Cavernous Sinus Surgery
Tumor Subtypes
Lesions involving the cavernous sinus have been considered a surgical challenge because of their relevant anatomic complexity, causing them to be described as “no man’s land.” Transcranial approaches have traditionally been used for treating tumors invading the cavernous sinus. This was especially the case during the late 1980s when complex skull base approaches were introduced and popularized.
However, the enthusiasm for radical skull base approaches and resections has recently dampened because of their associated high morbidity and with the development of nonsurgical therapies, such as radiosurgery.
The introduction of the endoscope to pituitary surgery revitalized interest in operating within and around the cavernous sinus, especially because of the advantages of broad peripheral and intracavitary visualization afforded via angled endoscopes and instruments. In addition, the transnasal trajectory offers unique advantages for protecting the neurovascular structures, especially for lesions that displace these structures laterally.
Lesions invading the cavernous sinus are rare entities, comprising approximately 10% to 17% of all sellar region tumors. Together, pituitary adenomas (58–78%), and chordomas/chondrosarcomas (13–17%) make up approximately 90% of all lesions managed endoscopically. Meningiomas, neurinomas, inflammatory disease (Tolosa-Hunt), lymphomas, and hemangiomas are rarely handled by the transnasal route.
The two most commonly encountered lesions for this approach are discussed below.
Pituitary Adenomas
For more details on pituitary adenomas’ epidemiology, clinical presentation, and diagnosis, please refer to the chapter Pituitary Adenoma: Diagnosis and Operative Considerations.
Pituitary adenomas are the prototype lesions that invade the cavernous sinus. They are usually soft tumors and barely infiltrate the internal carotid artery (ICA). Pituitary adenomas present a mediolateral pattern of growth, and consequently they displace the neurovascular structures within the cavernous sinus laterally. It is still unknown whether these lesions are opportunistic growths through weak cavernous sinus medial walls or signs of aggressive behavior.
Cavernous sinus invasion has been documented in 9% to 63% of all pituitary adenomas. They affect patients who have a mean age of 50 years and they may affect females slightly more often than males. Ectopic pituitary adenomas in the cavernous sinus are extremely rare. Bilateral cavernous sinus involvement, on the other hand, has a more frequent occurrence in up to one-third of the cases.
Most pituitary tumors invading the cavernous sinus are nonfunctioning lesions (25–54%), followed by GH-secreting (24–36.7%), prolactin-secreting (17–20%), and ACTH-secreting adenomas (5–20%). The importance of gross total resection of functional tumors within the cavernous sinus cannot be underestimated.
Presenting signs and symptoms usually occur as a result of endocrine dysfunction or mass effect. Ophthalmoplegia is uncommon, affecting 10% to 17% of all patients with pituitary tumors harboring cavernous sinus invasion.
Chordomas/Chondrosarcomas
For more details on chordomas and chondrosarcomas epidemiology, clinical presentation, diagnosis, and evaluation, please refer to the Chordoma and Chondrosarcoma chapter. Some details with respect to cavernous sinus invasion are discussed here.
Chordomas are rare, slow-growing skull base neoplasms that are derived from the notochord remnants. These tumors affect the clival region in approximately 25% of patients and comprise only 0.15% of all intracranial tumors.
Patients are most often male (with a 1.1–1.5:1 sex ratio) in their fifth to sixth decade of life (with a mean age of 50 years). Carotid artery involvement can be observed in approximately 40% of the patients and cavernous sinus invasion in less than 10%.
Diplopia as a result of abducens palsy and headache are by far the most common preoperative symptoms (50–80% and 40–100%, respectively). Patients usually complain of dysphagia (20%), ophthalmoplegia due to impairment of the oculomotor and trochlear nerves (20–60%) and decreases in visual acuity (20%).
Operative Anatomy
The cavernous sinus is a paired venous structure located nearly in the center of the head. It receives venous drainage from most of the anterior and middle cranial bases, and the orbit as well. It has an extremely complex anatomy and contains several important neurovascular structures with a dura mater cover.
Alfieri and Jho detailed the endoscopic surgical anatomy of the cavernous sinus. The posterior wall of the sphenoid sinus was divided into five distinct vertical compartments: midline, bilateral paramedian, and bilateral lateral. Paramedian vertical areas include the optic canal and the bony protuberances over the parasellar and paraclival ICA. Lateral vertical compartments have four protuberances and three depressions.
Figure 1: Endoscopic view of the posterior wall of the sphenoid sinus. In the paramedian vertical compartment, the transition of the paraclival ICA (pcICA) to the parasellar ICA (psICA) is shown at the level of the sellar floor. In the lateral vertical compartment, bony protrusions comprise the optic canal over the optic nerve (ON), the cavernous sinus apex, V2, V3, and middle clinoid process (Middle Clin.)(image courtesy of Juan Fernandez-Miranda).
Figure 2: Top photograph: the middle clinoid process (Middle Clin.) was removed on the right side, but preserved on the left in order to demonstrate the gain in the exposure of the parasellar ICA (psICA) by removal of the process. Bottom image: this is an enhanced view after resection of the left middle clinoid process. ON: Optic Nerve (image courtesy of Juan Fernandez-Miranda).
Harris and Rhoton divided the cavernous sinus into four venous compartments depending on the position of the venous spaces in relation to the ICA: anteroinferior (ventral), medial, posterosuperior (dorsal), and lateral. The medial and anteroinferior venous spaces are dominant in the majority of cases, which gives further support to the rationale of approaching the cavernous sinus via the transnasal route.
The medial compartment is mainly devoid of major neurovascular structures and faces the pituitary gland, whereas the lateral compartment contains cranial nerves III, IV, V1, V2, V3, and VI. During the transcranial route, these nerves are often located between the surgeon and the pathology.
Figure 3: After removal of the bony walls over the sella and carotid protuberances, the periosteum, which constitutes the outer layer of the dura mater, comes into view. The cavernous sinus is housed between the periosteal and meningeal layers of the dura. The paraclival ICA (pcICA) and parasellar ICA (psICA) are easily seen through translucency. The position of the medial (medial comp.) and inferior compartments (Inf. comp.) of the cavernous sinus is shown. Middle Clin. (rem) — middle clinoid process removed. (Image courtesy of Juan Fernandez-Miranda.)
The parasellar segment of the ICA has a “C”-shaped structure. It is divided into four parts: the hidden segment or posterior bend, the inferior horizontal segment, the anterior vertical segment, and the superior horizontal segment.
Further lateral bone removal uncovers the lateral wall of the cavernous sinus. Preparation of this lateral part discloses some anatomic landmarks that are similar to those seen when using the transcranial route. The lateral wall cannot be adequately exposed without medial mobilization of the parasellar carotid artery.
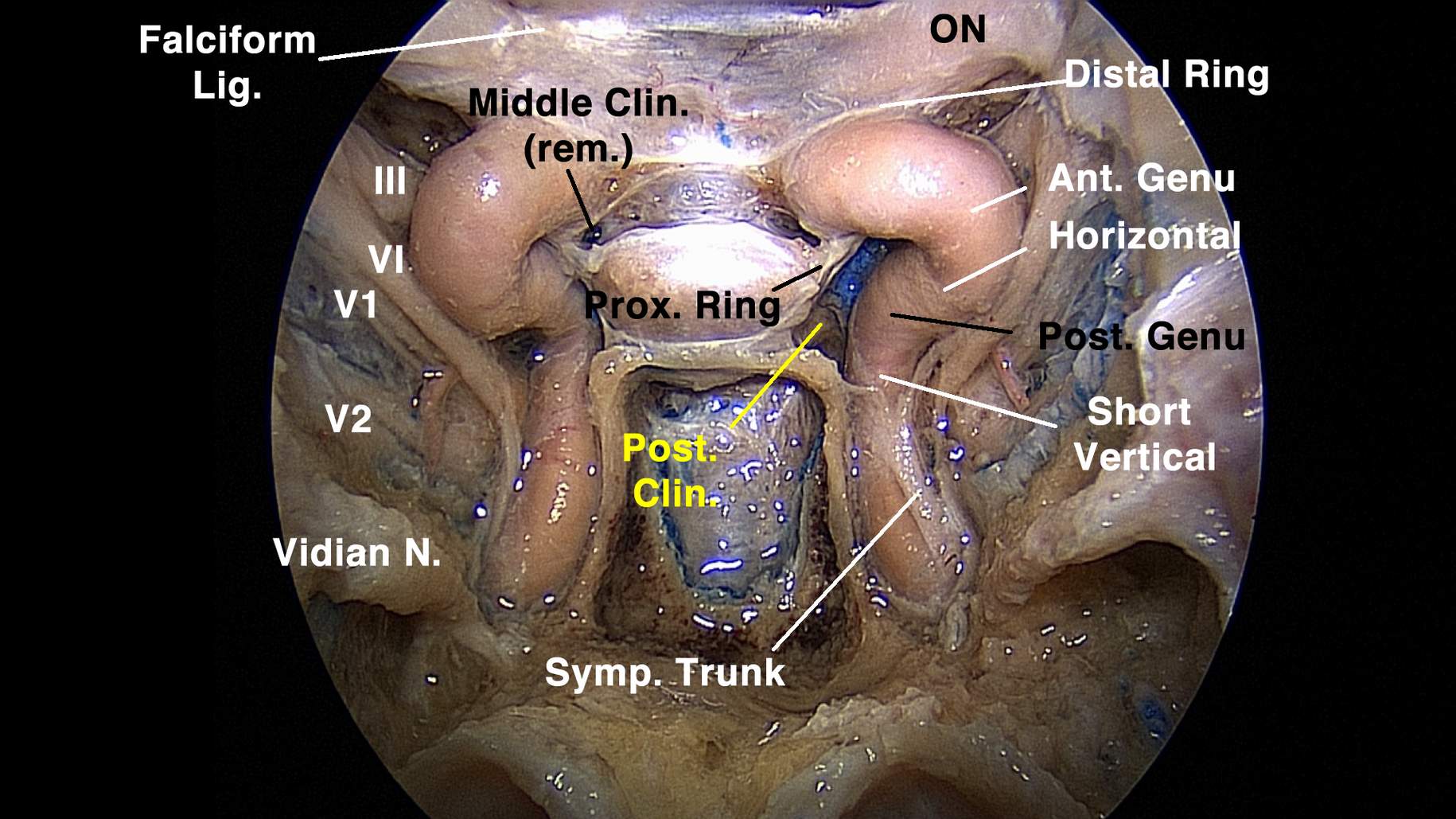
Figure 4: In this preparation, the periosteal layer was removed to expose the entirety of the cavernous sinus contents. Opening of the left medial wall of the cavernous sinus reveals the medial aspect of the parasellar ICA (Short vertical/Post. Genu — the hidden segment; Horizontal — inferior horizontal segment; Ant. Genu — anterior genu or anterior vertical segment). The pituitary gland is connected to the anterior bend of the parasellar ICA by an arachnoid band (Prox. Ring — proximal dural ring). Note that the vidian nerve (Vidian N.) comprises an important landmark in the sphenoid sinus floor, providing guidance to the ICA transition from the foramen lacerum to the paraclival carotid artery. Falciform Lig. — falciform ligament; Middle Clin. (rem.) — middle clinoid process removed; ON — optic nerve; Post. Clin. — posterior clinoid process; Symp. Trunk — sympathetic trunk (image courtesy of Juan Fernandez-Miranda).
Figure 5: At the depth of the middle compartment, the meningo-hypophyseal trunk is shown (Men.-Hyp. Trunk). By mobilizing the inferior horizontal segment of the parasellar ICA laterally, the oculomotor nerve (Interdural CN III) can be observed at the roof of the cavernous sinus. Ant. Genu — anterior genu; Basilar Tip — basilar artery tip; CN III — oculomotor nerve; Interclinoidal Lig. — interclinoidal ligament (image courtesy of Juan Fernandez-Miranda).
Figure 6: This is a lateral view of the left cavernous sinus showing the relationship of the parasellar ICA and its branches in the cavernous sinus compartments. Basilar Art. Tip — basilar artery tip; CN III — oculomotor nerve; CN VI — abducens nerve; Infero-Lat. Trunk — inferolateral trunk; Lat. comp. — lateral compartment; Men.-Hyp. Trunk — meningo-hypophyseal trunk; Post. comp. — posterior compartment; Sup. Cer. Art. — superior cerebellar artery; Sup. comp. — superior compartment (image courtesy of Juan Fernandez-Miranda).
Figure 7: By pushing the short vertical segment of the ICA anteriorly, we can bring the petrous apex into view. CN III — oculomotor nerve; CN IV — trochlear nerve; CN VI — abducens nerve; Inf. Petr. Sin. — inferior petrosal sinus; Post. comp. — posterior compartment; Sup. Cer. Art. — superior cerebellar artery; Sup. Petr. Sin. — superior petrosal sinus (image courtesy of Juan Fernandez-Miranda).
Figure 8: In this wide panoramic view of the left cavernous sinus, all neurovascular structures can be appreciated from different compartments. The meningo-hypophyseal trunk (Men.-Hyp. Trunk) is located at the depth of the medial compartment. Posterior (Post. comp.) and superior compartments (Sup. comp.) are mainly devoid of major structures. Note that the interdural portion of the abducens nerve (CN VI Dorello’s Ch.) is reached at the inferior portion of the posterior compartment, and therefore drilling of the clivus should be carefully done near the paraclival ICA. The lateral compartment (Lat. comp.), however, contains the inferolateral trunk (Infero-Lat. Trunk) and the cranial nerves. III — oculomotor nerve; Floor — cavernous sinus floor; Symp. Trunk — sympathetic trunk (image courtesy of Juan Fernandez-Miranda).
Figure 9: This endoscopic view of the left cavernous sinus lateral wall shows the entire course of the abducens nerve (CN VI) and its anatomic relationships to the short vertical segment of the ICA and the inferolateral trunk (Infero-Lat. Trunk). Lat. comp. — lateral compartment; Symp. Trunk — sympathetic trunk (image courtesy of Juan Fernandez-Miranda).
Diagnosis
Please refer to the chapters titled Pituitary Adenoma: Diagnosis and Operative Considerations and Chordoma and Chondrosarcoma.
Evaluation
Magnetic resonance (MR) imaging with contrast enhancement is the diagnostic study of choice for detecting cavernous sinus invasion. Coronal T1- and T2-weighted sequences are routinely included in the evaluation and are most relevant.
Several different criteria have been proposed to address cavernous sinus invasion shown on imaging. A major limitation of the imaging has always been its inaccuracy in defining the medial wall of the cavernous sinus, especially when associated with a sellar lesion.
This fact results in a significant ambiguity in describing cavernous sinus invasion by imaging and intraoperative observation. A recent meta-analysis revealed a higher prevalence of cavernous sinus invasion on radiographic criteria than suggested by intraoperative inspection for pituitary adenomas (43% vs. 18%, respectively).
The Knosp-Steiner classification has been the most traditional methodology to evaluate cavernous sinus invasion by imaging since its description in 1993. Increasing grades carry a progressive risk of invasion based on the position of the lateral portion of the tumor in relation to the ICA. A Knosp grade 3 or greater has a specificity of 90% for cavernous sinus invasion. Although this classification system was originally described for pituitary adenomas, its use has been expanded for nonadematous tumors as well.
| Grade | Description |
| 1 | Lateral tumor extension beyond the medial intercarotid line |
| 2 | Lateral tumor extension beyond the median intercarotid line |
| 3 | Tumor extension beyond the lateral intercarotid line |
| 4 | Encasement of the intracavernous internal carotid artery |
This classification was reassessed in the era of neuroendoscopy. Intermediate grades were found to be consistently less involved in comparison with the involvement determined by microscopic inspection. The updated risk of cavernous sinus invasion was 1.5% for grade 1; 9.9% for grade 2; 37.9% for grade 3; and 100% for grade 4 tumors. Grade 3 is divided in order to distinguish the involvement of superior and inferior cavernous sinus compartments, namely grades 3A and 3B, respectively. The rate of invasion is significantly different — from 26.5% in grade 3A to 70.6% in grade 3B.
Figure 10: Schematic representation of the updated Knosp-Steiner classification for cavernous sinus invasion.
Inferolateral venous compartment obliteration (IVLCO) and percentage encasement of the ICA (PEICA) are additional imaging criteria employed to detect cavernous sinus invasion by pituitary adenomas. These have better correlation with intraoperative observations. Solely 3% of the patients with no obliteration or less than 30% encasement presented surgical evidence of cavernous sinus invasion.
Displacement of the carotid artery, asymmetry of the cavernous sinuses, lateral bulging of the wall of the cavernous sinus, and obliteration of the superior venous compartment are additional parameters to evaluate for cavernous sinus involvement.
Computed tomography scans have a prominent role in the identification of size, shape, and pneumatization of the sphenoid sinus for surgical planning of endoscopic cavernous sinus approaches. The definition of the surgical landmarks is much more demanding in presellar or conchal-type sphenoid sinuses.
Figure 11: These images demonstrate an asymmetric pituitary adenoma with invasion of the right cavernous sinus (Knosp-Steiner Grade 4). Note that the ICA is completely encased by the tumor. The obliteration of the inferolateral venous compartment is also evident.
Indications for Surgery
Surgery for cavernous sinus tumors is highly controversial and remains a major source of criticism and contention by some colleagues. This controversy is mainly attributed to the unsatisfactory experience obtained via the transcranial route.
The rationale behind operating on the cavernous sinus from the endoscopic endonasal approach is based on pathologic and anatomic observations. Sellar (pituitary adenomas) and clival tumors (chordomas/chondrosarcomas) have an antero-inferior and medio-to-lateral direction of growth, which is similar to the surgical route and its long axis through the natural corridor of the nose and sphenoid sinus. Moreover, as mentioned before, the dominant venous compartments are usually the antero-inferior and medial ones.
Currently, surgical management of cavernous sinus tumors through the extended endonasal route is indicated for the following lesions:
- histologic diagnosis for lesions other than pituitary adenomas and chordomas/chondrosarcomas;
- endocrine cure for selected and ectopic functional adenomas;
- cytoreduction in the preparation for radiosurgery or adjuvant proton-beam radiation therapy; and
- symptomatic improvement in patients affected by cavernous sinus syndrome.
Preoperative Considerations
Please refer to the chapter Pituitary Adenoma: Diagnosis and Operative Considerations.
RESECTION OF INTRACAVERNOUS TUMORS
Initial anatomic studies on cavernous sinus surgery by the endoscopic route divided surgical approaches according to the corridor used within the nasal cavity into paraseptal (between the nasal septum and the middle turbinate), middle meatal (between the middle turbinate and the lateral wall of the nasal cavity), and middle turbinectomy (by removing the caudal half of the middle turbinate) approaches.
Clinical studies, however, have named the approaches according to the extent of bone removal needed to reach different cavernous sinus venous compartments. In this section, I have didactically divided the approaches to the cavernous sinus into those for medial and lateral intracavernous tumors.
For medial cavernous sinus tumors, the standard extended endoscopic approaches are usually adequate for most cases of sellar masses. Further lateral and inferior tumor extension demands widening of the surgical route via the transsphenoidal transethmoidal approach. This technique involves resection of the posterior sphenoid sinus wall over the carotid protuberance toward the cavernous sinus apex (~10% of the cases).
For lateral cavernous sinus tumors, the lateral operative trajectory can be secured by removing the pterygoid plate and the posterior wall of the maxillary sinus through a maxillary antrostomy (~15% of the cases).
It is worth emphasizing that a conservative strategy for intracavernous tumor removal is advised, especially for laterally situated tumors.
Exposure
For a detailed discussion on perioperative patient care, surgical positioning, and surgical approach, please refer to the Endoscopic Extended Transnasal Approach and Giant and Multicompartmental Pituitary Adenoma chapters. However, some especially relevant features are worth discussing here.
The nasoseptal flap is developed in the beginning of surgery and retracted toward the ipsilateral nasopharynx or into the maxillary sinus. For tumors with lateral extension, which require a transpterygoid approach, it is wise to develop the flap contralaterally since the surgical route occurs through its base.
OPERATIVE APPROACHES FOR MEDIAL INTRACAVERNOUS TUMORS
Standard and Extended Endoscopic Endonasal Transsphenoidal Approach
When reaching the posterior wall of the sphenoid sinus, bone removal extends over the medial aspects of both cavernous sinuses for the standard endoscopic approach. Further bone drilling over the tubercullum sella and the posterior portion of the planum sphenoidale is required for handling large and giant pituitary adenomas with significant suprasellar extension (extended approach). A posterior partial ethmoidectomy may be needed to increase suprasellar visualization.
Tumor removal starts with central internal decompression using a suction device and ring curettes. I often use two suction devices to efficiently remove easily deliverable tumor for large and giant lesions. The inferior and central portion of the tumor should be debulked first, followed by the lateral portions: I resist the temptation to remove the readily visible anterosuperior portions of the tumor because this would cause the diaphragm to prematurely descend, obscuring and hiding the lateral poles of the tumor.
The next step is to assess cavernous sinus invasion by inspection of the medial wall with a 30-degree endoscope. If the tumor is well circumscribed within the sella (that is, when no extension into the cavernous sinus is apparent), then the lateral tumor capsules can be peeled away from the medial wall of the sinus.
If the tumor extends into the cavernous sinus, then the tumor is “chased” into the medial venous compartment; next, stepwise tumor debulking will provide additional space for exposure of the tumor components residing within the sinus.
Neurophysiologic monitoring and stimulation mapping of the abducens, oculomotor, and trochlear nerves are routinely used.
After lateral decompression, the suprasellar portion can be assessed. Further details on suprasellar tumor removal and management of descending diaphragma sella are addressed in the Pituitary Macroadenoma chapter.
Extended Endoscopic Endonasal Transsphenoidal Transethmoidal Approach
Medial compartment tumors with obliteration of the inferolateral venous compartment require further lateral and anterior view. The approach consists of performing an anterior and posterior ethmoidectomy together with an upper turbinectomy, but not all of these steps are necessary in every case. The surgeon must be selective and judicious in determining what minimally destructive exposure is necessary to accomplish the job.
Figure 12: In such cases, sellar or clival bone opening is followed by resection of the bone over the anterior wall of the cavernous sinus, ipsilateral to tumor invasion, using a Kerrison punch (image courtesy of Juan C. Fernandez-Miranda).
Figure 13: For primary sellar tumors, dural opening is continuous from the sella toward the cavernous sinus. I usually open the dura in a cruciate fashion and the flaps are retracted by bipolar coagulation. As an alternative, a secondary dural opening can be made parallel and medial to the parasellar carotid. An essential step is the identification of the intracavernous ICA by the microDoppler probe. Inferolateral tumors may displace the ICA posteriorly; in these cases, identification of the artery may be more demanding (image courtesy of Juan C. Fernandez-Miranda).
Figure 14: Next, internal debulking is undertaken while the surgeon takes care to avoid early suprasellar decompression and resultant premature descending of the diaphragma sella. I often use two suction devices to remove the easily deliverable tumor fragments efficiently. Tumors with firmer consistency are removed with ring curettes and an ultrasonic aspirator. Adherent tumors to the neurovascular structures are left untouched (image courtesy of Juan C. Fernandez-Miranda).
Figure 15: After decompression of the medial compartment, the meningo-hypophyseal trunk comes into view. The parasellar ICA can be gently mobilized laterally to increase operative freedom (image courtesy of Juan C. Fernandez-Miranda). Venous bleeding is controlled with packing of Floseal hemostatic matrix (Baxter, Deerfield, IL).
OPERATIVE APPROACHES FOR LATERAL INTRACAVERNOUS TUMORS
Extended Endoscopic Endonasal Transsphenoidal Transethmoidal Approach
Lateral tumors are technically more challenging. After medial and inferolateral decompression, surgical view is directed toward the superior and posterior compartments. The ICA is gently mobilized inferiorly and laterally to improve visualization.
Figure 16: The lateral cavernous sinus can be decompressed between the horizontal segments of the carotid artery. At the end of surgical resection, the oculomotor nerve is identified at the tip of the left suction device (image courtesy of Juan C. Fernandez-Miranda).
Extended Endoscopic Endonasal Transmaxillary Transpterygoid Approach
The approach starts with uncinectomy and widening of the maxillary sinus ostium. The ethmoidectomy includes resection of the bulla and suprabullar cells.
The next step is opening of the sphenoid sinus medial to the ethmoidectomy. The exposition of the inferior aspect of the maxillary sinus may require an inferior turbinectomy.
The sphenopalatine artery is identified in its foramen and transected near the crista ethmoidalis. Then, the approach is directed to the orbital process of the palatine bone, which is removed by bone drilling and rongeurs. Further bone removal of the posteromedial maxillary sinus walls reveals the pterygopalatine fossa. Its contents are pushed laterally and the preparation is taken toward the sphenoid sinus floor.
The impression of the vidian nerve is identified at the floor of the sphenoid sinus and the nerve is usually preserved by drilling only the medial pterygoid plate. A wide exposure of the lateral recess of the sphenoid sinus is obtained with this approach.
The parasellar carotid artery is identified with microDoppler mapping and navigation, and the dura is incised laterally. Soft tumor components are removed, while firm tumors are usually left in place in order to avoid unintended neurovascular injury. Full exposure of the lateral wall of the cavernous sinus can be obtained only after medial mobilization of the parasellar carotid artery.
Closure
Closure is illustrated in detail in both the Endoscopic Extended Transnasal Approach and Giant and Multicompartmental Pituitary Adenoma chapters.
Of note, depending on the presence of a cerebrospinal fluid leak, closure is performed in a multilayered fashion with fat, allograft dura, and nasoseptal flap. In order to avoid a rupture late after surgery, the carotid artery should not be left uncovered.
Postoperative Considerations
Please refer to the Pituitary Adenoma: Diagnosis and Operative Considerations, Endoscopic Extended Transnasal Approach, and Chordoma and Chondrosarcoma chapters.
Cranial neuropathies usually improve after surgery. Transient postoperative cranial neuropathies may be especially observed in laterally seated tumors. Vision improvement is a rather common finding postoperatively. Endocrine dysfunction may also be ameliorated with surgery
Pearls and Pitfalls
- Cavernous sinus surgery can play a special role in the treatment of functional pituitary tumors.
- Three major surgical approaches are usually utilized for accessing the medial and lateral cavernous sinus compartments.
- Conservative resection within the lateral cavernous sinus can avoid unacceptable postoperative morbidity.
Contributor: Marcus André Acioly, MD, PhD
References
Abuzayed B, Tanriover N, Gazioglu N, Ozlen F, Cetin G, Akar Z. Endoscopic anatomy and approaches of the cavernous sinus: cadaver study. Surg Radiol Anat. 2010;32(5):499-508.
Alfieri A, Jho HD. Endoscopic endonasal cavernous sinus surgery: an anatomic study. Neurosurgery. 2001;48(4):827-837.
Ceylan S, Koc K, Anik I. Endoscopic endonasal transsphenoidal approach for pituitary adenomas invading the cavernous sinus. J Neurosurg. 2010;112(1):99-107.
Chibbaro S, Cornelius JF, Froelich S, Tigan L, Kehrli P, Debry C, Romano A, Herman P, George B, Bresson D. Endoscopic endonasal approach in the management of skull base chordomas—clinical experience on a large series, technique, outcome, and pitfalls. Neurosurg Rev. 2014;37(2):217-225.
Cottier JP, Destrieux C, Brunereau L, Bertrand P, Moreau L, Jan M, Herbreteau D. Cavernous sinus invasion by pituitary adenoma: MR imaging. Radiology. 2000;215(2):463-469.
Dhandapani S, Singh H, Negm HM, Cohen S, Anand VK, Schwartz TH. Cavernous sinus invasion in pituitary adenomas: systematic review and pooled data meta-analysis of radiologic criteria and comparison of endoscopic and microscopic surgery. World Neurosurg. 2016;96:36-46.
Dolci RL, Upadhyay S, Ditzel Filho LF, Fiore ME, Buohliqah L, Lazarini PR, Prevedello DM, Carrau RL. Endoscopic endonasal study of the cavernous sinus and quadrangular space: anatomic relationships. Head Neck. 2016;38 Suppl 1:E1680-1687.
Frank G, Pasquini E. Endoscopic endonasal cavernous sinus surgery, with special reference to pituitary adenomas. Front Horm Res. 2006;34:64-82.
Harris FS, Rhoton AL. Anatomy of the cavernous sinus. A microsurgical study. J Neurosurg. 1976;45(2):169-180.
Hofstetter CP, Singh A, Anand VK, Kacker A, Schwartz TH. The endoscopic, endonasal, transmaxillary transpterygoid approach to the pterygopalatine fossa, infratemporal fossa, petrous apex, and the Meckel cave. J Neurosurg. 2010;113(5):967-974.
Koutourousiou M, Winstead WI. Endoscopic endonasal surgery for remission of Cushing disease caused by ectopic intracavernous macroadenoma: case report and literature review. World Neurosurg. 2017 ;98:870.e5-870.e10.
Lobo B, Zhang X, Barkhoudarian G, Griffiths CF, Kelly DF. Endonasal endoscopic management of parasellar and cavernous sinus meningiomas. Neurosurg Clin N Am. 2015;26(3):389-401.
Micko AS, Wöhrer A, Wolfsberger S, Knosp E. Invasion of the cavernous sinus space in pituitary adenomas: endoscopic verification and its correlation with an MRI-based classification. J Neurosurg. 2015;122(4):803-811.
Patrona A, Patel KS, Bander ED, Mehta A, Tsiouris AJ, Anand VK, Schwartz TH. Endoscopic endonasal surgery for nonadenomatous, nonmeningeal pathology involving the cavernous sinus. J Neurosurg. 2017;126(3):880-888
Raithatha R, McCoul ED, Woodworth GF, Schwartz TH, Anand VK. Endoscopic endonasal approaches to the cavernous sinus. Int Forum Allergy Rhinol. 2012;2(1):9-15.
Woodworth GF, Patel KS, Shin B, Burkhardt JK, Tsiouris AJ, McCoul ED, Anand VK, Schwartz TH. Surgical outcomes using a medial-to-lateral endonasal endoscopic approach to pituitary adenomas invading the cavernous sinus. J Neurosurg. 2014;120(5):1086-1094.
Please login to post a comment.