Hemangioblastoma
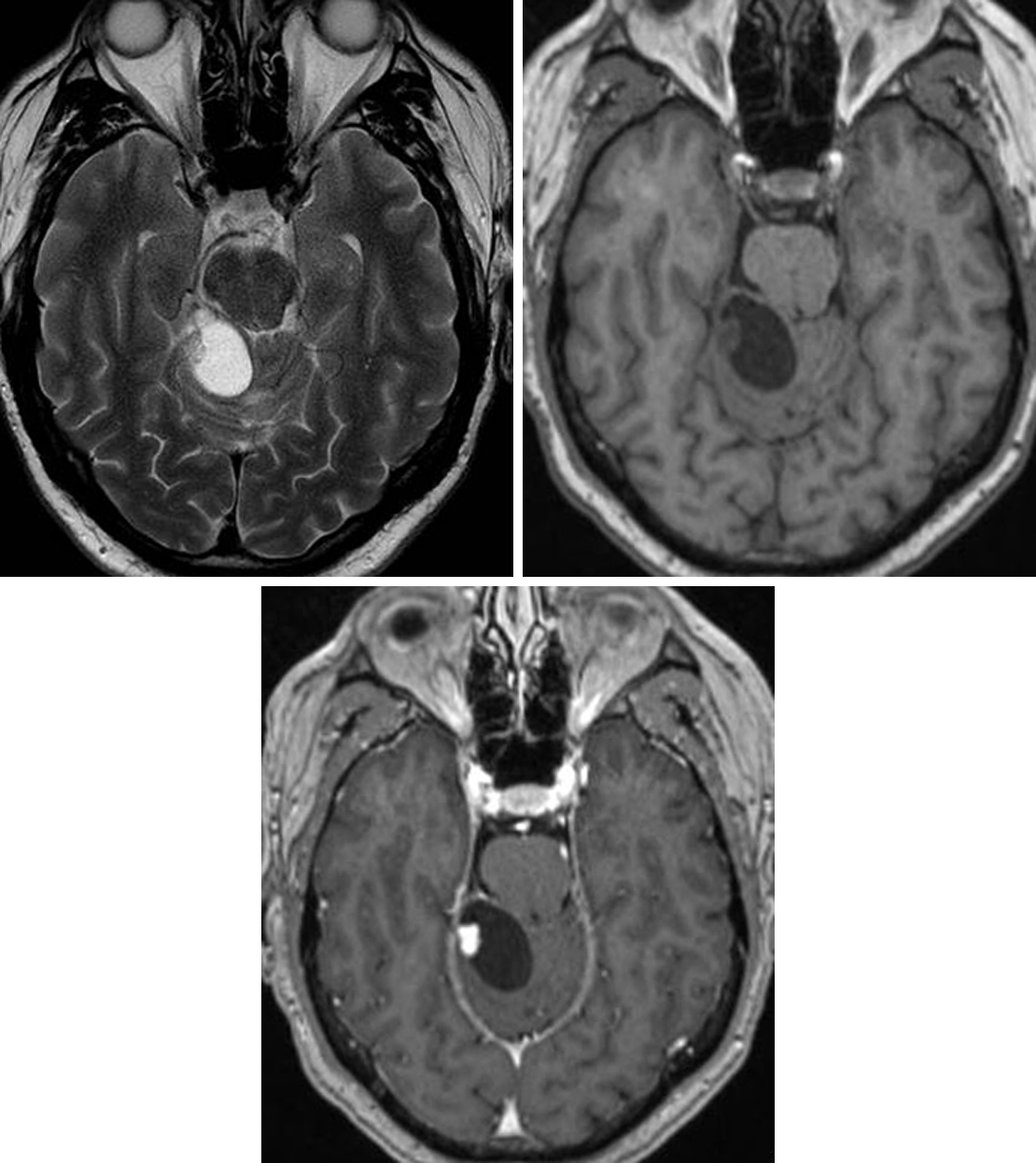
Figure 1: (Top Left) The cystic appearance is typical of this HGBL on T2WI. Note the posterior fossa location. The mural nodule is visible on T1WI but becomes much more evident after administration of intravenous contrast (bottom) due to its avid enhancement. The lack of enhancement in the cystic rim is also typical.
Figure 2: Axial T1 postcontrast (top left) and axial T2FS (top right) images demonstrate cystic lesions with associated enhancing dorsal nodules in the left posterior cerebellar hemisphere and right anterior cerebellar hemisphere, compatible with HGBLs. The smaller enhancing nodules in the right posterior cerebellar hemisphere are nonspecific in appearance but are favored to represent tiny HGBLs as well. Sagittal T1 postcontrast FS (middle left) and sagittal T2-weighted (middle right) images demonstrate multiple enhancing dorsal subpial nodules with extensive associated syrinx, compatible with spinal cord HGBLs. The patient initially presented in her late 20s with painless hematuria. (Bottom) CT imaging of the abdomen and pelvis with intravenous contrast at that time demonstrated heterogeneously enhancing renal masses, seen here in the medial aspect of the lower pole of the right kidney and lower pole of the left kidney, compatible with renal cell carcinoma in this patient with VHL disease. The hypodense lesions in the kidneys are compatible with renal cysts, which are also characteristic of VHL syndrome.
BASIC DESCRIPTION
- Usually benign, vascular, and slow-growing adult cerebellar tumor
PATHOLOGY
- WHO grade I
- Well-circumscribed, highly vascular mass composed of stromal cells and small blood vessels
- Sporadic or familial
- Familial cases associated with von Hippel-Lindau (VHL) disease
- Up to 40% of all hemangioblastomas (HGBLs) are in patients with VHL disease
- Often multiple, including retinal HGBLs
- Sporadic and VHL disease cases both demonstrate erythropoietin upregulation
CLINICAL FEATURES
- Sporadic: most commonly afflicts people aged 40 to 60 years
- VHL disease: afflicts younger people
- Slight male gender predilection
- Common presenting signs/symptoms related to increased intracranial pressure due to posterior fossa obstructive hydrocephalus
- Vomiting, altered mental status, macrocephaly
- Treatment: surgical resection
- Favorable prognosis: 10-year survival, 85%
- Tumor recurrence in up to 20%
- Leptomeningeal dissemination rare
IMAGING FEATURES
- General
- Posterior fossa mass
- Supratentorial, retinal HGBLs in patients with VHL disease
- Cyst with enhancing mural nodule common morphology but sometimes solid without cyst
- May have surrounding edema, particularly in the setting of hemorrhage
- Posterior fossa mass
- CT
- Hypodense cyst
- Isodense to hyperdense solid nodule
- Rare hyperdense hemorrhage, often with surrounding hypodense cerebellar edema
- Solid nodular component will enhance on contrast-enhanced CT
- MRI
- T1WI: isointense nodule, ±flow voids
- T2WI: hyperintense cyst and nodule, possible surrounding hyperintense edema
- FLAIR: hyperintense cyst and nodule, possible surrounding hyperintense edema
- T2*GRE: hypointense signal if hemorrhage is present
- T1WI+C: avidly enhancing nodule; nonenhancing cyst, usually without cyst wall enhancement
- DWI: possible DWI-bright, ADC-dark diffusion restriction in cystic component
- MRS: elevated Cho, decreased NAA, ±lactate/lipid peaks
IMAGING RECOMMENDATIONS
- MRI without and with intravenous contrast; screen patients with VHL disease, including both brain and spine, beginning in early childhood
For more information, please see the corresponding chapter in Radiopaedia. For additional information on spinal HGBLs, please refer to the hemangioblastoma chapter within the spinal disorders subvolume.
Contributors: Rachel Seltman, MD, and Jacob A. Eitel, MD
References
Conway JE, Chou D, Clatterbuck RE, et al. Hemangioblastomas of the central nervous system in von Hippel-Lindau syndrome and sporadic disease. Neurosurgery 2001;48:55–62, discussion 62–63. doi.org/10.1097/00006123-200101000-00009.
Innus C, Patterson J. Hemangioblastoma without von Hippel-Lindau disease. JAAPA 2007;20:28–32.
Osborn AG, Salzman KL, Jhaveri MD. Diagnostic Imaging (3rd ed). Elsevier, Philadelphia, PA; 2016.
Wanebo JE, Lonser RR, Glenn GM, et al. The natural history of hemangioblastomas of the central nervous system in patients with von Hippel-Lindau disease. J Neurosurg 2003;98:82–94. doi.org/10.3171/jns.2003.98.1.0082.
Please login to post a comment.