Hemangiopericytoma
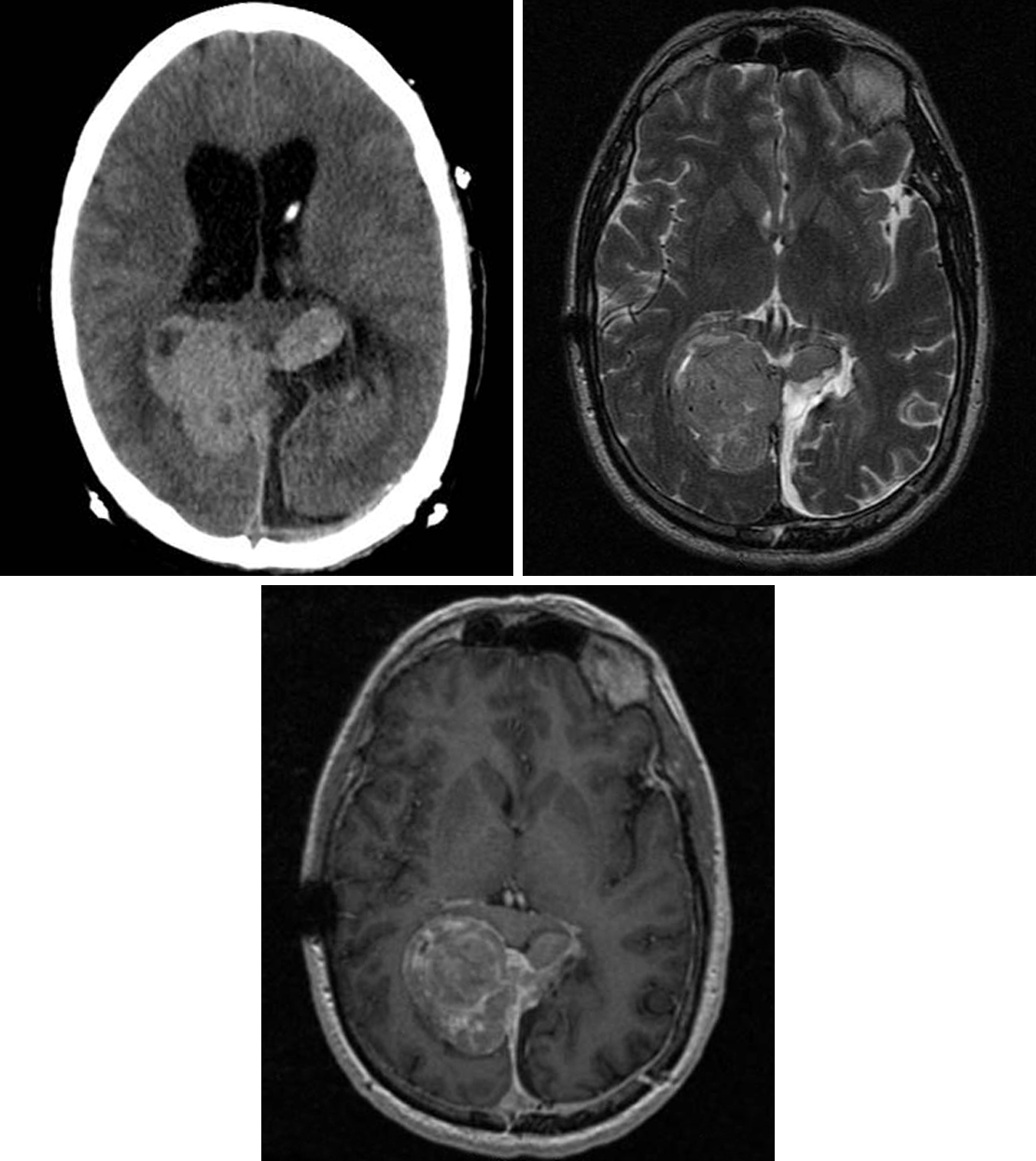
Figure 1: (Top Left) Often appearing as a more aggressive version of a meningioma, hemangiopericytoma is often seen as a complex-appearing extra-axial mass on CT, with areas of cystic degeneration and hyperdensity reflecting hypercellularity. (Top Right) T2WI confirms the extra-axial location with the adjacent cerebrospinal fluid cleft. Low T2 signal likely also reflects hypercellularity. (Bottom) A contrast-enhanced image demonstrates heterogeneous enhancement of this falx-based lesion. This patient had already undergone previous resection of the lesion from a left occipital approach.
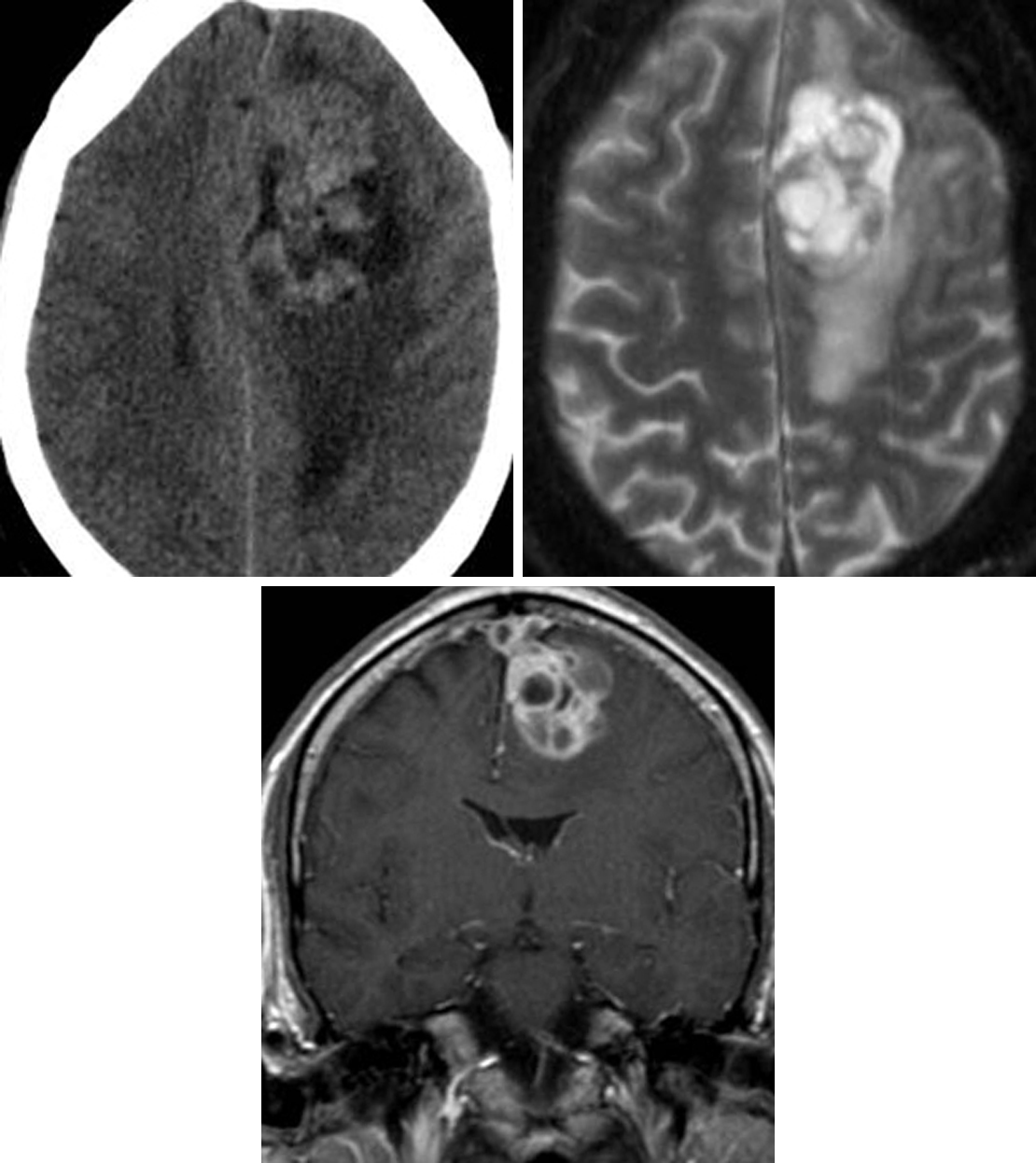
Figure 2: (Top Left) This hemangiopericytoma demonstrates complexity, cystic change, and hyperdensity on CT imaging. (Top Right) The cystic changes and surrounding edema are even more evident on T2WI. (Bottom) Avid, heterogeneous enhancement on postcontrast imaging is also typical. This lesion has also invaded the superior sagittal sinus, visible on this coronal contrast-enhanced image.
BASIC DESCRIPTION
- Highly vascular, hypercellular meningeal mesenchymal tumor
- Fibroblastic sarcoma
- Synonymous with “solitary fibrous tumor, hemangiocytoma type”
PATHOLOGY
- WHO grade II or III (anaplastic)
- Arises from smooth muscle pericytes around meningeal capillaries
- “Staghorn” pattern of malignant cells surrounding blood vessels
- Hypercellular, increased mitotic index (Ki-67, 5%–10%)
- Markedly increased mitoses, necrosis in WHO grade III tumors
- More aggressive than meningiomas
- Anaplastic tumors have a tendency for systemic metastases
CLINICAL FEATURES
- Adults most commonly afflicted (fouth to sixth decades of life)
- Slight male gender predilection
- Common presenting signs/symptoms: headache
- Treatment: surgical resection ± presurgical embolization due to risk of intraoperative hemorrhage, chemotherapy, radiation therapy
- Long-term patient monitoring due to delayed local recurrence, metastases
- Prognosis: 5-year survival, >90%
IMAGING FEATURES
- General
- Lobulated, enhancing extra-axial mass with dural attachment (dural tail)
- Mimics meningioma but lacks calcification or adjacent calvarial hyperostosis
- Dural sinus invasion, calvarial erosion may be seen
- CT
- Hyperdense extra-axial mass
- Hypodense peritumoral edema
- ±Calvarial erosion
- Heterogeneous but avid enhancement on contrast-enhanced CT imaging
- MRI
- T1WI: heterogeneous signal, ±flow voids
- T2WI: heterogeneous signal, hyperintense peritumoral edema, ±flow voids
- T1WI+C: heterogeneous but avid enhancement, ±dural tail
- MRV: ±dural venous sinus invasion/occlusion
IMAGING RECOMMENDATIONS
- MRI without and with intravenous contrast; CT to help characterize calvarial invasion
For more information, please see the corresponding chapter in Radiopaedia.
Contributor: Rachel Seltman, MD
References
Damodaran O, Robbins P, Knuckey N, et al. Primary intracranial haemangiopericytoma: comparison of survival outcomes and metastatic potential in WHO grade II and III variants. J Clin Neurosci 2014;21:1310–1314. doi.org/10.1016/j.jocn.2013.11.026.
Fountas KN, Kapsalaki E, Kassam M, et al. Management of intracranial meningeal hemangiopericytomas: outcome and experience. Neurosurg Rev 2006;29:145–153. doi.org/10.1007/s10143-005-0001-9.
Liu G, Chen Z-Y, Ma L, et al. Intracranial hemangiopericytoma: MR imaging findings and diagnostic usefulness of minimum ADC values. J Magn Reson Imaging 2013;38:1146–1151. doi.org/10.1002/jmri.24075.
Louis DN, et al. WHO Classification of Tumours of the CNS: Haemangiopericytoma. IARC Press, Lyon, France; 2007:178–180.
Osborn AG, Salzman, KL, Jhaveri MD. Diagnostic Imaging (3rd ed). Elsevier, Philadelphia, PA; 2016.
Sibtain NA, Butt S, Connor SEJ, et al. Imaging features of central nervous system haemangiopericytomas. Eur Radiol 2007;17:1685–1693. doi.org/10.1007/s00330-006-0471-3.
Smith AB, Horkanyne-Szakaly I, Schroeder JW, et al. From the radiologic pathology archives: mass lesions of the dura: beyond meningioma-radiologic-pathologic correlation. Radiographics 2014;34:295–312. doi.org/10.1148/rg.342130075.
Wu W, Shi J, Cheng H, et al. Hemangiopericytomas in the central nervous system. J Clin Neurosci 2009;16:519–523. doi.org/10.1016/j.jocn.2008.06.011.
Please login to post a comment.