial nerve; Front., frontal; Gang., ganglion; Gen., geniculate; Gl., gland; GSPN., greater superficial petrosal nerve; Int., internal; Lac., lacrimal; Mesenceph., mesencephalic; N. nerve; Nasocil., nasociliary; LSPN., lesser superficial petrosal nerve; Nucl., nucleus; Par., parotid; Ptery. Pal., pterygopalatine; Subling., sublingual; Submand., submandibular; Tr., tract; Trig., trigeminal; Tym. Plex., tympanic plexus. (Images courtesy of AL Rhoton, Jr.)
The principal sensory nucleus convey impulses for tactile and pressure sense. It is arranged in dorsoventral organization. Fibers of the ophthalmic division terminate ventrally, fibers of the maxillary division are intermediate, and fibers of the mandibular division are most dorsal. This nucleus lies lateral to the entering trigeminal root fibers in the upper pons. Trigeminal fibers from the principal sensory nucleus are both crossed and uncrossed to terminate the ventral posteromedial (VPM) nucleus of the thalamus. Crossed fibers originated from the ventral part of the nucleus ascend in association with the contralateral medial lemniscus to form ventral trigeminothalamic tract. Uncrossed fibers originated from the dorsomedial part of the nucleus ascend close to the central gray of the midbrain to form dorsal trigeminothalamic tract (Carpenter, 1991b).
The motor nucleus is medial to the principal sensory nucleus. Fibers from this nucleus exit from the brain stem medial to the entering sensory root, pass underneath the trigeminal ganglion without synapse, and become incorporated in the mandibular division. Axons from the mesencephalic nucleus project to the motor nucleus, completing a reflex arc in modulating the degree of bite (Go et al., 2001).
The spinal trigeminal tract and nucleus relays the sensory modalities of pain and temperature. It extends from the midpons to the cervical cord at the level C2-C4 and lies anterolateral to the fourth ventricle (Barakos et al., 1990; Carpenter, 1991b). Root fibers entering the spinal trigeminal tract and nucleus have a definite topographical organization caused by medial rotation of the sensory root as it enters the pons. Fibers of the ophthalmic division are most ventral, fibers of the mandibular division are most dorsal, and those of the maxillary division are intermediate and descend less far caudally than the other divisions. The spinal trigeminal nucleus consists of three parts: (1) a pars oralis, (2) a pars interpolaris, and (3) a pars caudalis. The pars oralis receives impulses predominantly from internal structures of the nose and mouth. The pars interpolaris is related mainly to cutaneous facial regions, while the pars caudalis has large receptive field over the forehead, cheek, and jaw. This topographic anatomy of the spinotrigeminal pathway may explain the onion peel representation of the face in the descending spinotrigeminal tract (Carpenter, 1991b; Kunc and Ceskoslovenská akademie věd, 1964).
Trigeminal Root (Cisternal Segment)
The trigeminal nerve arises from one motor nucleus and three sensory nuclei, which extend throughout most of the length of the brain stem. The trigeminal root is composed of the large sensory root and the small motor root. The sensory root receives somatosensory sensation from the entire face (except the angle of the jaw innervated by the cervical plexus), temple, external acoustic meatus, and the anterior scalp as far posterior as the vertex of the skull (Fig. 1C) (Shankland, 2000). Although most cell bodies of the somatosensory neurons are located in the trigeminal ganglion, the cell bodies for proprioception and stretch receptors in the muscles of mastication are located in the mesencephalic nucleus in the dorsal pons (Dodd and Kelly, 1991). The proprioceptive impulses from the masticatory muscle run through the motor root to enter the mesencephalic nucleus (Fig. 1B) (Gray and Williams, 1989b; Shankland, 2000).
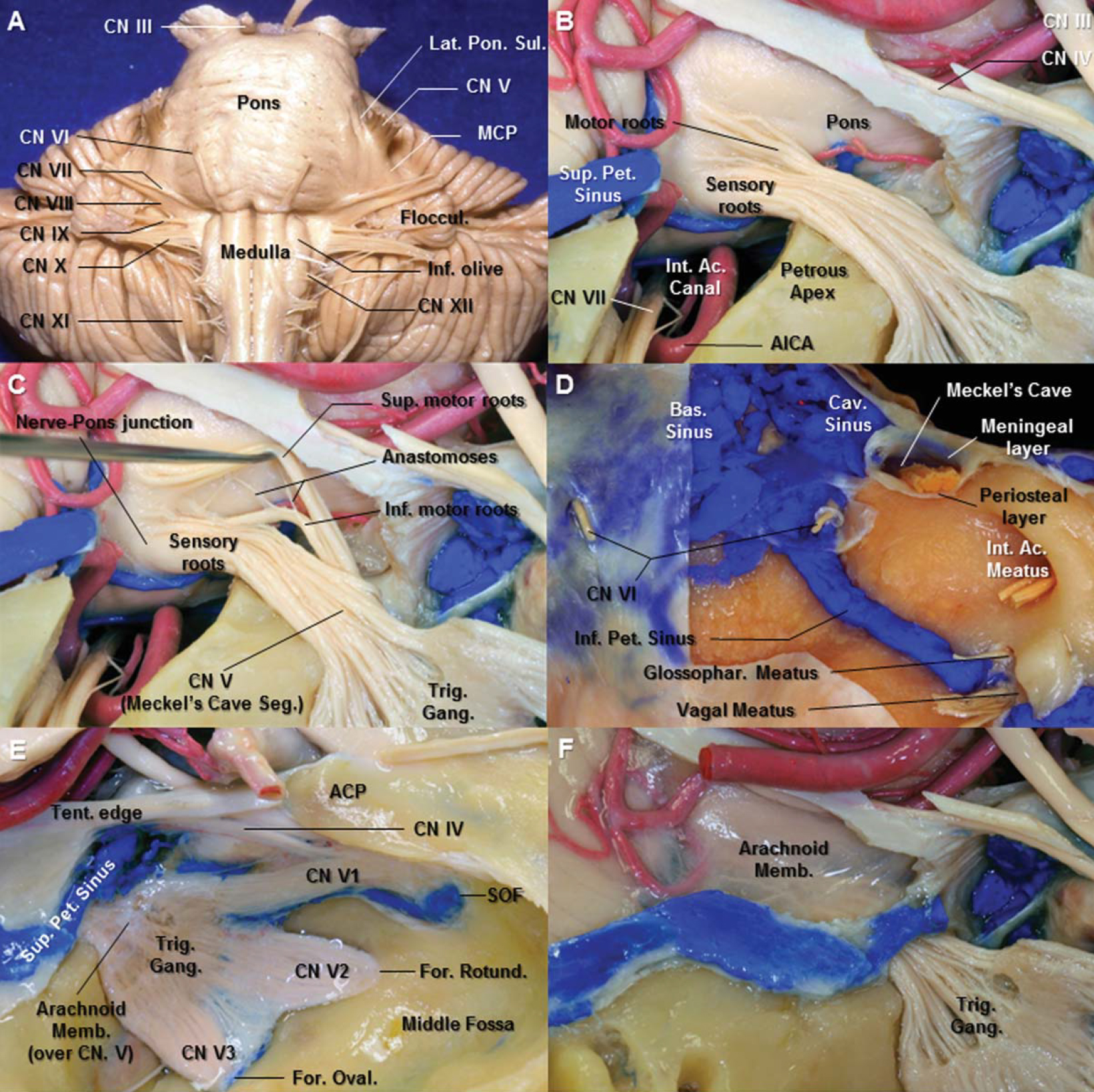
The large sensory rootlets of the trigeminal nerve exit the lateral aspect of the midpons medial to middle cerebellar peduncle with the ophthalmic division being most inferior, the maxillary in the middle, and the mandibular division in the superior position (Fig. 2A). As the roots pass anteriorly through the prepontine cistern and Meckel’s cave to the trigeminal ganglion in the middle fossa, they rotate approximately lateral 180 degree rotation (Jannetta, 1996; Shankland, 2000). However, Rhoton (2000) reported that the fibers from the mandibular division remain in a caudolateral position in the trigeminal root throughout the interval from the ganglion to the pons, the ophthalmic division rostromedial, with maxillary division fibers in an intermediate position (Rhoton, 2000).
Figure 2. A. Anterior view of the brain stem. The middle cerebellar peduncle is separated from the pons by a lateral pontine sulcus. Just lateral to the lateral pontine sulcus is the emergence of the trigeminal nerve. From the microsurgical standpoint, the apparent origin of the trigeminal nerve can be considered as the limit between the pons and the middle cerebellar peduncle. B. Lateral view of the right trigeminal root entry zone. The tentorium and the occipital lobe have been removed to expose the root entry zone of the trigeminal nerve. The small roots emerge from the pons superomedial to the large sensory root. The roof of the internal acoustic canal has been removed. C. The two motor rootlets groups of the trigeminal nerve, a primary superior and a secondary inferior motor rootlets, are visualized after superior retraction of the superior motor group from the sensory root. D. The dura of the anterior aspect of the posterior fossa has been removed to expose the basilar plexus, cavernous sinus, and inferior petrosal sinus. Meckel’s cave is a cleft-like dural pocket that originates from the dura propria of the posterior fossa. The cave is situated at the trigeminal impression between the meningeal layer (dura propria) and the periosteal layer of dura. E. The arachnoid membrane from the posterior fossa extends to Meckel’s cave, forming a pocket within the cave, continues along the rootlets of the trigeminal nerve. F. The arachnoid membrane over the trigeminal root has been removed. The superior petrosal sinus extends medially through the upper edge of the porus of Meckel’s cave and above the trigeminal nerve to join the cavernous sinus. Abbreviations: Ac., acoustic; ACP., anterior clinoid process; AICA., anterior inferior cerebellar artery; Bas., basilar; Cav., cavernous; CN., cranial nerve; For., foramen; Gang., ganglion; Glossophar., glossopharyngeal; Inf., inferior; Int., internal; MCP., middle cerebellar peduncle; Memb., membrane; Oval., ovale; Pet., petrosal; Rotund., rotundum; Seg., segment; SOF., superior orbital fissure; Sup., superior; Tent., tentorium; Trig., trigeminal. (Images courtesy of AL Rhoton, Jr.)
The small motor roots emerge from the pons anterosuperomedial to the entry point of the large sensory root (Saunders and Sachs, 1970; Lang, 1981). Some authors defined two motor rootlets groups of the trigeminal nerve; a primary superior and a secondary inferior motor rootlets, with numerous connections between both of these and the sensory root. The superior rootlets group, with its distinct position, and relative isolation from the main sensory root, represents the classic origin of the motor root (Fig. 2B) (Saunders and Sachs, 1970; Lang, 1981; Yousry et al., 2004). The inferior motor rootlets are visualized after retraction of the superior motor group from the sensory root (Figs. 2B and 2C). Pelletier at al. (1974) contend that the physiological characteristics of the inferior motor root were identical to that of the motor fibers and subserved either a motor or proprioceptive function rather than a sensory function (Pelletier et al., 1974). The two separate motor groups join together a short distance from the brain stem to form a single root and passes through the Meckel’s cave on the medial side of the sensory root and ganglion to join the mandibular division (Fig. 2C).
Peker et al. reported cisternal portion of the 100 trigeminal nerves measured 12.3 mm (range 8–15 mm). The root exit zone (REZ) of trigeminal nerve (the precise nerve-pons junction) and central-peripheral myelin transition zone (TZ), mentioned in the trigeminal neuralgia, are separate structures. The length of central myelin (distance from pons to TZ) on the medial aspect of the nerve (range, 0.1–2.5 mm; mean, 1.13 mm; median, 1 mm) was shorter than that on the lateral aspect (range, 0.17–6.75 mm; mean, 2.47 mm; median, 2.12 mm) (Peker et al., 2006).
Meckel’s Cave Segment
The cisternal segment of the trigeminal nerve in the posterior fossa passes forward below the tentorial edge and superior petrosal sinus between the periosteal and meningeal (dura propria) layers of middle fossa dura to enter Meckel’s cave. Meckel’s cave is a cleft-like dural pocket that originates from the dura propria of the posterior fossa, between the two layers of the middle fossa dura, and extends from the posterior fossa into the posteromedial portion of the middle cranial fossa (Figs. 2D–2F). The superior petrosal sinus extends medially through the upper edge of the porus of Meckel’s cave and above the trigeminal nerve to join the cavernous sinus. The abducens nerve pierces the posterior fossa dura inferomedial to the porus trigeminus (Fig. 2D).
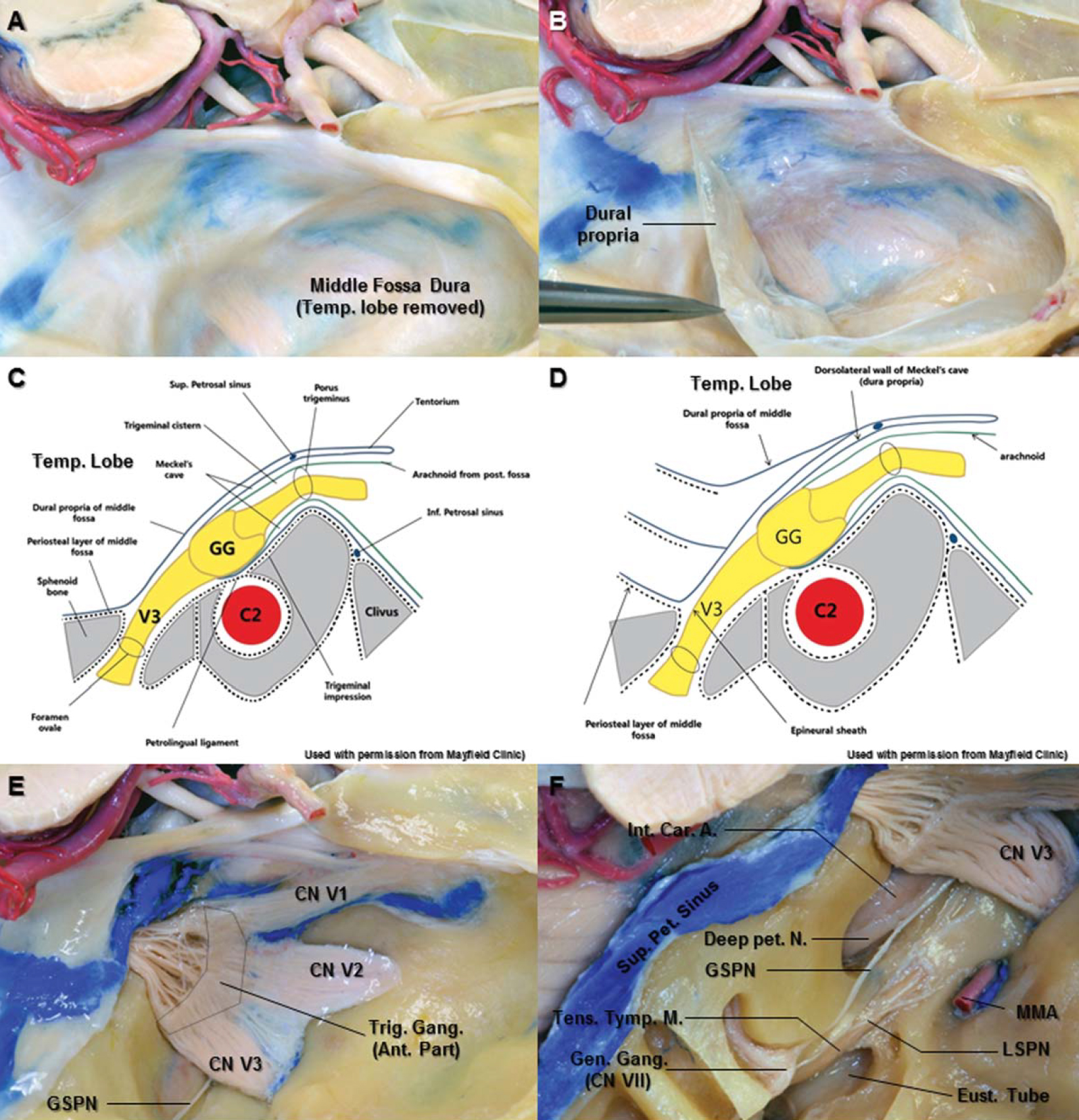
The cave is situated at the trigeminal impression between the meningeal layer (dura propria) and the periosteal layer of dura which appears to be tightly attached to the petrous apex (Fig. 2D). The arachnoid membrane from the posterior fossa extends to Meckel’s cave, forming a pocket within the cave, and continues along the rootlets of the trigeminal nerve as far as the trigeminal ganglion (Figs. 2E and 2F) (Sabanci et al., 2011). The contents of the Meckel’s cave are the sensory and motor roots of the trigeminal nerve, trigeminal ganglion, and arachnoid layer (Figs. 3C and 3D). The anterior portion of the trigeminal ganglion tightly adheres to the overlying arachnoid and dura propria of Meckel’s cave without any potential subarachnoid space (Fig. 3E). The subarachnoid space within Meckel’s cave is behind the trigeminal ganglion and is actual space that constitutes the trigeminal cistern (Figs. 2E, 2F, 3C, and 3E) (Youssef et al., 2006). The trigeminal ganglion and trigeminal roots have two layers of dura propria on their superolateral aspect. The inner layer, the dura propria, constitutes the superolateral wall of Meckel’s cave. The outer layer is the meningeal layer (dura propria) of the middle fossa. The cleavage plane is formed laterally between the epineural sheaths of the trigeminal nerves (inner layer) and dura propria of the middle fossa (outer layer). This cleavage plane serves as the anatomic basis for the interdural exposure of the contents of Meckel’s cave (Figs. 3A–3D) (Kawase et al., 1996; Yoshida and Kawase, 1999; Al-Mefty et al., 2002; Youssef et al., 2006). However, the limits of the Meckel’s cave decided by its meningeal architecture remain controversial (Taptas, 1982; Kapila et al., 1984; Kawase et al., 1996; Kehrli et al., 1997). According to Sabanci et al. (2011), the meningeal pouch (Meckel’s cave) extended beyond the trigeminal ganglion along the three divisions in some specimens, and in the others, it ended at the level of the ganglion (Sabanci et al., 2011).
Figure 3. A. The right temporal lobe has been removed to expose the middle fossa dura. B. The dura propria of the middle fossa dura has peeled off to the posterior direction from the middle fossa floor. The trigeminal nerve has visualized. C. Oblique coronal section along the line between the porous trigeminus and the foramen ovale (used with permission from Mayfield Clinic). At the anterior margin of the trigeminal ganglion, the dorsolateral and ventromedial walls of Meckel’s cave become an epineural sheath of each division of trigeminal nerve. The contents of the Meckel’s cave are the sensory and motor roots of the trigeminal nerve, trigeminal ganglion, and arachnoid layer. D. The endosteal incision near the foramen ovale leads to cleavage plane between the outer layer (dura propria of middle fossa, meningeal layer) and inner layer (epineural sheath of the mandibular nerve) (used with permission from Mayfield Clinic). E. The anterior portion of the trigeminal ganglion tightly adheres to the overlying arachnoid and dura propria of Meckel’s cave without any potential subarachnoid space. The arachnoid layer has been easily removed from the posterior portion of the trigeminal ganglion due to actual subarachnoid space. F. Superior view of the right temporal bone. The bone on the middle fossa floor has been removed laterally to show the petrous segment of the carotid artery, the Eustachian tube, the tensor tympani muscle, and geniculate ganglion of the facial nerve. The greater superficial petrosal nerve is separated from the horizontal segment of the petrous internal carotid artery. It passes under V3 and joins the deep petrosal nerve from the sympathetic carotid plexus to become the vidian nerve in the vidian canal. Abbreviations: A., artery; C2., petrous carotid artery; Car., carotid; CN., cranial nerve; Eust., Eustachian tube; Gang., ganglion; Gen., geniculate; GG., gasserian ganglion; GSPN., greater superficial petrosal nerve; Inf., inferior; Int., internal; LSPN., lesser superficial petrosal nerve; MMA., middle meningeal artery; N., nerve; Pet., petrosal; Sup., superior; Tens. Tymp.M., tensor tympani muscle; Trig., trigeminal; V3., mandibular division. (Images courtesy of AL Rhoton, Jr.)
The greater superficial petrosal nerve (GSPN) is located posterolateral to the Meckel’s cave (Fig. 3F). The GSPN originates at the geniculate ganglion, exits through facial hiatus, and runs under the dura in an anteromedial direction toward the mandibular division (V3). The facial nerve hiatus was found on to be 12.8 mm posterolateral MC (Arslan et al., 2012). The GSPN is separated from the horizontal segment of the petrous internal carotid artery (ICA). It passes under V3 and joins the deep petrosal nerve from the sympathetic carotid plexus to become the vidian nerve in the vidian canal. The distal part of the vidian nerve will be reviewed in the part of maxillary division.
The horizontal segment of the petrous ICA is situated just below the MC. The horizontal segment begins at the distal end of the posterior genu, courses anteromedially along the long axis of the petrous part of the temporal bone, largely below the GSPN, posterior to the tensor tympani muscle and eustachian tube, and posterior to the foramen spinosum and ovale, and ends below the trigeminal nerve and ganglion at the anterior genu, where the artery turns upward above the fibrocartilage-filled foramen lacerum (Fig. 3E, 12A, and 12B) (Osawa et al., 2008).
It is important to understand the relationships of the trigeminal nerve and the autonomic fibers. In the head, there are four parasympathetic ganglia which are associated with the trigeminal nerve: the ciliary, pterygopalatine, otic, and submandibular ganglia (Fig. 1D).
Ophthalmic Division
The ophthalmic nerve (V1) is the smallest of the three divisions of the trigeminal nerve. The oculomotor, trochlear, abducens, and V1 nerves are found within the cavernous sinus. From the trigeminal ganglion, the V1 is inclined upward as it passes forward in the lower part of the lateral wall of the cavernous sinus to reach the superior orbital fissure (Figs. 4A and 4B). The V1 branches into the lacrimal, frontal, and nasociliary nerves as it approaches the SOF. The SOF is a small but topographically important area, which connects the middle cranial fossa and the orbit (Fig. 4A) (Natori and Rhoton, 1995; Govsa et al., 1999).
Figure 4. A. Posterior view of the right superior orbital fissure (SOF). The SOF is bounded above by the lesser wing of the sphenoid bone, below by the greater wing, and medially by the sphenoid body. The optic strut forms the upper medial border of the fissure. The SOF provides a communication between the orbit and the middle fossa. B. Lateral view of the right cavernous sinus. The lateral wall of the cavernous sinus and the anterior clinoid process have been removed. The oculomotor, trochlear, abducens, and ophthalmic division (V1) are situated within the cavernous sinus. They enter the orbit through the SOF. C. Superolateral view of the right frontotemporal area. After performing the fronto-temporal craniotomy, the dura is elevated. The fronto-temporal dural fold is located on the lateral side of the SOF, between the greater and lesser wings of the sphenoid bone. D. Resecting the dural fold allows further detachment of the dura from the surrounding structures, enabling extradural exposure of the anterior portion of the cavernous sinus and the third, fourth cranial nerves as well as the fifth cranial nerve. E. Superior view of the right orbit and the optic canal. At the SOF, the dura covering the optic nerve, middle fossa, and the cavernous sinus blends into the periorbita of the orbital apex. F. Anteroinferior view of the right orbit. The rectus muscles originate from the annular tendon. The annular tendon surrounds the orbital end of the optic foramen and the adjacent part of the SOF. The fibrous component, which blend together to form the annular tendon, are the periorbita covering the orbital apex, the dura lining the SOF and optic canal, and the optic sheath. G. Superior view of the right SOF. The dura covering the cavernous sinus and the optic sheath blend into the periorbita of the orbital apex and into annular tendon from which the rectus muscles arise. H. Schematic anterior view of the main structures passing through a right SOF. Abbreviations: A., artery; ACP., anterior clinoid process; Cav., cavernous; CN., cranial nerve; Div., division; For., foramen; Front., frontal; Inf., inferior; Lac., lacrimal; Lat., lateral; Lev., levator; M., muscle; Med., medial; N., nerve; Nasocil., nasociliary; Obl., oblique; Oculom., oculomotor; Ophth., ophthalmic; PCP., posterior clinoid process; Rec., rectus; Rotund., rotundum; SOF., superior orbital fissure; Sph., sphenoid; Sup., superior; Temp., temporal; V., vein. (Images courtesy of AL Rhoton, Jr.)
Superior orbital fissure. The superior orbital fissure (SOF) is the narrow cleft through which the orbit communicates with the middle cranial fossa. The SOF is situated between the greater and lesser wings and body of the sphenoid bone. It has a somewhat triangular shape, having a wide base medially on the sphenoid body and a narrow apex situated laterally between the lesser and greater wings (Fig. 4A). At the level of the SOF, the outer and inner layers of the lateral wall of the cavernous sinus separate from one another (Kawase et al., 1996). The inner layer, which is composed of the cranial nerve perineurium and surrounding connective tissue, extends with the nerves into the posterior orbit. The outer layer is formed by the temporal fossa dura (Figs. 3A, 3B, and 4B). Along the lateral margin of the SOF, the periosteal layer of the dura mater is contiguous with the periosteal layer of the periorbita (Froelich et al., 2007). This dural bridge, at the lateral edge of the SOF, is the frontotemporal periosteal fold stretched between the periorbita and temporal dural fold. The cleavage plane between the temporal dura and the inner layer of the lateral wall of the cavernous sinus develops after cutting the fronto-temporal periosteal fold (Figs. 4C and 4D) (Day et al., 1994; Kawase et al., 1996). Froelich et al. (2007) reported that the lacrimal nerve of the V1 may be at risk during incision of periosteal fold because it is just medial to surgical cleavage plane (Figs. 4F and 4H) (Froelich et al., 2007). The distance between the lacrimal nerve and lateral end of the SOF was 4.21 ± 1.72 mm (Shi et al., 2007).
At the fissure, the dura covering the middle fossa and cavernous sinus blends into the periorbita of the orbital apex and into annular tendon from which the rectus muscles arise (Figs. 4E and 4G). The annular tendon can be used to divide the SOF into three regions: the central, lateral, and inferior sectors (Fig. 4H) (Natori and Rhoton, 1995; Shi et al., 2007). The annular tendon surrounds the orbital end of the optic canal and the adjacent part of the SOF. The central sector of the SOF surrounded by the annular tendon is called the oculomotor foramen because it is the part of the fissure through which the oculomotor nerve passes. The abducens and nasocillary nerves and branches of the carotid sympathetic plexus also pass through the oculomotor foramen (Figs. 4H, 6A, and 6C). The nasociliary nerve is separated from the oculomotor and abducens nerves by the fibrous septum in the oculomotor foramen (Fig. 6D). The lateral sector is defined as lateral to the annular tendon and transmits the trochlear, frontal, and lacrimal nerve, all of which pass through the fissure outside the annular tendon (Figs. 4H and 5B). The lacrimal nerve occupies the most lateral part of the fissure, with the frontal nerve being more medial (Figs. 4F and 4H) (Natori and Rhoton, 1995; Shi et al., 2007). The inferior sector of the SOF is situated below the annular tendon. The inferior rectus muscle arises from the annular tendon at the upper margin of this sector. Orbital fat extends backward below the inferior rectus muscle into this part of the fissure. This sector contains the inferior ophthalmic vein and orbital fat.
Figure 5. A. Superior view of the right orbit after removal of the orbital roof. The periorbita has been incised and retracted to expose the frontal, lacrimal, and trochlear nerves. B. The orbital fat has been removed to expose the main structures of the orbit. The frontal nerve arises in the lateral wall of the cavernous sinus and passes through the narrow lateral part of the SOF on the medial side of the lacrimal nerve and superior ophthalmic vein and below the trochlear nerve. It runs forward between the levator muscle and the periorbita. C. The levator palpebral and superior rectus muscles have been retracted posteromedially to expose optic, nasociliary, and abducens nerves. The nasociliary nerve passes forward above the optic nerve to reach the medial part of the orbit between the superior oblique and medial rectus muscles. D, E. Lateral view of the right SOF. The lesser wing of the sphenoid bone has been removed to open the SOF. At the level of the fissure, the nasociliary nerve ascends laterally to the inferior division of the oculomotor nerve and then crosses medially between the two divisions of the oculomotor nerve. Abbreviations: CN., cranial nerve; For., foramen; Front., frontal; Gl., gland; GSPN., greater superficial petrosal nerve; Lac., lacrimal; Lat., lateral; Lev., levator palpebral; M., muscle; MMA., middle meningeal artery; Nasocil., nasociliary; N., nerve; Obl., oblique; Oph., ophthalmic; Ptery., pterygoid; Rec., rectus; Rotund., rotundum; SOF., superior orbital fissure; Sup., superior; Suporb. N., supraorbital nerve; Sup.-Troch. N., supratrochlear nerve. (Images courtesy of AL Rhoton, Jr.)
Figure 6. A. Lateral view of the right SOF. The lesser wing of sphenoid bone and lateral wall orbit have been removed to expose the structures passing through the SOF. The frontal nerve has been retracted inferolaterally. The lateral sector transmits the trochlear, frontal, and lacrimal nerves, all of which pass through the fissure outside the annular tendon. B. Superior view of the right orbital apex. The optic nerve has been retracted medially to expose the ciliary ganglion. The ciliary ganglion receives parasympathetic motor root from the inferior oculomotor nerve, sensory root from the nasociliary nerve, and sympathetic fibers from the plexus around ophthalmic artery. C. Enlarged view of the SOF. The lateral margin of the SOF in (A) has been removed. The oculomotor foramen is the portion of the opening in the annular tendon lateral to the optic foramen through which the superior and inferior divisions of the oculomotor nerve and the nasociliary nerve and abducens nerve pass. The nasociliary nerve is situated above and lateral to the abducens nerve in the anterior part of the cavernous sinus. D. the annular tendon has been divided between the origin of the superior and lateral rectus muscles. The nasociliary nerve separates from the oculomotor and abducens nerves by fibrous septum within the oculomotor foramen. E. The levator and superior rectus muscles have been reflected medially and lateral rectus muscle has been reflected laterally to expose the right optic nerve (removed) and short ciliary nerve arising from the ciliary ganglion. F. Anterior view of the right orbit and extraocular muscles after removing the eye globe and optic nerve. The lacrimal nerve courses along the superior margin of the lateral rectus muscle. The nasociliary nerve gives rise to long ciliary nerves that enter the sclera around the optic nerve with the short ciliary nerves arising from the ciliary ganglion. Abbreviations: A., artery; Cil., ciliary; CN., cranial nerve; Div., division; Front., frontal; Gang., ganglion; Inf., inferior; Lac., lacrimal; Lat., lateral; M., muscle; N., nerve; Nasocil., nasociliary; Obl., oblique; Ophth., ophthalmic; Rec., rectus; SOF., superior orbital fissure; Sup., superior; Sympath., sympathetic. (Images courtesy of AL Rhoton, Jr.)
Frontal nerve. The frontal nerve is the largest division of the branches of the V1. The frontal branch of the V1 arises in the lateral wall of the cavernous sinus and passes through the narrow lateral part of the superior orbital fissure on the medial side of the lacrimal nerve and superior ophthalmic vein and below the trochlear nerve. It runs forward between the levator palpebral muscle and the periorbita. It is visualized through the periorbita after removal of the orbital roof (Figs. 5A, 5B, and 5D). The frontal nerve courses outside and superolateral to the annular tendon and divides into the supratrochlear and supraorbital nerves within the orbit (Fig. 5B).
Supratrochlear nerve. The supratrochlear nerve runs anteriorly above the trochlea of the superior oblique muscle with the supratrochlear artery (Figs. 5B and 5C). The nerve gives off a descending filament to the infratrochlear branch of the nasociliary nerve. The supratrochlear nerve exited between the trochlea and the supraorbital foramen and was located 16 mm lateral to the midline (range, 12-21 mm) and 7 mm below the upper margin of the supraorbital rim (range, 6-9 mm) (Jeong et al., 2010). The supratrochlear nerve is located medial to the supraorbital nerve at the supraorbital rim (Cuzalina and Holmes, 2005). It supplies the conjunctiva and the skin of the upper eyelid and ascends beneath the corrugator and the frontal belly of occipitofrontalis, dividing into branches which pierce these muscles to supply the skin of the lower forehead near the midline (Gray and Williams, 1989b).
Supraorbital nerve. The supraorbital nerve courses between the levator palpebrae muscle and orbital roof. The supraorbital nerve exited the supraorbital notch or foramen 29 mm lateral to the midline (25–33 mm) and 5 mm below the upper margin of the supraorbital rim (range, 4–6 mm) (Jeong et al., 2010). The nerve innervates the upper eyelid, the mucous membrane of the frontal sinus of the frontal bone, the galea aponeurosis, and the orbicularis oculi. It ascends on the forehead, dividing into a smaller medial and a lateral branch, which supply the skin of the scalp nearly as far back as the lambdoid suture (Gray and Williams, 1989b; Shankland, 2001a). It may also carry some sympathetic fibers to the globe and pupillary dilator (Rhoton, 2003b). The supraorbital nerve may transmit autonomic fibers from the cervical sympathetic ganglia to the lobe and pupillary dilator (Martins et al., 2011).
Nasociliary nerve. The nasociliary nerve, intermediate in size between the frontal and lacrimal nerves, is more deeply placed in the orbit. The nasociliary nerve arises from the medial side of the V1 and is situated above and lateral to the abducens nerve in the anterior part of the cavernous sinus (Figs. 5C–5E). Both the abducens and the nasociliary nerves course medial to the part of the V1 from which the lacrimal and frontal nerves arise. At the level of the fissure, the nasociliary nerve gently ascends laterally to the inferior division of the oculomotor nerve and then crosses medially between the two divisions of the oculomotor nerve and above the optic nerve to reach the medial part of the orbit, where it gives rise to the anterior and posterior ethmoidal and infratrochlear nerves (Figs. 5C and 5E).
The nasociliary nerve connects with the ciliary ganglion and gives off the long ciliary nerves. The sensory root of the ciliary ganglion arises from the nasociliary nerve. This sensory root courses forward on the lateral side of the optic nerve and enters the ciliary ganglion but does not synapse with any cell bodies. Several fine filaments known as the short ciliary nerves leave the ciliary ganglion and convey sensation to cornea and globe. The long ciliary nerves accompany the short ciliary nerves to pierce the sclera near the attachment of the optic nerve. The long ciliary nerves convey sympathetic fibers to the globe and pupillary dilator and may also carry some sensation from the globe and cornea (Figs. 6B, 6E, and 6F) (Rhoton, 2003b; Shankland, 2001a).
Lacrimal nerve. The lacrimal nerve is the smallest of the three division of the V1. It arises at the level of or just behind the SOF from the lateral edge of the V1 and passes through the lateral edge of the fissure on the lateral side of the frontal nerve and above the superior ophthalmic vein (Figs. 4H and 5A–5C). On entering the orbit, the lacrimal nerve courses along the superior margin of the lateral rectus muscle and serve as a bridge to parasympathetic twigs directed to the lacrimal gland (Figs. 6C and 6F). These twigs are related to the pterygopalatine ganglion (PPG). The postganglionic parasympathetic motor fibers containing lacrimal secretomotor fibers, carried by the zygomatic branch of the maxillary division, which course along the lateral orbital wall, join the lacrimal nerve (Fig. 1D) (Shankland, 2001a; Rhoton, 2003b; Martins et al., 2011). The lacrimal nerve also conveys sensation from the area in front of the lacrimal gland.
Ciliary ganglion. The ciliary ganglion is located at the inferolateral aspect of the optic nerve and at the medial side of the lateral rectus muscle. The ganglion is an oval-shaped collection of cell bodies about 3 mm in size (Figs. 6B, 6E, and 6F). The mean distance between the ganglion and the optic nerve was 2.9 mm (range, 2.7–3.1 mm) and the mean distance between the lateral rectus muscle and the ganglion was 10.4 mm (range: 9.2–11.2 mm) (Izci and Gonul, 2006). It receives three branches: parasympathetic motor root from the branch of the inferior oculomotor division to the inferior oblique muscle, sensory root from the nasociliary nerve, and sympathetic fibers from the plexus around the ophthalmic artery (Figs. 1D, 6B, 6E, and 6F).
The parasympathetic fibers, originated in the Edinger-Westphal nucleus of the oculomotor complex in the midbrain, synapse in the ciliary ganglion, which gives rise to the short ciliary nerves. These fibers supply the ciliary muscle and the sphincter of the pupil. The sympathetic fibers ascend on the surface of the internal carotid artery, pass through the central sector of the SOF, and course with the ophthalmic artery. The sympathetic fibers, which relay in the superior cervical ganglion, traverse the ciliary ganglion without synapse and enter the short ciliary ganglion. The sensory root from the nasociliary nerve passes to the globe through the short ciliary nerves and convey sensation to cornea and globe (Fig. 6B).
Maxillary Division
The maxillary nerve (V2), the intermediate division of the trigeminal nerve, is purely sensory in function. The V2 gives sensory innervation to all structures in and around the maxillary bone and the mid-facial region including the skin of the mid-facial regions, the lower eyelid, side of the nose and upper lip; the mucous membrane of the nasopharynx, maxillary sinus, soft palate, palatine tonsil, roof of the mouth, the maxillary gingiva, and maxillary teeth (Fig. 1C) (Shankland, 2001b).
Conflicting statements exist in the literatures regarding the presence or absence of V2 within the cavernous sinus. In many classic textbooks, oculomotor, trochlear, V1, and V2 are described as being embedded in the lateral wall of the cavernous sinus (Hollinshead, 1982a; Dolenc, 1989; Gray and Williams, 1989a; Fix, 1995). However, some authors have stated that V1 is the only part of the trigeminal nerve to reside in the cavernous sinus (Carpenter, 1991a; Rhoton, 2003a; Tubbs et al., 2008). The V2 leaves the middle portion of the trigeminal ganglion between ophthalmic (V1) and mandibular (V3) divisions. The V2 does not course in the lateral wall of the dural envelop of the cavernous sinus as does the ophthalmic nerve (Figs. 4B and 8B). It courses beneath the dura of the middle fossa below the level where the medial and lateral walls of the cavernous sinus join at the lower edge of the ophthalmic nerve. As the dura is elevated from the floor of the middle fossa, it can be stripped upward off the lateral aspects of both the V1 and V2 nerves, but only the ophthalmic nerve has the venous space of the cavernous sinus on its medial side (Fig. 4D) (Rhoton, 2003a). The laterotrigeminal venous system, which is the venous system surrounding the foramen ovale and V3, may be extend to the region of the foramen rotundum and lateral aspect of the V2. The venous vascularization of this area may cause a bleeding in surgical intervention of the middle cranial fossa (Figs. 8A and 8B) (Simoes, 1993; Tubbs et al., 2008).
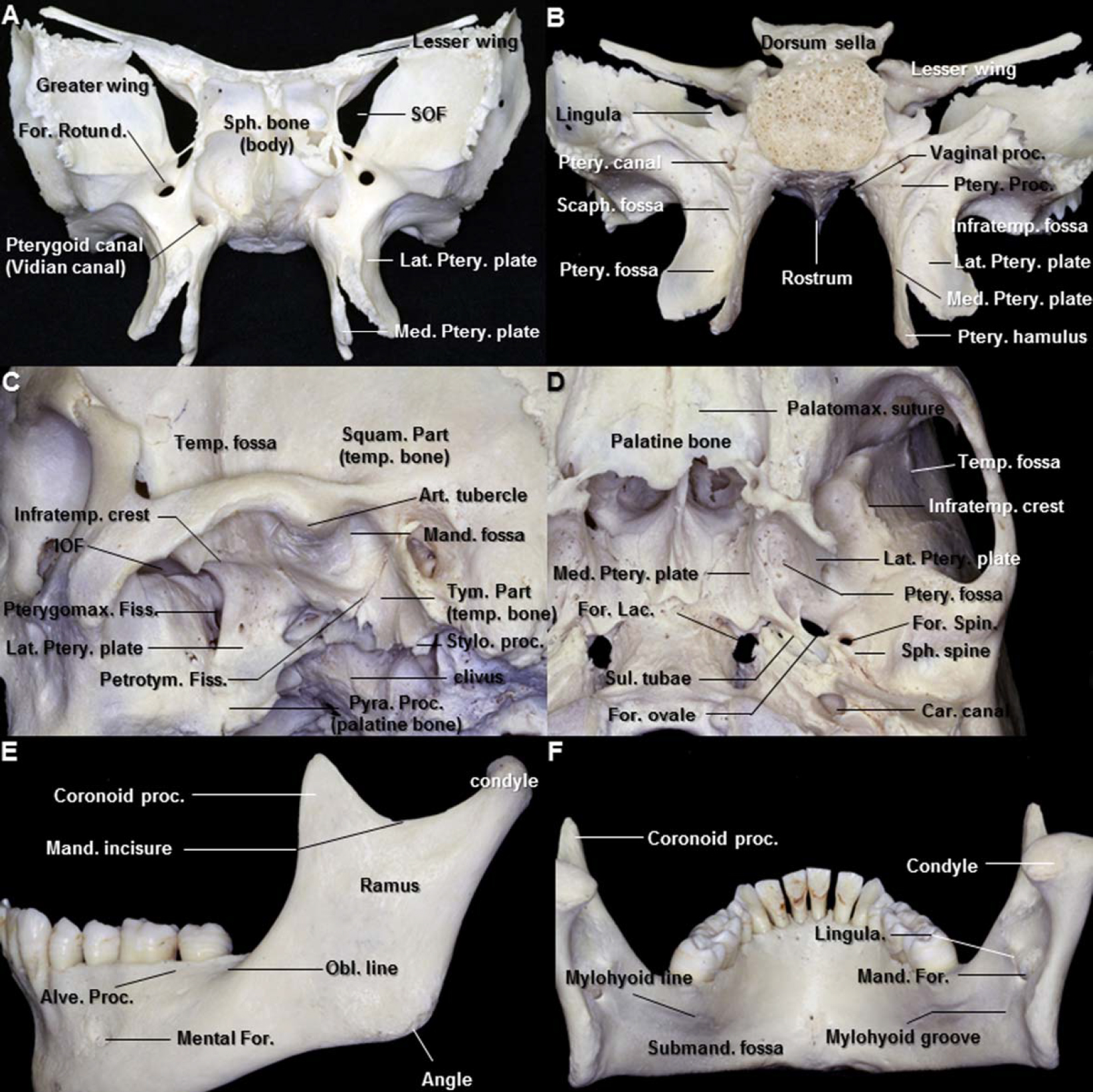
The maxillary nerve passes through the foramen rotundum to enter the pterygopalatine fossa (PPF), where it becomes more cylindrical and compact. The PPF is pyramidal space located between the pterygoid bone posteriorly, the perpendicular plate of the palatine bone anteromedially, and maxilla anterolaterally. It opens laterally into the medial part of the infratemporal fossa through the pterygomaxillary fissure and superiorly through the medial part of the inferior orbital fissure into the orbital apex (Figs. 7C and 7D). The fossa also communicates with middle cranial fossa posterolaterally through the foramen rotundum, with foramen lacerum posteromedially through the vidian canal, with the nasopharynx medially through the palatovaginal canal, with the oral cavity inferomedially through the palatine foramina, and with nasal cavity medially through the sphenopalatine foramen (Figs. 7A, 7B, and 8D) (Alfieri et al., 2003). It contains maxillary nerve, PPG, maxillary artery, and their branches, all embedded in fat tissue. The anterior compartment of the PPF contains the third segment of the internal maxillary artery and its branches (Morton and Khan, 1991). The posterior compartment of the PPF contains the PPG and its branches the maxillary nerve (V2) (Figs. 8C–8E, and 8F) (Alfieri et al., 2003).
Figure 7. A. Anterior view of the sphenoid bone. The anterior opening of the vidian canal is situated inferomedial to the foramen rotundum. B. Posterior view of the sphenoid bone. The pterygoid processes of the sphenoid descend perpendicularly from the region where the greater wings unite with the body. Each process consists of the medial and a lateral plate, the upper parts of which are fused anteriorly. The medial pterygoid plate is narrower and longer than the lateral; its lower end curves laterally into a hook-like process, the pterygoid hamulus, around which the tendon of the tensor veli palatini is deflected. C. Lateral view of the infratemporal fossa. The pyramidal process of the palatine bone fits into the angular interval between the lower ends of the pterygoid plates. The medial portion of the tympanic part of the temporal bone forms the posterior boundary of the petrotympanic fissure. D. Inferior view of the infratemporal fossa. The sulcus for auditory tube, which is the attachment site of the cartilaginous part of the Eustachian tube to the cranial base, is located on the extracranial surface of the sphenopetrosal fissure, anterolateral to the foramen lacerum and posteromedial to the foramen ovale and spinosum. The foramen ovale, which is irregularly oval, lies close to the upper end of the posterior margin of the lateral pterygoid plate. E. Lateral view of the mandible. The oblique line in the mandible runs upward and backward from the mental tubercle and is continuous with the anterior border of the ramus. The upper border of the ramus is thin and bounds a wide notch, the mandibular incisures, which transmits the masseteric nerve and vessels from the infratemporal fossa. F. Posterior view of the mandible. The mandibular canal runs from the mandibular foramen obliquely downward and forward in the ramus and then horizontally forward in the body. The mylohyoid line is the origin of the mylohyoid muscle. The lingula, the medial border of the mandibular foramen, is the attachment site of the sphenomandibular ligament. Abbreviations: Alve., alveolar; Art., articular; Car., carotid; Condy., condyle; Fiss., fissure; For., foramen; Inf., inferior; Infratemp., infratemporal; IOF., inferior orbital fissure; Lac., Lacerum; Lat., lateral; Mand., mandible; Med., medial; Obl., oblique; Palatomax., palatomaxillary; Ptery., pterygoid; Pterygomax., pterygomaxillary; Petrotym., petrotympanic; Pyra. Proc., pyramidal process; Scaph., scaphoid; SOF., superior orbital fissure; Sph., sphenoid; Spin., spinosum; Squam., squamous; Stylo., styloid; Submand., submandibular; Sul., sulcus; Temp., temporal; Tym., tympanic. (Images courtesy of AL Rhoton, Jr.)
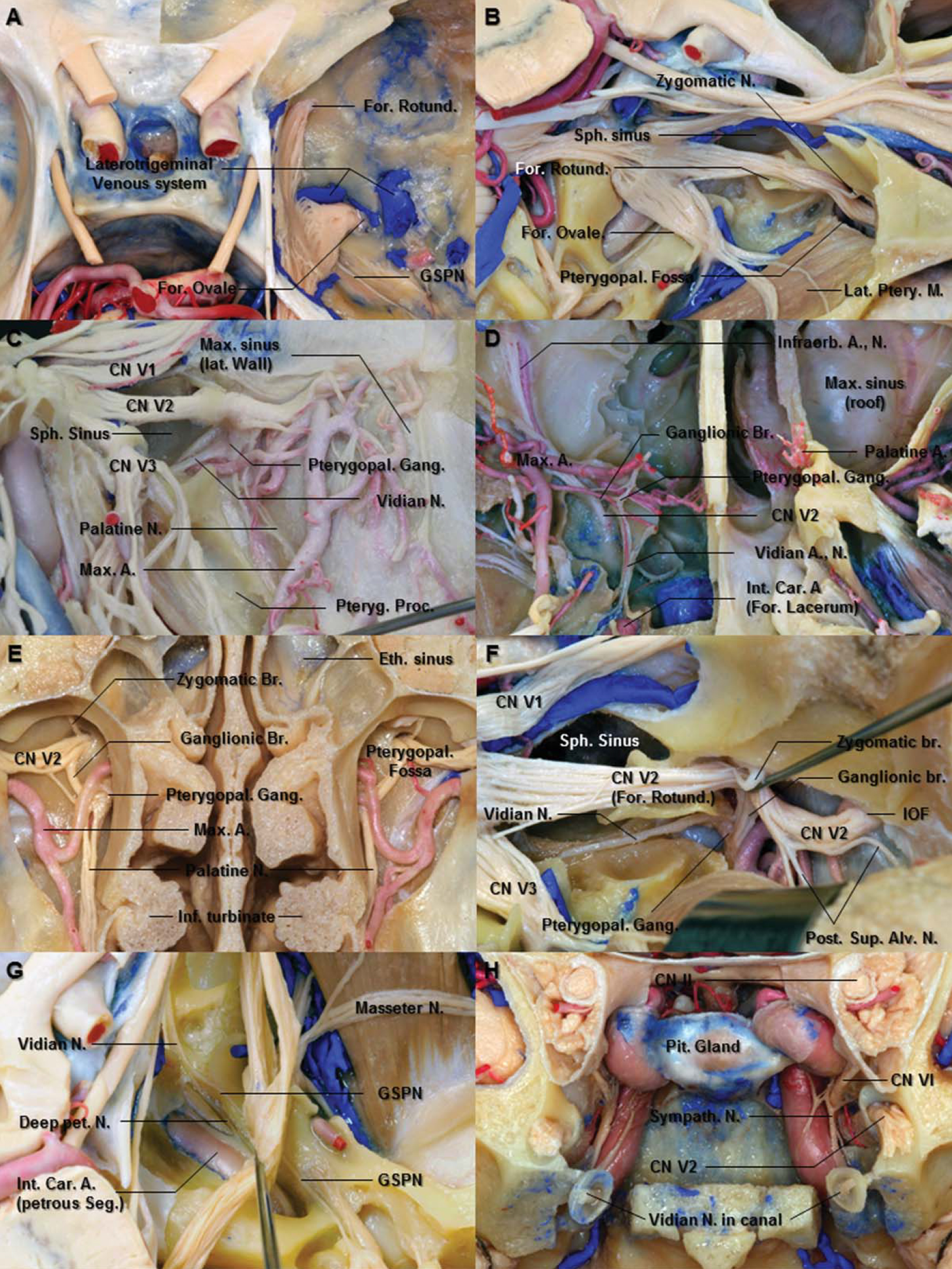
Figure 8. A. Superior view of the middle fossa. The middle fossa dura has been removed to expose the trigeminal nerve. The laterotrigeminal venous system is the venous system surrounding the foramen ovale and mandibular division. B. Superolateral view of the right trigeminal nerve. The bone surrounding the foramen rotundum and ovale has been removed to expose the maxillary and mandibular divisions, respectively. Removing bone in the triangular space between the ophthalmic and maxillary nerve opens into the sphenoid sinus. The maxillary nerve enters the pterygopalatine fossa by passing through the foramen rotundum. C. Lateral view of the right pterygopalatine fossa. The temporal bone, mandibular ramus, and pterygoid muscles have been removed to expose the branches of the maxillary nerve in the pterygopalatine fossa. The vascular structures are anterior to nervous structures in the pterygopalatine fossa. D. Inferior view of the pterygopalatine fossa. The pterygopalatine ganglion is located inferior and medial to the maxillary nerve. The ganglionic branch in the pterygopalatine fossa connects between the maxillary nerve and pterygopalatine ganglion. After crossing the upper part of the pterygopalatine fossa, the maxillary nerve inclines laterally and then enters the infraorbital groove and canal. E. Cross section through the ethmoidal and maxillary sinuses and the nasal cavity in front of the posterior maxillary wall. The posterior wall of the maxillary sinus has been removed to expose the pterygopalatine fossa and ganglion. The maxillary arteries enter the pterygopalatine fossa from the laterally by passing through the pterygomaxillary fissure and give rise to its terminal branches in the pterygopalatine fossa. F. Lateral view of the right pterygopalatine fossa. The maxillary nerve is situated superior and lateral to the pterygopalatine ganglion. The vidian nerve, which courses the floor of the sphenoid sinus, is inferomedial to the maxillary nerve and joins the pterygopalatine ganglion. The maxillary nerve also gives rise to the zygomatic and the posterior superior alveolar nerves. G. The trigeminal nerve has been reflected laterally to expose the vidian nerve. The vidian nerve is formed by the union of the GSPN and deep petrosal nerve. H. Coronal section through the orbital apex behind the pterygopalatine fossa. The anterior end of vidian canal, which opens into the medial part of the posterior wall of the pterygopalatine fossa, is funnel shaped. Abbreviations: A., artery; Alv., alveolar; Br., Branch; Car., carotid; CN., cranial nerve; Eth., ethmoid; For., foramen; Gang., ganglion; GSPN., greater superficial petrosal nerve; Inf., inferior; Infraorb., infraorbital; Int., internal; IOF., inferior orbital fissure; Lat., lateral; M., muscle; Max., maxillary; N., nerve; Pet., petrosal; Pit., pituitary; Post., posterior; Proc., process; Ptery., pterygoid; pterygopal., pterygopalatine; Rotund., rotundum; Seg., segment; Sph., sphenoid; Sup., superior; Sympath., sympathetic. (Images courtesy of AL Rhoton, Jr.)
The V2, after entering the PPF, gives off ganglionic branches to the PPG. It then deviates laterally just beneath the inferior orbital fissure, giving rise to zygomatic and posterosuperior alveolar nerves outside of the periorbita. The V2 then turns medially as the infraorbital nerve, passing through the inferior orbital fissure to enter the infraorbital groove, where the anterior and middle superior alveolar nerves arise (Figs. 8B, 8D, 8E, and 8F).
The branches of the V2 can be divided into four groups corresponding to their origins, as follows: in the cranium, the pterygopalatine fossa, the infraorbital canal, and on the face.
In the Cranium
Meningeal nerve. The meningeal nerve arises from the V2 within the middle cranial fossa near the foramen rotundum. It receives a ramus from the internal carotid sympathetic plexus and accompanies the frontal branch of the middle meningeal artery to supply the dura mater in the middle cranial fossa. Its anterior small branches just reach the anterior cranial fossa. This is the smallest branch of the V2 (Gray and Williams, 1989b; Shankland, 2001b).
In the Pterygopalatine Fossa
Ganglionic branches. The ganglionic branches in the pterygopalatine fossa (PPF) connect the V2 to the PPG. The pterygopalatine ganglion (PPG) is located inferior and medial to the maxillary nerve (V2) (Figs. 8C–8F). The ganglionic branches contain postganglionic parasympathetic nerve fibers to the lacrimal gland, which join the V2 and pass into its zygomaticotemporal nerve, and reach the lacrimal gland via the communication between the zygomaticotemporal nerve and lacrimal nerve (Fig. 1D). They also contain sensory fibers from the orbital periosteum and the mucosa of the nose, palate, and pharynx (Gray and Williams, 1989b).
Zygomatic nerve. The zygomatic nerve arises from the V2 in the PPF, passes anteriorly, superiorly, and laterally to enter the orbit through the inferior orbital fissure. It runs along the lateral wall of the orbit and divides into zygomaticotemporal and zygomaticofacial nerves (Fig. 8B and 9C).
Figure 9. A. Enlarged anterior oblique view of the pterygopalatine fossa. The pterygopalatine ganglion receives communicating rami from the maxillary nerve. The sphenopalatine branch passes through the sphenopalatine foramen to enter the lateral nasal cavity. B. The terminal branch of the maxillary artery and nasal branches arising from the pterygopalatine ganglion penetrate the lateral wall of the nasal cavity to course along the sphenoid face. C. Anterosuperior view of the orbit. The maxillary nerve gives rise to the infraorbital, zygomatic, and superior alveolar nerves. The anterior wall of the pterygopalatine fossa is formed by the posterior wall of the maxillary sinus. D. Anterosuperior view of the maxilla. The maxillary nerve enters the infraorbital groove and canal by passing through the inferior orbital fissure and continues as the infraorbital nerve. The infraorbital nerve emerges in the face through the infraorbital foramen. E. The posterior wall of the right maxillary sinus has been removed to expose the pterygopalatine fossa. The maxillary artery is located anterior to the pterygopalatine ganglion. The palatine nerves descend through the palatine foramina of the maxilla located at the inferior tip of the pterygopalatine fossa. F. The right buccolabial muscles have been removed to expose the branches of the infraorbital nerve. The branches of the infraorbital nerve communicate with the branches of the facial nerve to form infraorbital plexus in the infraorbital space. G. The branches of the infraorbital nerve have been removed. The infraorbital nerve gives rise to anterior superior alveolar nerve just behind the infraorbital exit through the foramen. Abbreviations: A., artery; Alv., alveolar; Ant., anterior; Br., branch; CN., cranial nerve; For., foramen; Gr., great; Inf., inferior; Infraorb., infraorbital; Max., maxillary; N., nerve; Pit., pituitary; Post., posterior; Pterygopal., pterygopalatine; Rotund., rotundum; SOF., superior orbital fissure; Sph., sphenoid; Sphenopal., sphenopalatine; Sup., superior; Temp., temporal; Zygo., zygomatic. (Images courtesy of AL Rhoton, Jr.)
Zygomaticotemporal nerve. The zygomaticotemporal nerve passes along the inferolateral angle of the orbit, gives off the communicating branch to the lacrimal nerve of the V1, traverses a bony canal in the zygomatic bone, and enters into the temporal fossa. It then ascends between the bone and the temporalis muscle and pierces the deep temporal fascia approximately 2 cm above the zygomatic arch to innervate the skin of the temporal area (Totonchi et al., 2005). Sometimes, when the lacrimal nerve is lacking, the zygomaticotemporal nerve becomes its replacement and innervates the lacrimal gland (Shankland, 2001b).
Zygomaticofacial nerve. The zygomaticofacial nerve also courses the inferolateral angle of the orbit, emerging on the face through a zygomaticofacial foramen in the zygomatic bone, and supplies the skin on the prominence of the cheek. It forms a plexus with zygomatic branches of the facial nerve and palpebral branches of the V2.
Posterior superior alveolar nerves. The posterior superior alveolar nerve arises from the maxillary nerve before penetrating into the infraorbital canal in the PPF and descends anteriorly and inferiorly to pierce the infratemporal surface of the maxillary sinus (Figs. 8C and 8F). After entering the maxillary sinus, the nerves pass forward under the mucosa of the maxillary sinus, supplying afferent innervation to these membranes. The number of posterior superior alveolar nerves that originate from the V2 in the zygomatic region can vary from one to three (Moretto et al., 2005). The posterior superior alveolar nerves communicate with the middle superior alveolar nerve and give branches which form a dental plexus (Shankland, 2001b). It also supplies a branch to the upper gum and the adjoining part of the cheek (Gray and Williams, 1989b).
Pterygopalatine ganglion. The pterygopalatine ganglion (PPG), the largest of the peripheral parasympathetic ganglia, is located deeply in the PPF, near the sphenopalatine foramen and anterior to pterygoid canal, and associated with the V2. The ganglion receives communicating rami from the V2 (ganglionic branches) superolaterally and vidian nerve superomedially and gives rise to the greater and lesser palatine nerves from the lower surface of the ganglion, sphenopalatine nerve, and pharyngeal branch from the medial surface and the orbital branch from the superior surface (Figs. 8C–8F, 9A, and 9B). The vidian nerve is formed by the union of the greater petrosal nerve, which conveys parasympathetic fibers arising from the facial nerve (nerve intermedius) at the level of the geniculate ganglion, and deep petrosal nerve, which conveys sympathetic fibers from the carotid plexus, to reach the lacrimal gland and nasal mucosa (Figs. 1D, 8G, and 9A).
Palatine nerves. The palatine nerves are distributed to the roof of the mouth, the soft palate, tonsil, and the nasal mucosa. They also convey taste impulses from the palate via the PPG and vidian nerve to the nervus intermedius of the facial nerve, which terminates to the solitary tract and nucleus of the brain stem (Fig. 1D). The greater palatine nerve descends through the greater palatine foramen of the maxilla located at the inferior tip of the PPF and runs forward in a groove on the inferior surface of the hard palate (Figs. 9A and 9E). It communicates with the filaments of the nasopalatine nerve, a branch of the sphenopalatine nerve. The thickest nerves connecting the PPG were invariably the sphenopalatine nerve and greater palatine nerve (Rusu et al., 2009).
The lesser palatine nerves, after leaving the PPG, descend through a lesser palatine foramen in the palatine bone and give branches to the uvula, tonsil, and soft palate. These nerves anastomose with branches of the glossopharyngeal nerve to form a tonsillar plexus around the palatine tonsil (Fig. 9E) (Shankland, 2001b).
Vidian nerve. The vidian canal connects the PPF and the foramen lacerum. It conveys the vidian nerve, artery, and vein and contains adipose tissue. The anterior opening of the vidian canal is located inferomedial to the foramen rotundum in the posterior wall of the PPF (Fig. 8D). The canal is a straight to slightly curved pathway directed posterolaterally from its anterior opening (Figs. 8D and 8H) (Kim et al., 1996). The canal sits just below the floor of the well-pneumatized sphenoid sinus (Figs. 8D and 8F). The posterior opening is located above the posterior edge of the medial pterygoid plate. It opens posteriorly into the upper part of the anterolateral edge to the foramen lacerum (Fig. 8D). The posterior opening of the vidian canal is situated 6.9 mm (range, 4.8–9.1 mm) medial to the medial edge of the foramen ovale and V3 (Rahman et al., 2009).
Although the vidian nerve, formed by the union of the greater and deep petrosal nerves, is not the branch of the V2, it enters and passes through the vidian canal and ends in the PPG, which is positioned in front to the anterior opening of the vidian canal (Fig. 8G). The greater petrosal nerve (GSPN) contains taste fibers from the palatal mucosa and preganglionic parasympathetic fibers that arise from the superior salivary nucleus in the brainstem and are conveyed in the nervus intermedius. The postganglionic parasympathetic fibers pass through the V2 and its zygomatic branch to enter orbit through the inferior orbital fissure and reach the lacrimal gland through a communication with the lacrimal branch of the ophthalmic nerve (Fig. 1D) (Gray and Williams, 1989b; Rhoton, 2003b; Rahman et al., 2009). The deep petrosal nerve contains postganglionic sympathetic fibers that arise in the superior cervical ganglion and travel upward in the nerve plexus on the internal carotid artery. Therefore, the vidian nerve contains sensory, sympathetic, and parasympathetic fibers. The parasympathetic fibers synapse in the PPG, however, the sensory and the sympathetic fibers pass through the ganglion without synapse (Gray and Williams, 1989b; el Shazly, 1991; Rahman et al., 2009).
The vidian canal and nerve have become important landmarks in directing the microsurgical and endoscopic approaches along the floor of the sphenoid sinus to the petrous carotid and the anteromedial part of the cavernous sinus and Meckel’s cave (Figs. 8G and 9B) (Rahman et al., 2009).
Nasal branches. The nasal branches enter the nasal cavity through the sphenopalatine foramen in the lateral wall of the nasal cavity. These branches include medial and lateral posterior superior nasal nerves and nasopalatine nerves (Fig. 9B). Lateral posterior superior nasal nerves. The lateral posterior superior nasal branches, usually six in number, innervate the mucosa of the posterior part of the superior and middle nasal conchae and the lining of the posterior ethmoidal sinuses (Gray and Williams, 1989b).
Medial posterior superior nasal nerves. The medial posterior superior nasal branches, usually two to three in number, cross the nasal roof below the opening of the sphenoidal sinus to supply the mucosa of the posterior part of the roof and of the nasal septum (Gray and Williams, 1989b).
Nasopalatine nerve. The nasopalatine nerve, the largest nerve of the nasal branches of the PPG, travels through the sphenopalatine foramen to enter the nasal cavity just below the orifice to the sphenoid sinus to reach the nasal septum. It then runs anteroinferiorly between the periosteum and mucous membrane of the nasal septum, supplies a few filaments to the nasal septum, exits the nasal cavity through the incisive foramen, and ends by supplying the mucosa of the anterior part of the hard palate, there communicating with the greater palatine nerves (Gray and Williams, 1989b; Shankland, 2001b).
Pharyngeal nerve. The pharyngeal nerve arises from the posterior part of the PPG, traverses the palatovaginal canal with a pharyngeal branch of the maxillary artery, and supplies the mucosa of the nasopharynx behind the auditory tube. The palatovaginal canal is a short bone tunnel formed by the application of the sphenoid process of the palatine bone to the vaginal process of the sphenoid bone (Figs. 7B and 11B) (Wentges, 1975). The palatovaginal canal is located medial and inferior to the vidian canal. The palatovaginal canal is found inferomedially on the posterior wall of the PPF, in the roof of the nasopharynx.
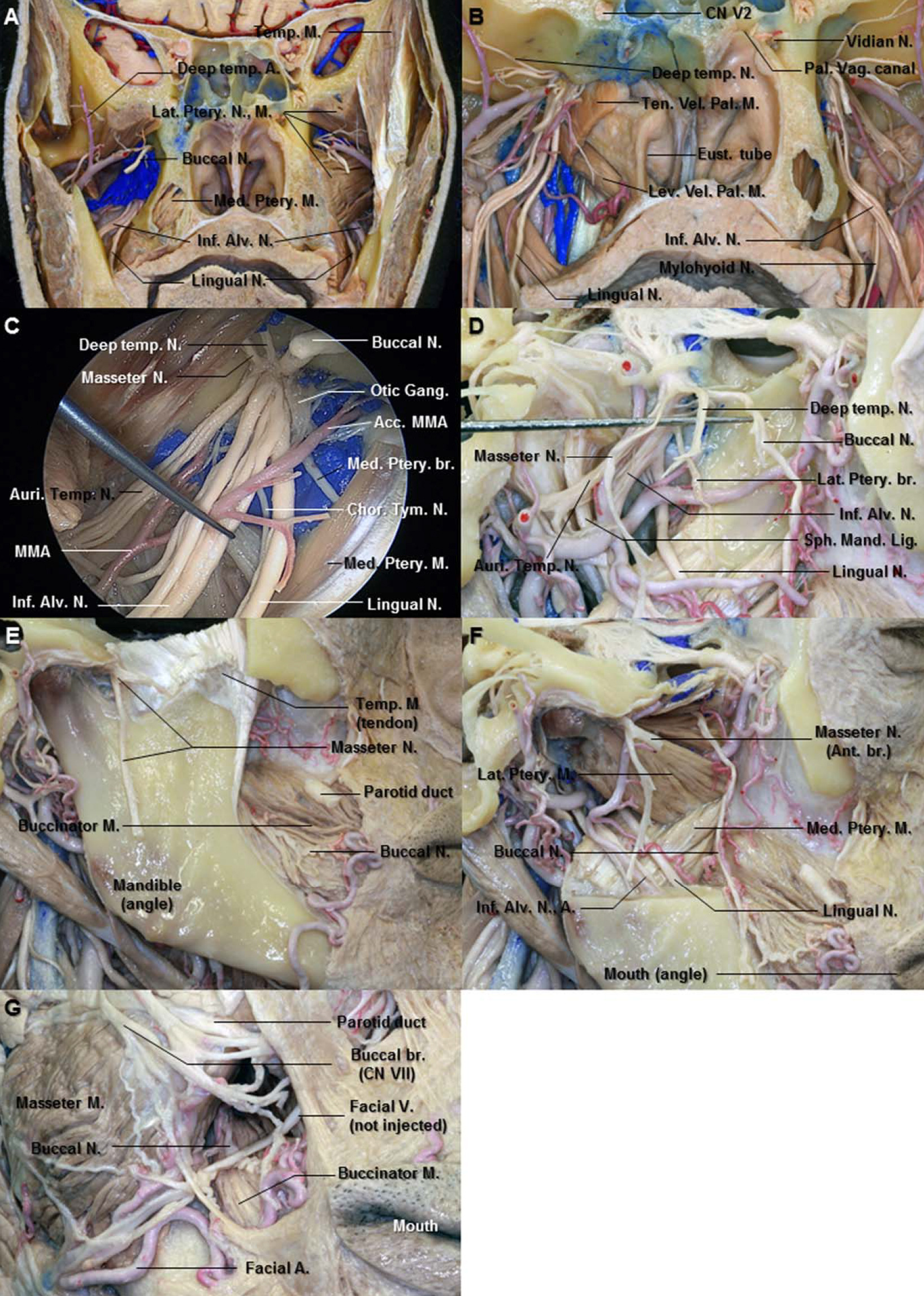
Figure 10. A. Superolateral view of the right infratemporal fossa. The middle fossa floor has been removed to expose the branches of the mandibular nerve. The masseteric and deep temporal nerves pass above the pterygoid venous plexus and the upper head of the lateral pterygoid muscle. B. The mandibular ramus has been removed to pterygoid muscles. The buccal nerve passes anterolaterally between the upper and lower heads of the lateral pterygoid muscles. C. The mandibular condyle and the lateral pterygoid muscle have been reflected anteriorly to expose the branches of the maxillary artery and mandibular nerve. The auriculotemporal nerve runs backward medial to the lateral pterygoid muscle to the neck of the mandible. The middle meningeal artery passes between the two roots of the auriculotemporal nerve. D. Enlarged view of the branches of the mandibular nerve. The anterior division of the mandibular nerve passes in the horizontal plane just below the pericranium of the infratemporal surface of the middle cranial fossa. The chorda tympani nerve enters the infratemporal fossa through the petrotympanic fissure, descends medial to the auriculotemporal and inferior alveolar nerves, and joins the lingual nerve. E. The lateral pterygoid muscle has been removed to pterygoid nerves. The medial pterygoid nerve originates from the medial aspect of the main trunk below the foramen ovale close to the otic ganglion. The tensor veli palatini muscle is located medial to the branches of the mandibular nerve. F. The lesser petrosal nerve emerging through the roof of the tympanic cavity of the temporal bone passes along the tensor tympani muscle anterolaterally to enter the otic ganglion. Abbreviations: A., artery; Acc., accessory; Alv., alveolar; Auri. Temp. N., auriculotemporal nerve; Br., branch; Chor.Tym. N., chorda tympani nerve; CN., cranial nerve; For., foramen; GSPN., greater superficial petrosal nerve; Inf., inferior; Lat., lateral; LSPN., lesser superficial petrosal nerve; M., muscle; Max., maxillary; Med., medial; MMA., middle meningeal artery; N., nerve; Plex., plexus; Ptery., pterygoid; Spin., spinosum; Sph. Mand. Lig., sphenomandibular ligament; Supf., superficial; Temp., temporal; Ten. Tym. M., tensor tympani muscle; Ten. Vel. Pal. M., tensor veli palatini muscle. (Images courtesy of AL Rhoton, Jr.)
Figure 11. A. Coronal section just behind the pterygopalatine fossa. The right lateral pterygoid muscle has been removed from the pterygoid venous plexus and posterior division of the mandibular nerve. The nerve to the lateral pterygoid muscle originates from the buccal nerve passing between the two heads of the lateral pterygoid. B. The right pterygoid venous plexus and pterygoid plates have been removed to expose the branches of the mandibular nerve. The posterior division of the mandibular nerve descends between the lateral pterygoid muscle (removed) and tensor veli palatini muscle (cut). The palatovaginal canal is located media to the vidian canal. C. Enlarged view of the proximal portion of the right mandibular nerve. The nerve to the medial pterygoid muscle arises from the medial aspect of the mandibular nerve close to the otic ganglion. D. Lateral view of the right infratemporal fossa. The mandibular ramus and lateral pterygoid muscle have been removed. The buccal, deep temporal, and masseter nerves have been elevated with the dissector. This division passes in the horizontal plane. The auriculotemporal nerve passes backward between the sphenomandibular ligament and the ramus of the mandible (removed). E. The masseter muscle has been removed from the mandible to expose the masseter nerve. The masseter nerve passes laterally above the lateral pterygoid muscle in front of the temporomandibular joint and behind the tendon of the temporal muscle. It runs to the deep surface of the master muscle. F. The mandibular ramus has been removed to expose the lingual and the inferior alveolar nerves. G. Anterior view of the right cheek. The buccal nerve emerges from the undersurface of the ramus of mandible and unites with the buccal branches of the facial nerve. Abbreviations: Acc. MMA., Accessory middle meningeal artery; Ant., anterior; Alv., alveolar; Auri. Temp. N., auriculotemporal nerve; Br., branch; Chor.-Tym. N., chorda tympani nerve; CN., cranial nerve; Eust., Eustachian; Gang., ganglion; Inf., inferior; Lat., lateral; Lev. Vel. Pal. M., levator veli palatini muscle; M., muscle; Med., medial; N., nerve; Pal. Vag., palatovaginal; Sph. Mand. Lig., sphenomandibular ligament; Temp., temporal; Ten. Vel. Pal. M., tensor veli palatini muscle. (Images courtesy of AL Rhoton, Jr.)
In the infraorbital canal. After crossing the upper part of the PPF, the maxillary nerve (V2) inclines laterally and then enters the infraorbital groove and canal and continues as the infraorbital nerve (ION) (Figs. 8B and 8D). The average lengths of the groove and canal were 12 mm (range, 5–22 mm) and 14 mm (range, 7–22 mm), respectively (Rahman et al., 2009). The long axis of the infraorbital canal is directed downward and medially across the face (Fig. 9D). The ION runs in its canal lying progressively below the floor of the orbit, in the roof of the maxillary sinus, until it emerges in the face through the infraorbital foramen located below the inferior orbital rim. The ION branches into middle and anterior superior alveolar nerves within the infraorbital canal (Fig. 9F).
Middle superior alveolar nerve. The middle superior alveolar nerve leaves the ION in the infraorbital groove, the posterior part of the infraorbital canal (Fig. 9C). It runs down and forward in the lateral wall of the maxillary sinus and ends in small branches which link up with the superior dental plexus, supplying small rami to the upper premolar teeth. The middle superior alveolar also anastomoses with the posterior superior alveolar nerve (Shankland, 2001b).
Anterior superior alveolar nerve. The anterior superior alveolar nerve, being larger than middle superior alveolar nerve, leaves the lateral side of the ION just prior to the infraorbital exit through the foramen (Fig. 9G). It traverses the canal in the anterior wall of maxillary sinus and divides into branches supplying incisor and canine teeth. It communicates with middle alveolar nerve to form the superior dental plexus and gives rise to nasal branch, which passes through a small canal in the lateral wall of the inferior meatus to supply the mucous membrane of the anterior area of the lateral wall and the floor of the nasal cavity (Gray and Williams, 1989b; Shankland, 2001b).
On the face. The infraorbital nerve (ION), an entirely sensory nerve, is the terminal branch of the maxillary nerve (V2). When it emerges onto the face through the infraorbital foramen, which is normally located within 1 cm of the inferior border of the orbital rim, the ION divides into the inferior palpebral, internal and external nasal, and superior labial branches, which supply skin and conjunctiva of the inferior eyelid, lateral part of the nose, and the skin and mucosa of the upper lip (Figs. 9D and 9F) (Gray and Williams, 1989b; Moore and Dalley, 1999; Hu et al., 2006).
When the ION emerges from the infraorbital foramen, three branches except for the inferior palpebral branch run downward. The infraorbital space is placed inferior to the infraorbital foramen and here the ION that travels downward and the facial nerve that travels transversely form the infraorbital plexus (Fig. 9F) (Hu et al., 2006).
Inferior palpebral branches. The inferior palpebral branches, usually two or three in number, ascend deep into the orbicularis oculi muscle, piercing the muscle to supply the skin and conjunctiva of the lower eyelid. These nerves communicate with the facial and zygomaticofacial nerves near the lateral canthus (Fig. 9F).
Nasal branches. The external nasal branch innervates the skin of the lateral surface of the nose. The internal nasal branch emerged through the medial portion of the infraorbital foramen and descended down the face along the nose and around the ala of the nose (Fig. 9F). Finally, it supplied the nasal septum and vestibule of the nose. The nasal branches join with external branches of the anterior ethmoidal nerve (Gray and Williams, 1989b; Hu et al., 2006).
Superior labial branches. The superior labial branches, large and numerous, descend posterior to the levator labii superior muscle to supply the skin of the anterior part of the cheek, upper lip, oral mucosa, and labial gland and are joined by zygomatic branch of the facial nerve to form the infraorbital plexus (Fig. 9F) (Gray and Williams, 1989b).
Mandibular Division
The mandibular division (V3) is the largest of the three divisions of the trigeminal nerve. It supplies the teeth, gums of the mandible, the skin in the temporal region, part of the auricle, the lower lip, and the lower part of the face. However, unlike the ophthalmic (V1) and maxillary (V2) divisions which convey purely afferent fibers, the V3 also contains motor or efferent fiber to innervate the muscle that are attached to mandible, including the muscle of mastication, the mylohyoid, the anterior belly of the digastric muscle, tensor veli palatini, and tensor tympani muscle.
The V3, which is the largest division of the trigeminal nerve, is made up of two roots: a large, sensory root, which proceeds from the lateral part of the trigeminal ganglion and emerges almost immediately through the foramen ovale of the sphenoid bone and a small motor root arising around the superomedial part of the main sensory root in the pons that passes below the trigeminal ganglion and unites with the sensory root just outside the foramen ovale (Figs. 2B, 2C, and 5D). The V3 exits the middle fossa through the foramen ovale to enter the infratemporal fossa and medial to the lateral pterygoid muscle where the main trunk divides into a small anterior division and a large posterior division (Figs. 10A–10C).
The infratemporal fossa is a deep-seated space below the infratemporal crest, which continues superiorly to the temporal fossa including the temporal muscle and inferiorly to parapharyngeal space. The osseous boundaries of the infratemporal fossa are the posterolateral maxillary surface anteriorly, the lateral pterygoid plate anteromedially, the mandibular ramus laterally, and the tympanic part of the temporal bone and the styloid process posteriorly (Figs. 7C and 7D). This fossa contains the maxillary artery, the mandibular branch (V3) of the trigeminal nerve, the pterygoid muscles, and the pterygoid venous plexus (Figs. 10A, 10B, 11A, and 11C). Topographically, the mandibular division is located intimately to the lateral pterygoid muscle and some mandibular nerve branches pass through the lateral pterygoid muscle (Figs. 10A and 10B).
Undivided trunk. The small motor root originates in the pons, passes below the trigeminal ganglion, and unites with the large sensory root just outside the foramen ovale, where main trunk of the V3 lies between the tensor veli palatini medially and the lateral pterygoid muscle laterally (Figs. 10C, 10E, and 11B). Immediately beyond the junction of the two roots, the main trunk (V3) gives rise to the meningeal branch and the nerve to the medial pterygoid muscle from the medial aspect and then divides into a smaller anterior trunk and a larger posterior trunk (Fig. 10E).
Meningeal branch. The meningeal branch, a nervous spinosus, arises near the otic ganglion and ascends through the foramen spinosum with the middle meningeal artery to innervate the middle cranial fossa dura. It divides into anterior and posterior branches, which accompany the main division of the artery. The nervous spinosus contains sympathetic postganglionic fibers from the middle meningeal plexus (Gray and Williams, 1989b).
Medial pterygoid nerve. The medial pterygoid nerve arises from the medial aspect of the main trunk below the foramen ovale close to the otic ganglion and descends to supply the medial pterygoid muscle (Figs. 10E and 11C). It contains sensory, motor, and proprioceptive fiber of the medial pterygoid muscle.
Tensor veli palatini nerve. The nerve to the tensor veli palatini arises from the medial aspect of the main trunk like the medial pterygoid nerve. It passes through otic ganglion to innervate the tensor veli palatini near its origin at the base of the medial pterygoid plate of the sphenoid bone (Shankland, 2001c).
Tensor tympani nerve. The nerve to the tensor tympani may arise separately or in common with the tensor veli palatini nerve from the undivided main trunk. It passes through the otic ganglion without interruption. The nerve pierces the cartilage of the auditory tube to enter the tensor tympani muscle (Kierner et al., 2003; Shankland, 2001c).
Otic ganglion. The otic ganglion is a small, oval, flat, and reddish gray ganglion situated immediately below the foramen ovale (Fig. 11C). It lies on the medial surface of the mandibular undivided trunk near the origin of the medial pterygoid and tensor veli palatini nerves. This ganglion is a peripheral parasympathetic ganglion intimately related topographically to the mandibular nerve but functionally connected with the glossopharyngeal nerve (Fig. 1D). The preganglionic parasympathetic fibers leave the inferior salivary nucleus of the glossopharyngeal nerve in the brain stem. It enters the tympanic branch, which passes through a small canal in the carotid ridge between the jugular foramen and carotid canal to reach the tympanic cavity, passes through the tympanic plexus and emerges through the roof of the tympanic cavity of the temporal bone as the lesser superficial petrosal nerve (LSPN). The LSPN proceeds to the otic ganglion (Figs. 10D and 10F).
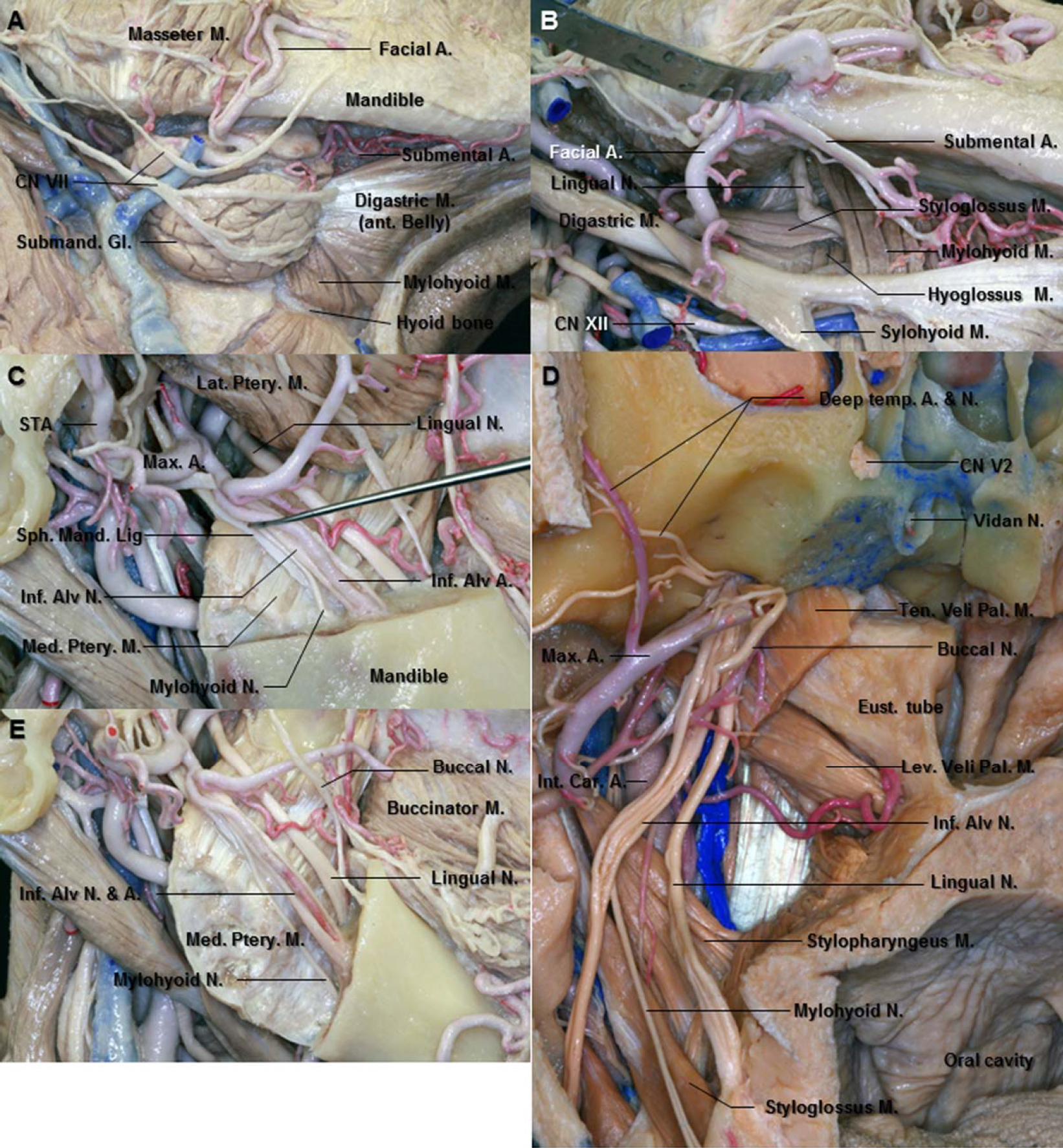
After synapsing on cell in the ganglion, postganglionic parasympathetic secretomotor fibers reach to the parotid gland via the auriculotemporal nerve (Figs. 10C, 12C, and 12D). The sympathetic root arises from the plexus on the middle meningeal artery. It contains postganglionic fibers from the superior cervical sympathetic ganglion, which traverse the otic ganglion without synapse. The sympathetic fiber supplies the blood vessels in the parotid gland (Shankland, 2000).
Figure 12. A. Superior view after removing the bone of middle fossa. The posterior deep temporal nerve runs on the superior surface of the superior head of the lateral pterygoid muscle. The masseter nerve is the most posterior branch among the anterior division of the mandibular nerve. B. The squamous portion of the temporal bone has removed to expose deep surface of the temporal muscle. The anterior deep temporal nerve passes between the superior and inferior heads of the lateral pterygoid muscle. The deep temporal nerves enter the deep surface of the anterior portion of the temporal muscle. C. Enlarged view of the right infratemporal fossa. The middle meningeal artery passes between the two roots of the auriculotemporal nerve. The auriculotemporal nerve runs medial to lateral behind the neck of the mandible. D. Lateral view of the right mandibular neck area. The parotid gland has removed to expose the auriculotemporal and facial nerves. The auriculotemporal nerve gives off the parotid branches and ascends in the parotid gland between the temporomandibular joint and external acoustic meatus. It communicates with facial nerve at the posterior border of the mandibular ramus. E. Lateral view of the right preauricular area. The auriculotemporal nerve ascends posterior to the superficial temporal artery over the posterior root of zygoma. The frontal branches of the facial nerve pass over the zygomatic arch. Abbreviations: A., artery; Ac., acoustic; Ant., anterior; Auri. Temp. N., auriculotemporal nerve; Br., branch; Ext., external; Gang., ganglion; Gl., gland; Inf. Alv. N., inferior alveolar nerve; Lat., lateral; M., muscle; Mand. For., mandibular foramen; Max., maxillary; Med., medial; N., nerve; Post., posterior; Post. Auri. A., posterior auricular artery; Ptery., pterygoid; STA., superficial temporal artery; Sup., superior; Temp., temporal; Tr., trunk. (Images courtesy of AL Rhoton, Jr.)
Anterior division. The V3 divides into the anterior smaller and the posterior larger divisions in the infratemporal fossa. The average distance of the undivided trunk from the foramen ovale to the bifurcation of the V3 was approximately 7.7 mm (range, 5–12 mm) (Vrionis et al., 1996). The smaller anterior division gives rise to the sensory buccal nerve and the motor branches: masseteric nerve, deep temporal nerves, and nerve to the lateral pterygoid muscle. This division passes in the horizontal plane just below the pericranium of the infratemporal surface of the middle cranial fossa (Fig. 10A).
Buccal nerve. The sensory buccal nerve passes anterolaterally between the two heads of the lateral pterygoid, below the inferior portion of the temporal muscle, and deep to the mandible and the masseter muscle (Figs. 10A, 10B, and 11A). Its course is directed between the coronoid process and tuberosity of the maxilla. It emerges from the undersurface of the ramus of the mandible and the anterior border of the masseter muscle and unites with the buccal branches of the facial nerve (Figs. 11E–11G) (Gray and Williams, 1989b). The buccal nerve conveys sensory innervation to the buccinators muscle, buccal mucosa, and the skin of the corner of the mouth. It normally pierces the posterior half of the buccinators muscle to arborize extensively on the buccal surface of the cheek (Tubbs et al., 2010). However, some authors reported that the buccal nerve was a mixed nerve, which provide the branches to the lateral pterygoid muscle and temporal muscle (Kim et al., 2003; Piagkou et al., 2011; Davies et al., 2012).
The buccal nerve was found to lie 3 cm lateral to the angle of the mouth (range, 2.8–3.3 cm). It was located 7 mm caudally from the point of entrance of the parotid duct into the buccinators muscle (range, 4–12 mm) (Figs. 11E and 11G) (Tubbs et al., 2010).
Lateral pterygoid nerve. The lateral pterygoid nerve enters the deep surface of the muscle (Figs. 10E and 11D). It is generally described that the nerve to the lateral pterygoid nerve originates mainly from the buccal nerve (Fig. 11A) (Gray and Williams, 1989a; Kim et al., 2003; Piagkou et al., 2011). It is the most inconsistent of all the individual branches of the entire trigeminal nerve (Shankland, 2001c). Foucart et al. (1998) reported that the lateral pterygoid muscle is innervated by one to three branches from the anterior trunk of the mandibular nerve and additionally by branches from the buccal, auriculotemporal, and masseteric nerves (Foucart et al., 1998). However, according to Kim et al. the lateral pterygoid muscle was observed to be innervated not only by the buccal nerve but also by the deep temporal nerves and branches directly from the mandibular nerve trunk. The nerve branches arising from the auriculotemporal or masseteric nerve did not innervate the lateral pterygoid muscle (Kim et al., 2003).
Masseter nerve. The masseteric nerve passes laterally above the lateral pterygoid muscle in front of the temporomandibular joint and behind the tendon of the temporal muscle (Fig. 10A). It crosses the posterior part of the mandibular notch with the masseteric artery and runs to the deep surface of the masseter muscle (Figs. 11D and 11E). The masseteric nerve gives off anterior and posterior branches in the short masseter muscle. The anterior branch is larger and longer than the posterior one (Figs. 11E and 11F) (Hwang et al., 2005). The masseteric nerve is the most posterior branch among the anterior division of the V3 (Figs. 10A and 11D).
The motor nerve to the masseter was found 3.16 ± 0.30 cm anterior to the tragus and 1.08 ± 0.18 cm inferior to the caudal edge of the zygomatic arch. Relative to the zygomatic arch, the nerve formed an angle of 50 ± 7.6° as it coursed distally into the masseter muscle (Borschel et al., 2012).
Deep temporal nerves. The anterior and posterior branches of the nerves usually pass above the lateral pterygoid muscle to enter the deep surface of the temporalis muscle (Fig. 10A) (Gray and Williams, 1989a). Kwak et al. reported that the anterior deep temporal nerve passes between the superior and inferior heads of the lateral pterygoid muscle, courses anteriorly in the infratemporal fossa, and then turns superiorly, passing into the temporal fossa on the lateral aspect of the skull to enter the deep surface of the anterior portion of the temporal muscle. The posterior deep temporal nerves ran on the superior surface of the superior head and distributed into the posterior portion of the temporalis muscle (Figs. 12A and 12B). In all specimens, the anterior deep temporal nerve arose from the buccal nerve, being one or two in number (Fig. 12B) (Kwak et al., 2003; Shankland, 2001c). The posterior branch, generally two or three in number, arises in common with the masseteric nerves (Akita et al., 2000; Gray and Williams, 1989a).
Posterior division. The large posterior division of the V3 is mainly sensory but receives a few filaments from the motor root. It divides into three main branches: the auriculotemporal nerve, the inferior alveolar nerve, and the lingual nerve which descend in the sagittal plane toward the lower face structures (Figs. 10C, 10D, and 11D).
Auriculotemporal nerve. The auriculotemporal nerve originates from the posterior trunk of the V3 primarily in two branches and the middle meningeal artery passes between them (Gray and Williams, 1989b; Joo et al., 2013; Schmidt et al., 1998). Encircling the middle meningeal artery, these roots join and run backward deep to the lateral pterygoid muscle on the surface of the tensor veli palatini to pass between the sphenomandibular ligament and the neck of the mandible (Figs. 10C, 10D, 11C, and 11D). However, Gülekon et al. (2005) reported that single root of the auriculotemporal nerve in 16 specimens (50%), two roots in 12 specimens (37.5%), three roots in 3 specimens (9.4%), and four roots in 1 specimen (3.1%) were detected in 32 infratemporal fossa of 16 cadaveric heads (Gülekon et al., 2005).
The auriculotemporal nerve runs medial to lateral behind the neck of the mandible, gives off parotid branches, and changes its direction upward in the parotid gland between the temporomandibular joint and the external acoustic meatus (Fig. 12D). Emerging from behind the joint, it ascends posterior to the superficial temporal vessels, over the posterior root of the zygoma, and divides into superficial temporal branches (Figs. 12D and 12E). The nerve was always found to be lateral to the superficial temporal artery in the upper preauricular region of the temple in the dissections of 25 fresh cadaveric heads (Janis et al., 2010).
The auriculotemporal nerve contains somatosensory and secretomotor fibers of CN V3 and CN IX (Loughner et al., 1990). It conveys secretomotor fibers to the parotid gland. The preganglionic parasympathetic fibers leave the glossopharyngeal nerve by way of its tympanic branch to join the tympanic plexus on the promontory of the middle ear cavity, subsequently leaving the plexus through the lesser petrosal nerve; this nerve ends in the otic ganglion, where the preganglionic fibers make synapse (Fig. 1D). The otic ganglion lies just outside the foramen ovale on the medial surface of the mandibular nerve and gives off filaments to the roots by which the auriculotemporal nerve arises from the mandibular nerve; these fibers then leave the auriculotemporal nerve with sensory fibers to form the parotid branches of this nerve and reach the gland. The auriculotemporal nerve is also closely associated with the facial nerve. It communicates with the facial nerve at the posterior border of the mandibular ramus where the auriculotemporal nerve passes posterior to the neck of the condyle and facial nerve divides into two major branches in the parotid gland after exiting the stylomastoid foramen (Fig. 12D). Occasionally, connecting branches may be seen between the auriculotemporal and inferior alveolar nerves in the temporomandibular region (Gülekon et al., 2005; Janis et al., 2010).
Literature review showed that the study of Baumel et al. presents the most comprehensive quantitative data on the variations of the auriculotemporal nerve (Baumel et al., 1971). The lengths of the roots were 15 mm (range, 5–23 mm). The distances between the roots were 6 mm (range, 1–13 mm). The upper root is usually located lateral to the middle meningeal artery and the lower root is located medially (Figs. 10C and 12C) (Baumel et al., 1971).The average length of the posterior trunk from foramen ovale to origin of the upper root of the auriculotemporal nerve was 3.3 mm (range, 1–7.5 mm) (Joo et al., 2013).
Lingual nerve. The lingual nerve is the main branch of the posterior division of V3 that provides sensation to the anterior two-thirds of the tongue and gingiva variably along the lingual side of the mandibular teeth. Within the infratemporal fossa, the lingual nerve arises from the posterior division of V3. The average length of the posterior trunk from the foramen ovale to the bifurcation into lingual and inferior alveolar nerve was 13.5 mm (range, 6–32 mm) (Joo et al., 2013). Shinohara et al. reported that the average distance between the foramen ovale and the bifurcation of lingual and inferior alveolar nerve was 8.7 mm (range, 0–14 mm). They found high bifurcation which consists of the bifurcation of the V3 with the lingual nerve above the foramen ovale (Shinohara et al., 2010). At first, the lingual nerve runs down between the tensor veli palatini and the lateral pterygoid muscles (Figs. 10C, 10D, 11A, and 13D). At the inferior border of the lateral pterygoid, the nerve is joined by the chorda tympani branch of the facial nerve, which contains both sensory fibers from the geniculate ganglion and preganglionic parasympathetic fibers and often by a branch of the inferior alveolar nerve (Figs. 10C, 10F, and 11C). Beyond this point, the lingual nerve contains fibers for general sensation that are true trigeminal nerve fibers, fibers for taste derived from the facial nerve, and autonomic fibers destined for the submandibular ganglion (Fig. 1D) (Hollinshead, 1982b). The lingual nerve courses down and forward between the mandibular ramus and the medial pterygoid, lying anterior and slightly deep to the inferior alveolar nerve, with which it may communicate (Figs. 10B, 10C, and 11B). It then passes inferiorly to the attachment of the superior constrictor at the posterior end of the mylohyoid line, where it is covered only by the gingival mucosa (Benninger et al., 2012). According to some reports, the average distance from the lingual alveolar crest to the lingual nerve was 4.45 mm in the retromolar region (Pogrel et al., 1995), and the average distance in the third molar region was 2.28 mm (Kiesselbach and Chamberlain, 1984). It leaves the gingiva and passes on to the side of the tongue, where it crosses the styloglossus and runs on the lateral surface of the hyoglossus and deep to the mylohyoid, above the deep part of the submandibular gland and its duct (Figs. 13A and 13B). The lingual nerve proceeds forward on the side of the tongue, lateral to the hyoglossus and genioglossus, and divides into terminal branches which lie directly under the lingual mucosa (Gray and Williams, 1989b). The nerve distribution in the tongue is actually more complicated. The nerve fibers are complexly intermingled, and communication between the lingual and the hypoglossal nerve have been reported (Shinohara et al., 2010).
Figure 13. A. Inferolateral view of the right submandibular area. The facial nerves run over the submandibular gland which lie on the digastric tendon. B. Enlarged view of the right submandibular triangle. The submandibular gland has been removed to expose the contents of the submandibular triangle. After passing between the mandibular ramus and the medial pterygoid muscle, the lingual nerve crosses the styloglossus muscle and runs between the hyoglossus and mylohyoid muscles above the deep part of the submandibular gland. C. Lateral view of the right infratemporal fossa. The lingual nerve courses down and forward between the mandibular ramus (removed) and medial pterygoid muscle, lying anterior and slightly deep to the inferior alveolar nerve. The sphenomandibular ligament is a flat, thin band descending from the sphenoidal spine and widening to reach the lingual of the mandibular foramen. D. Anterior view of the right infratemporal fossa. The lingual nerve is anterior and medial to the inferior alveolar nerve. The inferior alveolar nerve gives rise to the mylohyoid nerve before it enters the mandibular foramen. It then emerges in the submandibular triangle and supplies both mylohyoid and anterior belly of the digastric muscles. E. The angle of mandible has been removed. The mylohyoid nerve runs down and forward between the mandible and the medial pterygoid muscle and lodges in the mylohyoid groove. The buccal nerve emerges from the undersurface of the ramus of the mandible. Abbreviations: A., artery; Alv., alveolar; Ant., anterior; Car., carotid; CN., cranial nerve; Eust., Eustachian; Gl., gland; Inf., inferior; Int., internal; Lat., lateral; Lev. Vel. Pal. M., levator veli palatini muscle; M., muscle; Max., maxillary; Med., medial; N., nerve; Ptery., pterygoid; Sph. Mand. Lig., sphenomandibular ligament; STA., superficial temporal artery; Temp., temporal; Ten. Vel. Pal. M., tensor veli palatini muscle. (Images courtesy of AL Rhoton, Jr.)
Most of the parasympathetic fibers leave the lingual nerve at the level of the submandibular gland to end in the submandibular ganglion, suspended from the nerve as it courses just above the gland; the fibers from the ganglion are distributed to the submandibular and sublingual glands, while the sensory fibers in the lingual nerve are distributed to the anterior two third of the tongue (Figs. 1D and 13A).
Inferior alveolar nerve. The inferior alveolar nerve is the largest branch of the mandibular division of the trigeminal nerve. The nerve usually gives four distributing branches and some communicating branches, three of which are sensory branches and one a motor branch. Sensory branches are the incisive nerve, the mental nerve, and the nerve to the lower premolars and molars. The motor branch is the nerve to the mylohyoid (Figs. 13C–13E). The inferior alveolar nerve arises from the posterolateral surface of the main mandibular trunk and descends deep to the lateral pterygoid muscle and then, at the lower border of the muscle, it passes between the sphenomandibular ligament and the ramus of the mandible to the mandibular foramen (Figs. 7E, 7F, 10C, 10F, and 13C). The distance from the mandibular notch to the mandibular foramen was 17.4 mm (range, 15–20 mm) (Joo et al., 2013). Below the lateral pterygoid, it is accompanied by the inferior alveolar artery arising from the maxillary artery (Fig. 13E). The inferior alveolar nerve enters the mandibular foramen slightly anterior and superior to the inferior alveolar artery. The length of the inferior alveolar nerve before it enters the mandibular foramen was 31.1 mm (range, 13–44 mm) (Joo et al., 2013). The nerve passes through the body of the mandible, sometimes enclosed by a thick connective tissue sheath within the bony canal, and gives off branches to the teeth which may form a plexus between the trunk of the nerve and the roots of the teeth (Zoud and Doran, 1993).
The inferior alveolar nerve gives off the mylohyoid nerve just before it enters the mandibular foramen (Figs. 13D and 13E). The nerve to the mylohyoid nerve pierces the sphenomandibular ligament, runs downward and forward below the mylohyoid line, a groove on the ramus of the mandible. It then appears in the digastric triangle and supplies both the mylohyoid and anterior belly of the digastric muscle (Gray and Williams, 1989b; Kumar et al., 2011; Shankland, 2001c). However, Kumar et al. (2011) reported that they found the nerve to the mylohyoid nerve, which arose from the trunk of the mandibular nerve and passed posteromedial to the inferior alveolar nerve in five of 50 southern Indian cadavers (Kumar et al., 2011). Recently, Kim et al. (2004) described communication between the mylohyoid and lingual nerve in 12.5% of examined cases and they first mentioned that this communication could provide another route for collateral sensory transmission to the tongue (Kim et al., 2004).
The dental branches of the inferior alveolar nerve supply the molar, premolar, incisor, and canine teeth. Before they enter the dental root, they communicate and form an inferior dental plexus, which is located between the mandibular canal and the roots of the mandibular teeth. The mental nerve, pure sensory, is a large branch of the inferior alveolar nerve that leaves the interior of the mandible to supply the skin of the chin and lower lip, the mucosa of the lip, and the adjacent gum. The mental foramen may usually be found on the vertical line drawn downward from the supraorbital notch and lies below the level of premolar teeth (Fig. 7E) (Hollinshead, 1982b). The mental nerve, emerging from its foramen, divides beneath the depressor anguli oris into three: a branch descending to the skin of the chin and two ascending to the skin and mucosa of the lower lip. These branches communicate with mandibular branch of the facial nerve.
Submandibular ganglion. This peripheral parasympathetic ganglion is a small, fusiform body, which lies on the upper part of the hyoglossus. It situates superior to the deep part of the submandibular gland and inferior to the lingual nerve, suspended from the lingual nerve by anterior and posterior filaments (Figs. 13A and 13B). Although the ganglion is related to the lingual nerve, it is connected functionally with the facial nerve and chorda tympani. The preganglionic parasympathetic fibers leave the superior salivatory nucleus of facial nerve in the brain stem. It enters the chorda tympani which leaves the facial nerve above the stylomastoid foramen and takes a recurrent course upward and forward in its canaliculus to enter the tympanic cavity through its posterior wall. It crosses the upper aspect of the tympanic membrane between malleus and incus and leaves the cavity through a canal in the petrotympanic fissure. It then joins the posterior aspect of the lingual nerve at an acute angle (Figs. 10F and 11C). The chorda tympani contains preganglionic parasympathetic secretomotor fibers which enter the submandibular ganglion, from which postganglionic fibers are relayed to the submandibular and sublingual glands (Fig. 1D).
The sympathetic root is derived from the plexus on the facial artery. It contains postganglionic fibers from the superior cervical ganglion, which traverse the submandibular ganglion without synapse. They are vasomotor to the blood vessels of the submandibular and sublingual glands.
CONCLUSIONS
The trigeminal nerve is the largest cranial nerve and contains both sensory and motor components. It is encountered with imaging or surgery of the skull base surgery. With advancement of the surgical procedures, many of the lesions involving the trigeminal nerve can be treated surgically. Thus, a comprehensive knowledge of the anatomy of the trigeminal nerve is crucial for performing the surgical procedures without significant complication.
Contributors: Wonil Joo, Fumitaka Yoshioka, Takeshi Funaki, Koji Mizokami, and Albert L. Rhoton, Jr
Content from Joo W, Yoshioka F, Funaki T, Mizokami K, Rhoton AL, Jr. Microsurgical anatomy of the trigeminal nerve. Clin Anat 2014;27:61–88. doi.org/10.1002/ca.22330.
The Neurosurgical Atlas is honored to maintain the legacy of Albert L. Rhoton, Jr, MD.
References
- Akita K, Shimokawa T, Sato T. 2000. Positional relationships between the masticatory muscles and their innervating nerves with special reference to the lateral pterygoid and the midmedial and discotemporal muscle bundles of temporalis. J Anat 197: 291–302.
- Al-Mefty O, Ayoubi S, Gaber E. 2002. Trigeminal schwannomas: removal of dumbbell-shaped tumors through the expanded Meckel cave and outcomes of cranial nerve function. J Neurosurg 96:453–463.
- Alfieri A, Jho HD, Schettino R, Tschabitscher M. 2003. Endoscopic endonasal approach to the pterygopalatine fossa: Anatomic study. Neurosurgery 52:374–378; discussion 378–380.
- Arslan M, Deda H, Avci E, Elhan A, Tekdemir I, Tubbs RS, Silav G, Yilmaz E, Baskaya MK. 2012. Anatomy of Meckel’s cave and the trigeminal ganglion: Anatomical landmarks for a safer approach to them. Turk Neurosurg 22:317–323.
- Barakos JA, D’Amour PG, Dillon WP, Newton TH. 1990. Trigeminal sensory neuropathy caused by cervical disk herniation. AJNR 11:609.
- Baumel JJ, Vanderheiden JP, McElenney JE. 1971. The auriculotemporal nerve of man. Am J Anat 130:431–440.
- Benninger B, Kloenne J, Horn JL. 2012. Clinical anatomy of the lingual nerve and identification with ultrasonography. Br J Oral Maxillofac Surg 51:541–544.
- Borschel GH, Kawamura DH, Kasukurthi R, Hunter DA, Zuker RM, Woo AS. 2012. The motor nerve to the masseter muscle: an anatomic and histomorphometric study to facilitate its use in facial reanimation. J Plast Reconstr Aesthet Surg 65:363–366.
- Carpenter MB. 1991a. Blood supply of the central nervous system. In: Carpenter MB, editor. Core Text of Neuroanatomy. 4th Ed. Baltimore: Williams & Wilkins. p 434–462.
- Carpenter MB. 1991b. The pons. In: Carpenter MB, editor. Core Text of Neuroanatomy. 4th Ed. Baltimore: Williams & Wilkins. p 151–191.
- Cuzalina AL, Holmes JD. 2005. A simple and reliable landmark for identification of the supraorbital nerve in surgery of the forehead: An in vivo anatomical study. J Oral Maxillofac Surg 63:25–27.
- Davies JC, Charles M, Cantelmi D, Liebgott B, Ravichandiran M, Ravichandiran K, Agur AM. 2012. Lateral pterygoid muscle: A three-dimensional analysis of neuromuscular partitioning. Clin Anat 25:576–583.
- Day JD, Giannotta SL, Fukushima T. 1994. Extradural temporopolar approach to lesions of the upper basilar artery and infrachiasmatic region. J Neurosurg 81:230–235.
- Dodd J, Kelly JP. 1991. The trigeminal system. In: Kandel ER, Schwartz JH, Jessell TM, editors. Principles of Neural Science. 3rd Ed. New York: Elsevier.
- Dolenc VV. 1989. Anatomy of the Cavernous Sinus. Wien; New York: Springer-Verlag. p. 3–7.
- el Shazly MA. 1991. Endoscopic surgery of the vidian nerve. Preliminary report. Ann Otol Rhinol Laryngol 100:536–539.
- Fix JD. 1995. Gross anatomy of the brain. In: Fix JD, editor. Neuroanatomy. 2nd Ed. Baltimore: Williams & Wilkins. p 1–31.
- Foucart JM, Girin JP, Carpentier P. 1998. Innervation of the human lateral pterygoid muscle. Surg Radiol Anat 20:185–189.
- Froelich SC, Aziz KM, Levine NB, Theodosopoulos PV, van Loveren HR, Keller JT. 2007. Refinement of the extradural anterior clinoidectomy: surgical anatomy of the orbitotemporal periosteal fold, Neurosurgery 61:179–185; discussion 185–176.
- Gülekon N, Anil A, Poyraz A, Peker T, Turgut HB, Karak€ose M. 2005. Variations in the anatomy of the auriculotemporal nerve. Clin Anat 18:15–22.
- Go JL, Kim PE, Zee CS. 2001. The trigeminal nerve. Semin Ultrasound CT MR 22:502–520.
- Govsa F, Kayalioglu G, Erturk M, Ozgur T. 1999. The superior orbital fissure and its contents. Surg Radiol Anat 21:181–185.
- Gray H, Williams PL. 1989a. Cranial and intracranial veins. In: Gray H, editor. Gray’s Anatomy. 37th Ed. Edinburgh; New York: C. Livingstone. p 798–805.
- Gray H, Williams PL. 1989b. The cranial nerves. In: Gray H, editor. Gray’s Anatomy. 37th Ed. Edinburgh; New York: C. Livingstone.
- Hollinshead WH. 1982a. The cranium. In: Hollinshead WH, editor. Anatomy for Surgeons. 3rd Ed. Philadelphia [etc.]: Lippincott. p 60–68.
- Hollinshead WH. 1982b. The jaws palate, and tongue. In: Hollinshead WH, editor. Anatomy for Surgeons. 3rd Ed. Philadelphia [etc.]: Lippincott. p 325–385.
- Hu KS, Kwak HH, Song WC, Kang HJ, Kim HC, Fontaine C, Kim HJ. 2006. Branching patterns of the infraorbital nerve and topography within the infraorbital space. J Craniofac Surg 17:1111–1115.
- Hwang K, Kim YJ, Chung IH, Song YB. 2005. Course of the masseteric nerve in masseter muscle. J Craniofac Surg 16:197–200.
- Izci Y, Gonul E. 2006. The microsurgical anatomy of the ciliary ganglion and its clinical importance in orbital traumas: An anatomic study. Minim Invasive Neurosurg 49:156–160.
- Janis JE, Hatef DA, Ducic I, Ahmad J, Wong C, Hoxworth RE, Osborn T. 2010. Anatomy of the auriculotemporal nerve: Variations in its relationship to the superficial temporal artery and implications for the treatment of migraine headaches. Plast Reconstr Surg 125:1422–1428.
- Jannetta PJ. 1996. Trigeminal neuralgia: Treatment by microvascular decompression. In: Wilkins RH, Rengachary SS, editors. Neurosurgery. 2nd Ed. New York: McGraw-Hill. p 3961–3968.
- Jeong SM, Park KJ, Kang SH, Shin HW, Kim H, Lee HK, Chung YG. 2010. Anatomical consideration of the anterior and lateral cutaneous nerves in the scalp. J Korean Med Sci 25:517–522.
- Joo W, Funaki T, Yoshioka F, Rhoton AL Jr. 2013. Microsurgical anatomy of the infratemporal fossa. Clin Anat 26:455–469.
- Kapila A, Chakeres DW, Blanco E. 1984. The Meckel cave: computed tomographic study. Part I: Normal anatomy; Part II: Pathology. Radiology 152:425–433.
- Kawase T, van Loveren H, Keller JT, Tew JM. 1996. Meningeal architecture of the cavernous sinus: Clinical and surgical implications, Neurosurgery 39:527–534; discussion 526–534.
- Kehrli P, Maillot C, Wolff MJ. 1997. Anatomy and embryology of the trigeminal nerve and its branches in the parasellar area. Neurol Res 19:57–65.
- Kierner AC, Mayer R, Adunka O. 2003. Is there a double innervation of the tensor tympani muscle in humans? Ann Otol Rhinol Laryngol 112:1056–1058.
- Kiesselbach JE, Chamberlain JG. 1984. Clinical and anatomic observations on the relationship of the lingual nerve to the mandibular third molar region. J Oral Maxillofac Surg 42:565–567.
- Kim HJ, Kwak HH, Hu KS, Park HD, Kang HC, Jung HS, Koh KS. 2003. Topographic anatomy of the mandibular nerve branches distributed on the two heads of the lateral pterygoid. Int J Oral Maxillofac Surg 32:408–413.
- Kim HS, Kim DI, Chung IH. 1996. High-resolution CT of the pterygopalatine fossa and its communications. Neuroradiology 38(Suppl 1):S120–S126.
- Kim SY, Hu KS, Chung IH, Lee EW, Kim HJ. 2004. Topographic anatomy of the lingual nerve and variations in communication pattern of the mandibular nerve branches. Surg Radiol Anat 26:128–135.
- Kumar S, Kumar CJ, Bhat S, Kumar A. 2011. Anatomical study of the unusual origin of a nerve to the mylohyoid muscle and its clinical relevance. Br J Oral Maxillofac Surg 49:e14–e15.
- Kunc Z, Ceskoslovenská akademie věd. 1964. Tractus spinalis nervi trigemini: Fresh anatomic data and their significance for surgery. Praha: Nakladatelství Ceskoslovenské akademie věd.
- Kwak HH, Ko SJ, Jung HS, Park HD, Chung IH, Kim HJ. 2003. Topographic anatomy of the deep temporal nerves, with references to the superior head of lateral pterygoid. Surg Radiol Anat 25:393–399.
- Lang J. 1981. [Neuroanatomy of the optic, trigeminal, facial, glossopharyngeal, vagus, accessory and hypoglossal nerves (author’s transl)]. Arch Otorhinolaryngol 231:1–69.
- Loughner BA, Larkin LH, Mahan PE. 1990. Nerve entrapment in the lateral pterygoid muscle. Oral Surg Oral Med Oral Pathol 69:299–306.
- Martins C, Costa E Silva IE, Campero A, Yasuda A, Aguiar LR, Tatagiba M, Rhoton A Jr. 2011. Microsurgical anatomy of the orbit: The rule of seven. Anat Res Int 2011:468727.
- Moore KL, Dalley AF. 1999. Clinically Oriented Anatomy, 4th Ed. Baltimore [etc.]: Lippincott Williams & Wilkins. p. 859–861.
- Moretto EP, Silva GH, Toledo Filho JL, Andreo JC, Navarro Rde L, Navarro JA. 2005. Surgical anatomy of the maxillary nerve in the zygomatic region. J Appl Oral Sci 13:167–170.
- Morton AL, Khan A. 1991. Internal maxillary artery variability in the pterygopalatine fossa. Otolaryngol Head Neck Surg 104:204–209.
- Natori Y, Rhoton AL Jr. 1995. Microsurgical anatomy of the superior orbital fissure. Neurosurgery 36:762–775.
- Osawa S, Rhoton AL Jr, Tanriover N, Shimizu S, Fujii K. 2008. Microsurgical anatomy and surgical exposure of the petrous segment of the internal carotid artery, Neurosurgery 63:210–238; Discussion 239.
- Peker S, Kurtkaya O, Uz€un I, Pamir MN. 2006. Microanatomy of the central myelin-peripheral myelin transition zone of the trigeminal nerve, Neurosurgery 59:354–359; Discussion 354–359.
- Pelletier VA, Poulos DA, Lende RA. 1974. Functional localization in the trigeminal root. J Neurosurg 40:504–513.
- Piagkou MN, Demesticha T, Piagkos G, Androutsos G, Skandalakis P. 2011. Mandibular nerve entrapment in the infratemporal fossa. Surg Radiol Anat 33:291–299.
- Pogrel MA, Renaut A, Schmidt B, Ammar A. 1995. The relationship of the lingual nerve to the mandibular third molar region: An anatomic study. J Oral Maxillofac Surg 53:1178–1181.
- Rahman M, Richter EO, Osawa S, Rhoton AL Jr. 2009. Anatomic study of the infraorbital foramen for radiofrequency neurotomy of the infraorbital nerve, Neurosurgery 64:423–427; Discussion 427–428.
- Rhoton AL. 2003a. The cavernous sinus, the cavernous venous plexus, and the carotid collar. In: Rhoton AL, Congress of Neurological Surgeons, editors. Rhoton Cranial Anatomy and Surgical Approaches. Philadelphia: LippincottWilliams & Wilkins. p 403–438.
- Rhoton AL. 2003b. The orbit. In: Rhoton AL, Congress of Neurological Surgeons, editors. Rhoton Cranial Anatomy and Surgical Approaches. Philadelphia: Lippincott Williams & Wilkins. p 331–362.
- Rhoton AL Jr. 2000. The cerebellopontine angle and posterior fossa cranial nerves by the retrosigmoid approach. Neurosurgery 47: S93–S129.
- Rusu MC, Pop F, Curcă GC, Podoleanu L, Voinea LM. 2009. The pterygopalatine ganglion in humans: A morphological study. Ann Anat 191:196–202.
- Sabanci PA, Batay F, Civelek E, Al Mefty O, Husain M, Abdulrauf SI, Karasu A. 2011. Meckel’s cave, World Neurosurg 76:335–341; Discussion 266–337.
- Saunders RL, Sachs E Jr. 1970. Relation of the accessory rootlets of the trigeminal nerve to its motor root. A microsurgical autopsy study. J Neurosurg 33:317–324.
- Schmidt BL, Pogrel MA, Necoechea M, Kearns G. 1998. The distribution of the auriculotemporal nerve around the temporomandibular joint. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 86:165–168.
- Shankland WE 2nd. 2000. The trigeminal nerve. Part I: An overview. Cranio 18:238–248.
- Shankland WE 2nd. 2001a. The trigeminal nerve. Part II: the ophthalmic division, Cranio 19:8–12.
- Shankland WE 2nd. 2001b. The trigeminal nerve. Part III: The maxillary division, Cranio 19:78–83.
- Shankland WE 2nd. 2001c. The trigeminal nerve. Part IV: the mandibular division, Cranio 19:153–161.
- Shi X, Han H, Zhao J, Zhou C. 2007. Microsurgical anatomy of the superior orbital fissure. Clin Anat 20:362–366.
- Shinohara H, Mataga I, Kageyama I. 2010. Discussion of clinical anatomy of the lingual nerves. Okajimas Folia Anat Jpn 87:97–102.
- Simoes S. 1993. An anatomical study of the laterotrigeminal venous system. Ann Anat 175:115–118.
- Taptas JN. 1982. The so-called cavernous sinus: A review of the controversy and its implications for neurosurgeons. Neurosurgery 11:712–717.
- Totonchi A, Pashmini N, Guyuron B. 2005. The zygomaticotemporal branch of the trigeminal nerve: An anatomical study. Plast Reconstr Surg 115:273–277.
- Tubbs RS, Hill M, May WR, Middlebrooks E, Kominek SZ, Marchase N, Shoja MM, Loukas M, Oakes WJ. 2008. Does the maxillary division of the trigeminal nerve traverse the cavernous sinus? An anatomical study and review of the literature. Surg Radiol Anat 30:37–40.
- Tubbs RS, Johnson PC, Loukas M, Shoja MM, Cohen-Gadol AA. 2010. Anatomical landmarks for localizing the buccal branch of the trigeminal nerve on the face. Surg Radiol Anat 32:933–935.
- Vrionis FD, Cano WG, Heilman CB. 1996. Microsurgical anatomy of the infratemporal fossa as viewed laterally and superiorly, Neurosurgery 39:777–785; discussion 776–785.
- Wentges RT. 1975. Surgical anatomy of the pterygopalatine fossa. J Laryngol Otol 89:35–45.
- Yoshida K, Kawase T. 1999. Trigeminal neurinomas extending into multiple fossae: surgical methods and review of the literature. J Neurosurg 91:202–211.
- Yousry I, Moriggl B, Holtmannspoetter M, Schmid UD, Naidich TP, Yousry TA. 2004. Detailed anatomy of the motor and sensory roots of the trigeminal nerve and their neurovascular relationships: a magnetic resonance imaging study. J Neurosurg 101:427–434.
- Youssef S, Kim EY, Aziz KM, Hemida S, Keller JT, van Loveren HR. 2006. The subtemporal interdural approach to dumbbell-shaped trigeminal schwannomas: Cadaveric prosection, Neurosurgery 59:ONS270–ONS277; discussion ONS277–ONS278.
- Zoud K, Doran GA. 1993. Microsurgical anatomy of the inferior alveolar neurovascular plexus. Surg Radiol Anat 15:175–179.
Please login to post a comment.