Subfrontal Translamina Terminalis Approach
This is a preview. Check to see if you have access to the full video. Check access
Resection of a Predominately Solid Third Ventricular Craniopharyngioma via the Subfrontal Translamina Terminalis Approach Using an Orbitozygomatic Craniotomy
General Considerations and Indications for the Approach
The lamina terminalis is a thin membrane composed of gray matter, pia mater, and ependyma bordered superiorly by the anterior commissure, laterally by the cerebral hemispheres and inferiorly by the superior aspect of the optic chiasm. Embryologically, this lamina represents the most rostral end of the developing neural tube.
The subfrontal translamina terminalis approach uses the anterior wall of the third ventricle (lamina terminalis) to reach anterior lesions in this chamber. I use this approach rarely, mainly for large predominately solid craniopharyngiomas and hypothalamic hamartomas. Cystic craniopharyngiomas are ideally exposed via the transnasal transtuberculum route.
The subfrontal approach for a solid third ventricular craniopharyngioma requires a modified orbitozygomatic craniotomy, so an inferior-to-superior subfrontal operative trajectory facilitates handling of the superior pole of the tumor without aggressive retraction of the basal frontal lobe.
The subfrontal translamina terminalis approach is a restricted, nonflexible operative corridor that cannot be safely expanded. Gross total tumor resection can be problematic. The anterior interhemispheric modification of this approach may provide more extended operative space but is not minimally disruptive.
The manipulations required through this narrow corridor often lead to cognitive decline, most likely because of blind dealings with the ventricular wall. Despite use of an orbitozygomatic craniotomy, a fair amount of retraction on the frontal lobe is necessary.
Figure 1: A predominately solid craniopharyngioma of the third ventricle is a reasonable candidate for the subfrontal translamina terminalis approach using an orbitozygomatic craniotomy.
Preoperative Considerations
For a specific discussion of the preoperative considerations for third ventricular tumors, see the Principles of Intraventricular Surgery chapter.
Preoperative endocrinological and ophthalmological evaluations are necessary. The lamina terminalis should be affected by the tumor and the optic apparatus should not be covering the anterior and inferior poles of the tumor. The floor of the ventricle should also be affected by the tumor. An intact third ventricular floor is a contraindication for the use of this route and supports the use of the transcallosal transforaminal transvenous transchoroidal approach.
Operative Anatomy
The anatomy of the lamina terminalis is summarized in the following images.
Click here to view the interactive module and related content for this image.
Figure 2: The upper images demonstrate the attenuated texture of the lamina terminalis (yellow arrows) in relation to the chiasm. A view of the third ventricle through the lamina is depicted in the lower image, however, this is a non-operative view achieved via an anterior interhemispheric dissection requiring undue retraction on bilateral frontal lobes. Note the intimate relationship of the anterior communicating artery complex to the lamina (images courtesy of AL Rhoton, Jr).
SUBFRONTAL TRANSLAMINA TERMINALIS APPROACH VIA AN ORBITOZYGOMATIC CRANIOTOMY
This approach is especially favorable if the solid tumor extends through the lamina terminalis and has a small suprasellar component. Tumors with primarily suprasellar components are resected through the endoscopic transnasal transsphenoidal translamina terminalis approach.
This subfrontal translamina terminalis approach offers the advantage of providing excellent visualization of the lamina terminalis, optic nerves, optic chiasm, bilateral internal carotid arteries, anterior communicating artery complex, bilateral A2 segments, posterior communicating arteries, associated perforating branches, and the pituitary stalk.
Figure 3: The subfrontal translamina terminalis approach provides a limited exposure to the anterior third ventricle and is suitable for lesions enlarging the lamina terminalis and the associated operative pathway. A supraorbital craniotomy and orbital rim osteotomy is another reasonable skull base approach for this operative pathway.
INTRADURAL PROCEDURE
The use of dynamic retraction and wide arachnoidal dissection over bilateral optic nerves are necessary in reaching the lamina terminalis. The vector of retraction is parallel to the ipsilateral optic nerve.
Figure 4: A fair amount of frontal lobe retraction is necessary to expose and work through the lamina terminalis. The lamina is invaded by the tumor and has a distinct grayish color compared to the chiasm. The chiasm must be carefully protected from the incision in the lamina. Generous microsurgical dissection over the chiasm allows identification of the exact borders of the lamina.
Figure 5: This is an exposure of the lamina terminalis via a left-sided orbitozygomatic craniotomy (see Figure 1 for the corresponding preoperative scans). The grayish tumor has expanded the lamina. The anterior communicating artery complex (AComm) is labeled. Undue retraction of this vascular structure should be avoided. You can appreciate the narrow operative corridor.
Figure 6: Dynamic retraction allows precise expansion of the operative corridor at the working site of the instruments. The tumor is debulked and rolled out of the resection cavity (see Figure 5 above). There are numerous blind spots associated with the translamina terminalis approach. These blind spots include the posterior and superior aspects of the third ventricle and the ipsilateral wall of the hypothalamus. Consequently, excessive retraction is unavoidable, causing injury to the fornix, the supraoptic nuclei, the organ vasculosum, the tuber cinerum, and perforating vessels.
If the tumor reaches into the sella, the intrasellar portion of the tumor may be removed via the corridor between the optic nerves. However, I do not recommend this maneuver because of its associated morbidity that results from the blind manipulation of the optic nerves and their perforating vessels. The prefix chiasm can limit this working space.
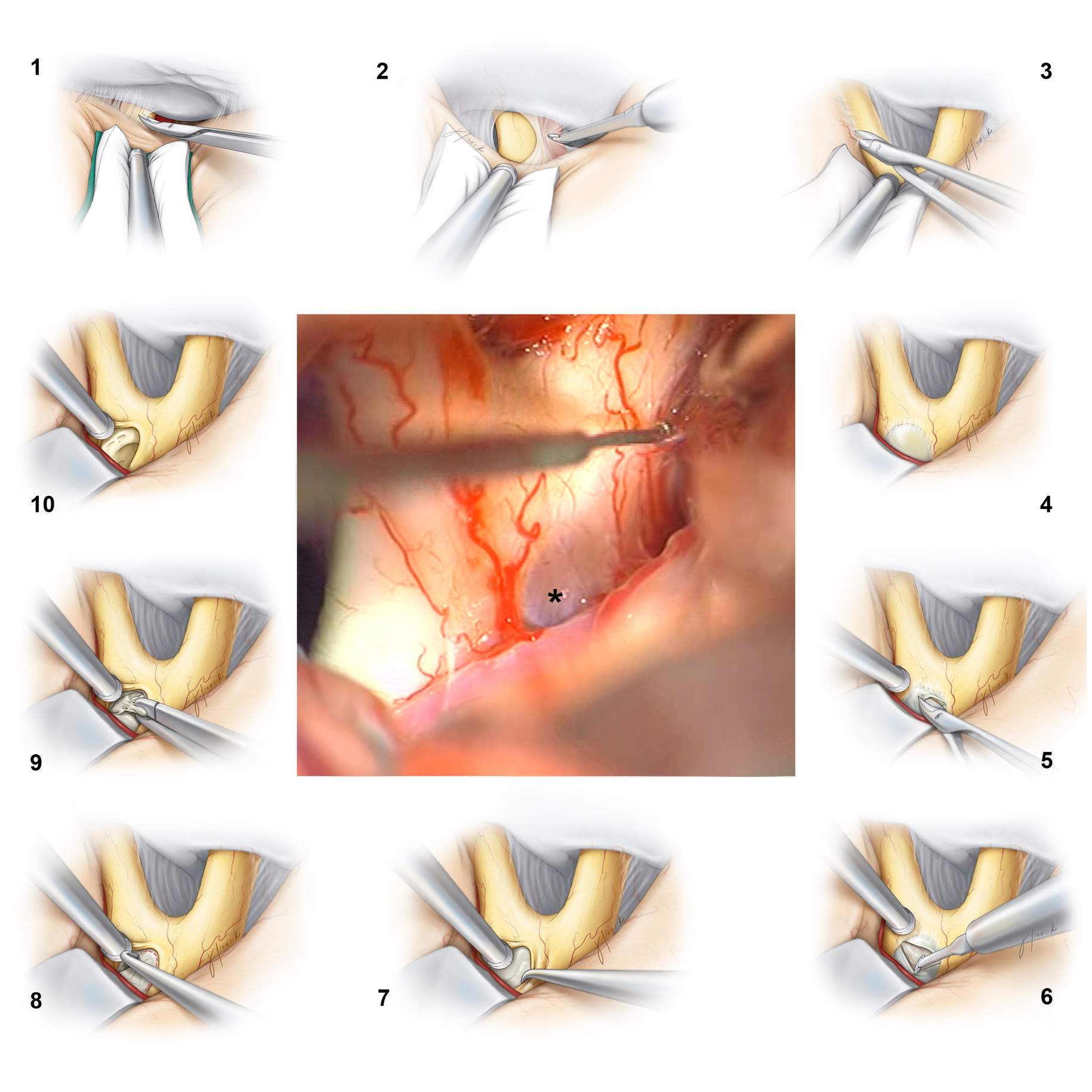
Figure 7: The thin membrane of the lamina terminalis is shown in the middle intraoperative photo (*). The other illustrations (clockwise) detail the operative maneuvers for resection of a hypothalamic hamartoma.
Resection of a Hypothalamic Hamartoma via the Supraorbital Translamina Terminalis Approach
Postoperative Considerations
For a detailed discussion of recommendations for postoperative care of patients with ventricular tumors, see the Principles of Intraventricular Surgery chapter.
Pearls and Pitfalls
- The subfrontal translamina terminalis approach is restrictive and should be used in the case of small tumors that are not amenable to its endoscopic transnasal counterpart. Gross total resection of large tumors is problematic and not usually feasible without undue retraction on the surrounding normal neurovascular structures.
Please login to post a comment.