Posterior Interhemispheric Transcallosal Intervenous/Paravenous Variant
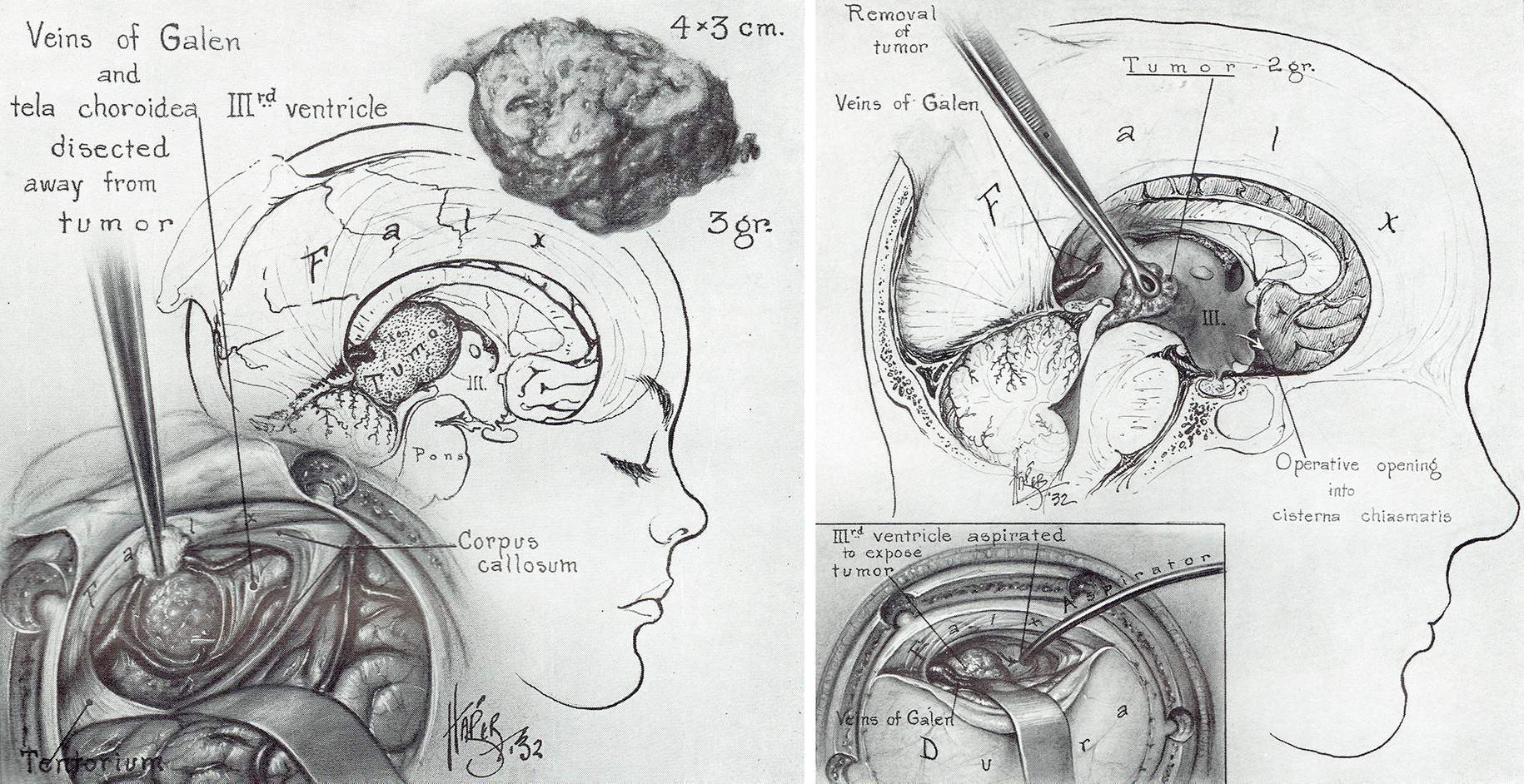
Figure 1: Walter Dandy described the posterior interhemispheric transcallosal approach approximately 100 years ago for resection of pineal region tumors.
This is a preview. Check to see if you have access to the full video. Check access
Resection of a Large Recurrent Posterior Third Ventricular Epidermoid Tumor
General Considerations
In this chapter, our specific region of interest is the posterior segment of the third ventricle. The region around the aqueduct of Sylvius and the suprapineal recess demarcate this segment. The structures composing this region include the posterior commissure, pineal body, and habenular commissure.
Figure 2: A posterior third ventricular ependymoma is illustrated. Note the overlying neurovascular structures, including the internal cerebral veins. Posterior third ventricular tumors are among the most unreachable tumors. The deep diencephalic veins block their access through a posterior corridor.
Figure 3: Some of the posterior third ventricular tumors invade and expand an opening within the tectum. This opening allows their exposure via the infratentorial supracerebellar approach.
Diagnosis and Evaluation
For a general discussion of diagnosis and evaluation for ventricular tumors, see the Principles of Intraventricular Surgery chapter.
Patients who harbor a tumor in this region often present with obstructive hydrocephalus because of the location of the tumor near the third ventricle and aqueduct. If the tumor is large or intratumoral hemorrhage or pineal apoplexy occurs, the patient may develop Parinaud’s syndrome.
Figure 4: A posterior third ventricular pineoblastoma is shown. This tumor was removed using the posterior interhemispheric transcallosal intervenous approach (right image). I have also used the paramedian supracerebellar route for such tumors. The location of the deep veins defines the appropriate approach. If the veins are mobilized posteriorly, the supracerebellar route is deemed unsafe
Indications for Surgery
The goals for surgery in this region may be gross total resection, biopsy alone, or reestablishment of cerebrospinal fluid flow. During preoperative planning, I consider the goals of the surgery based on the size and location of the tumor and its invasion of the neurovascular structures.
Of course, the surgeon’s experience and comfort level with various approaches are imperative in operative planning. In addition, the texture of the tumor (soft and suckable versus firm and vascular) must be considered in the decision to proceed with a particular approach. Firm and vascular tumors require wider operative corridors.
Two methods that are most commonly chosen to access the posterior third ventricle/pineal area are the supracerebellar-infratentorial route and the occipital interhemispheric-transtentorial route. I have predominantly used the infratentorial supracerebellar pathway because of its minimal disruption of the normal anatomy. I do not prefer the occipital interhemispheric transtentorial route because it places a number of supratentorial structures at risk.
The disadvantages of the occipital interhemispheric-transtentorial route include the vulnerability of the occipital lobe, the straight sinus and its anastomosing veins, and the corpus callosum (splenium).
Parinaud’s syndrome can result from injury to the quadrigeminal plate from the use of the supracerebellar-infratentorial route. The paramedian supracerebellar transventricular approach for small posterior third ventricular lesions is addressed in its own dedicated chapter.
Overall, based on the exact location of the lesion, the following routes have been described:
- Posterior interhemispheric transcallosal intervenous/paravenous route (described in this chapter,)
- Paramedian supracerebellar transventricular approach
- Occipital interhemispheric transtentorial route
- Anterior interhemispheric transcallosal interforniceal approach.
For a general discussion of the indications for surgery in patients with ventricular tumors, see the Principles of Intraventricular Surgery chapter.
Preoperative Considerations
A careful study of the preoperative magnetic resonance images (MRI) determines the location of the internal cerebral veins, veins of Rosenthal and Galen in relation to the tumor. This important information will determine the pathway of the dissection between or around the internal cerebral veins (intervenous versus paravenous). Superior and anterior dislocation of the veins indicates a need for a posterior approach, preferably via the supracerebellar route.
Parasagittal veins are more indispensable in the posterior frontal and parietal regions, and their sacrifice and manipulation may predispose the patient to venous infarction. The preoperative MRI or a computed tomography (CT) venogram may help determine the side of approach that avoids dominant parasagittal veins along the desired interhemispheric operative corridor.
The use of an external ventricular drain in the presence of non-communicating hydrocephalus is advised so that interhemispheric dissection is pursued safely. In the absence of hydrocephalus, I use a lumbar drain to facilitate smooth dissection before entering the ventricle.
Operative Anatomy
For further details regarding the relevant anatomy of the region, please refer to the Anatomy of the Ventricular System and the Transcallosal Interforniceal Approach chapters.
POSTERIOR INTERHEMISPHERIC TRANSCALLOSAL INTERVENOUS/PARAVENOUS VARIANT
The posterior interhemispheric transcallosal intervenous/paravenous variant is appropriate for lesions that lie primarily within the posterior third ventricle, quadrigeminal plate, and pineal region. For this approach, the center and bulk of the tumor should be within the ventricle, rather than in the pineal region. This approach provides a unique and suitable surgical field for the area anterior to the internal cerebral veins, straight sinus, vein of Galen, and pineal region.
Figure 5: For the posterior interhemispheric transcallosal intervenous/paravenous approach, the patient may be positioned supine or lateral. More neck flexion is required than for an anterior transcallosal approach. I prefer a line incision because it provides adequate exposure and heals well. For a midline pathology, the bone flap is usually made on the right side. For a paramedian pathology, the bone flap is placed on the ipsilateral side. It is approximately 5 to 6 cm long in an anterior-to-posterior direction, and centered either on the coronal suture or one-third anterior and two-thirds posterior to it.
Navigation is mandatory for planning the precise location of the bone flap and callosotomy and fine-tuning the operative trajectory. I unroof the superior sagittal sinus and open the dura using a curvilinear incision based along the superior sagittal sinus. I frequently need to sacrifice 1-2 small parasagittal draining veins when accessing the interhemispheric fissure.
The more posterior location of the craniotomy places the sensorimotor cortices at risk. Therefore, the surgeon must be especially cautious during exposure and interhemispheric dissection to prevent undo manipulation and retraction of these functional cortices. All parasagittal veins in the posterior extent of the craniotomy must be preserved.
Decompression and diversion of CSF greatly facilitates the work within the interhemispheric fissure.
INTRADURAL PROCEDURE
Navigation should be used to guide the extent of the callosotomy in relation to the tumor’s anteroposterior margins. Most of the splenium must be spared to prevent the risk of disconnection syndrome. The surgeon should continue the callosotomy and dissection following the midline plane; this maneuver will lead the operator to the avascular membrane that separates the internal cerebral veins. If the septum has not been invaded by tumor, I continue dissection between the leaflets of the septum pellucidum, avoiding the lateral ventricles, if possible.
The septum pellucidum has been usually invaded by the tumor, and its anatomy is distorted. In these cases, I enter the right ventricle (for a midline pathology) or the ipsilateral ventricle (for a paramedian pathology). For the technical tenets of this stage of the operation, please refer to the Transcallosal Interforniceal Approach chapter.
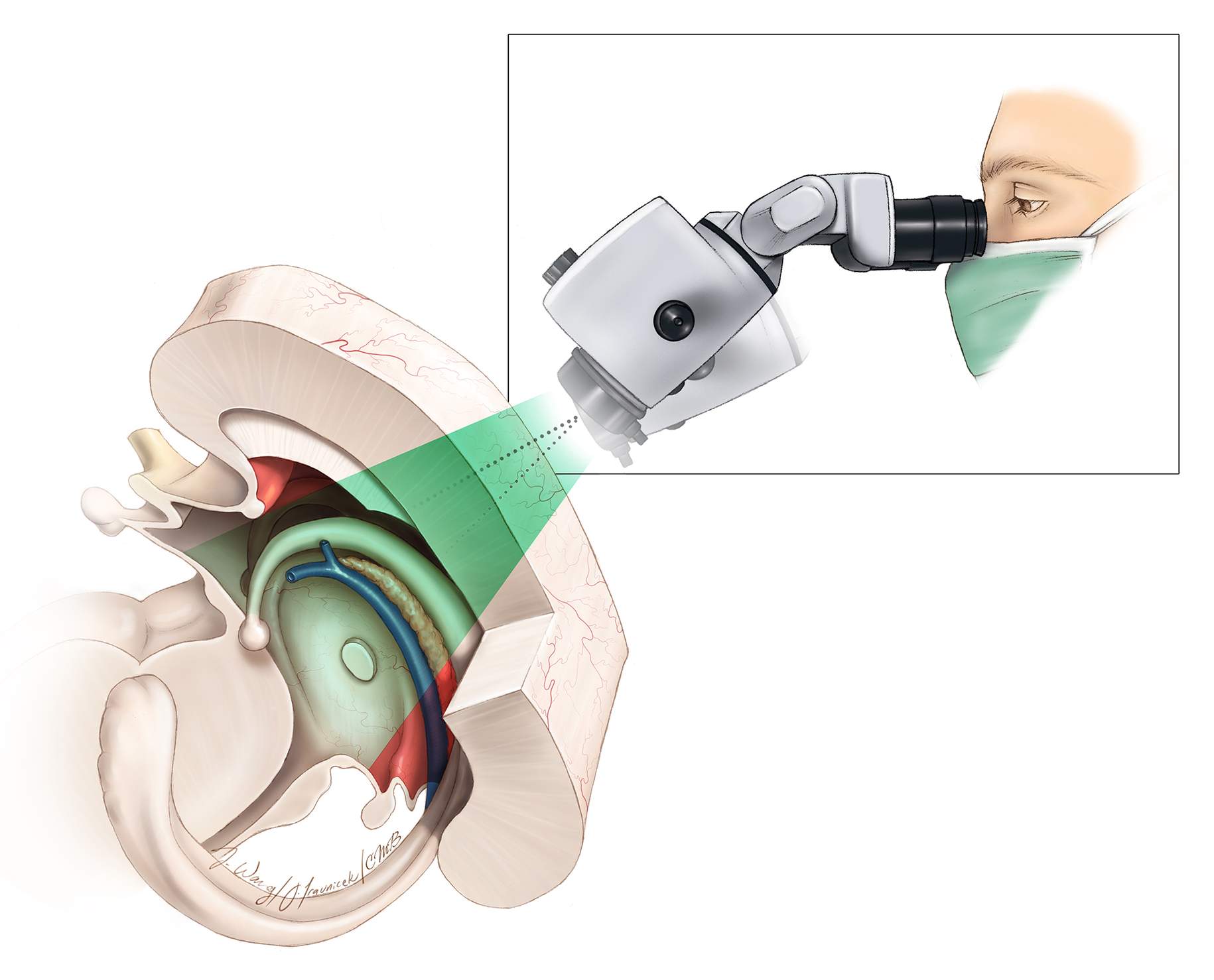
Figure 6: A sagittal operative view showing the operative trajectory for a posterior interhemispheric transcallosal intervenous/paravenous approach. Note that the more attenuated part of the callosum is entered and the splenium is spared. The working angle is from anterior-to-posterior to prevent the need to transect the splenium. The operative blind spots are immediately under the splenium (subsplenial) and laterally under the corpus callosum (subcallosal). Directing the line of sight of the scope in the anterior-to-posterior direction will expose the tumor contents immediately below the splenium (Redrawn from Tew, van Loveren, Keller*).
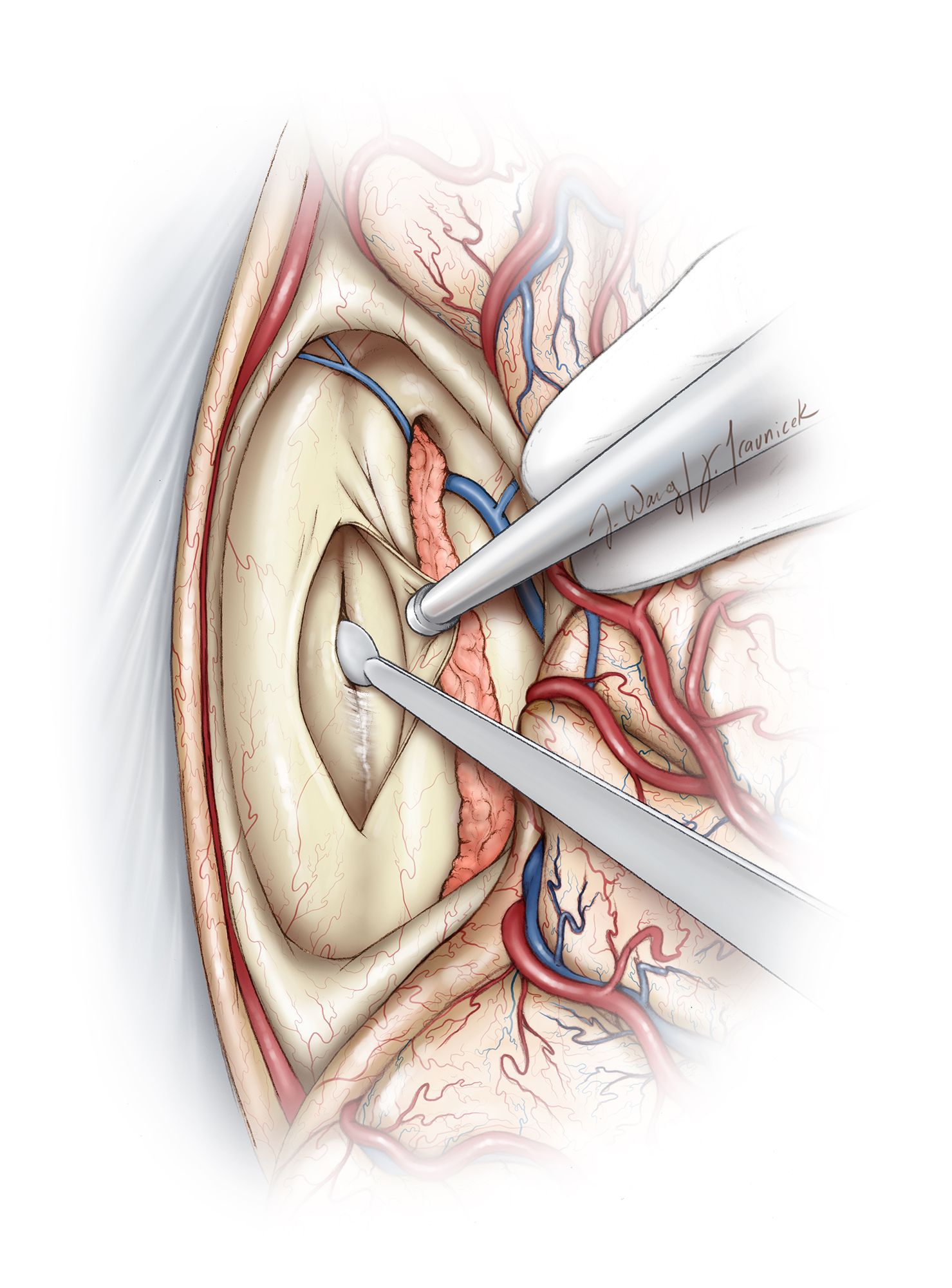
Figure 7: Once the callosotomy (~2 cm) is completed and the right ventricle is entered, I work between the leaflets of the septum for entry between (intervenous) or around (paravenous) the internal cerebral veins (Redrawn from Tew, van Loveren, Keller*).
Figure 8: If the septum is not invaded by the tumor, its leaflets are separated and the forniceal bodies detached along their raphe using a sharp microinstrument. If the septum has been destroyed by the tumor, the midline plane is developed until the tumor and internal cerebral veins below the forniceal raphe are identified. These veins diverge within the posterior roof of the third ventricle and are often further displaced away from each other by the tumor. These factors create the necessary resection corridor. The hippocampal commissures have frequently been invaded or posteriorly displaced by the tumor (Redrawn from Tew, van Loveren, Keller*).
Figure 9: There is often a layer of tenia choroidea just below the raphe that encases the internal cerebral veins. This layer is shapely opened to separate the veins laterally and disclose the tumor capsule. Dynamic retraction is used on the laterally located forniceal bodies. The internal cerebral veins remain separated near their convergence with the vein of Galen, and they are dissected anteriorly at this natural divide (Redrawn from Tew, van Loveren, Keller*).
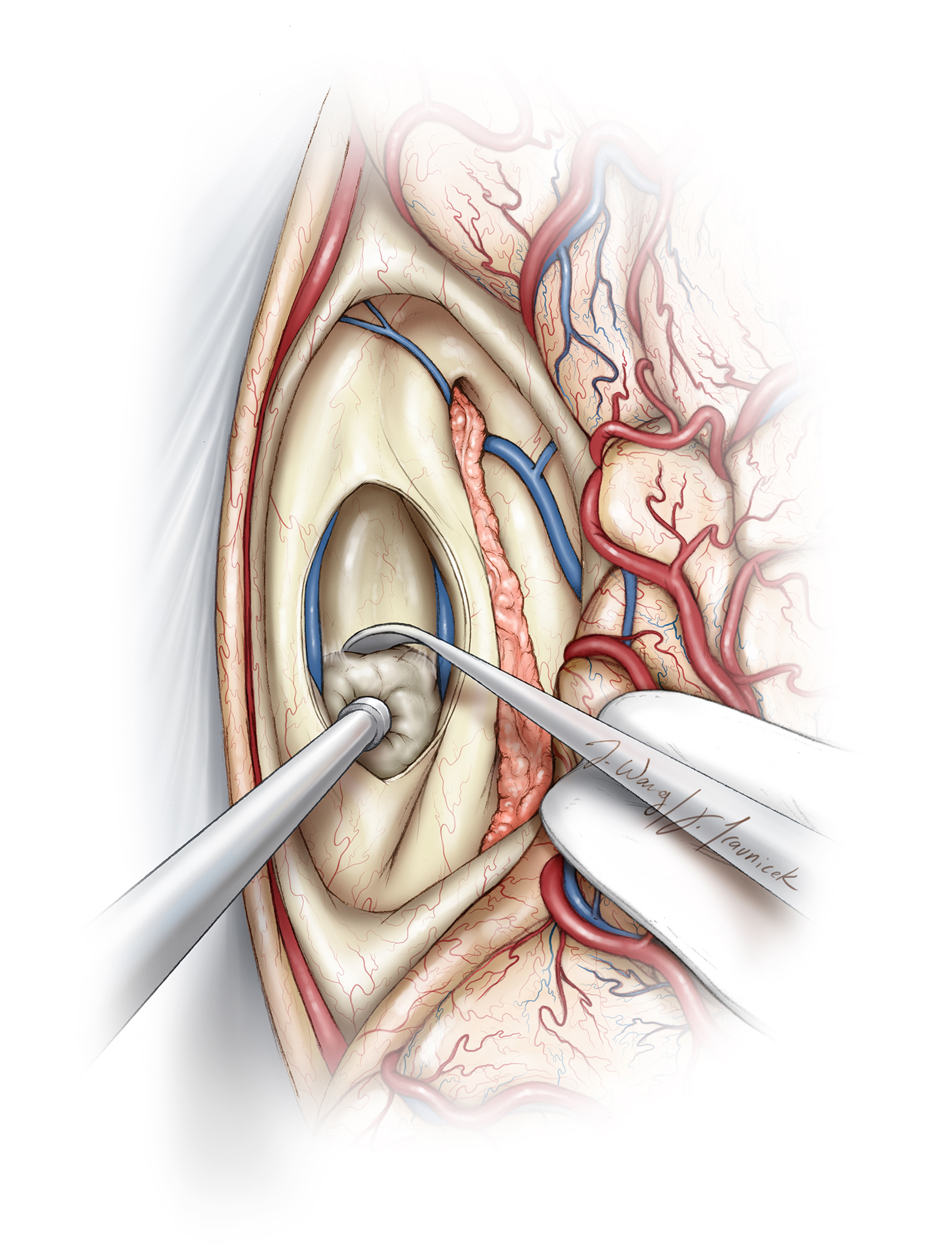
Figure 10: The internal cerebral veins are left encased in tenia choroidea and gently mobilized laterally. This maneuver isolates the tumor capsule. I cover the internal cerebral veins with soft, nonadherent, small cotton patties to prevent their desiccation. Their manipulation is kept to a minimum to prevent their occult thrombosis. If the tumor is adherent to one vein, an arachnoid knife is used to cut the tumor capsule slightly away from and parallel to the vein, leaving a thin sheet of tumor over the vein (Redrawn from Tew, van Loveren, Keller*).
Figure 11: I use standard microsurgical techniques to debulk the tumor and then dissect it along its anterior, lateral, and posterior capsule planes. I avoid using fixed retractor blades, no matter how small, in the ventricle (Redrawn from Tew, van Loveren, Keller*).
Figure 12: I often place a small cottonoid patty at the floor to prevent dispersion of the debris, especially if a shunt is in place. At this point, I can usually separate the tumor from the pial-arachnoid boundary around the tectal plate and superior cerebellum. Larger tumors invade the tectum, and gross total resection of the mass exposes the fourth ventricle. A distinct arachnoid plane separates the vein of Galen from the tumor capsule (Redrawn from Tew, van Loveren, Keller*).
After the tumor has been removed, I use angled mirrors or endoscopes to inspect the operative blind spots for residual tumor that may lie just below the splenium, under the edges of the corpus callosum, or under the folds of the surrounding tissues and veins.
Figure 13: The expansive reach of the posterior interhemispheric transcallosal intervenous/paravenous variant (green shaded area) is shown. The subsplenial and subcallosal blind spots may be examined with a mirror or an endoscope. Since the callosotomy is made anterior to the splenium, an acute working angle is required to dissect around the subsplenial area or around the venous confluence located ventral to the splenium.
Paravenous-Interforniceal Variant for a Paramedian Pathology
Figure 14: Intra-axial or exophytic lesions that arise from the posterior thalamus may be reached via the paravenous variant of the above approach. This ganglioglioma was approached via this route.
Using navigation, I incise the corpus callosum in the paramedian plane, directly over the pole of the tumor near the lateral ventricle. Preoperative MRI allows me to reliably identify the course of the fornix, internal cerebral veins, and the available operative trajectory.
Normal ependyma may or may not cover the capsule of the tumor. Intratumoral debulking mobilizes the tumor into the resection cavity while dissection progresses from a lateral to a medial direction. The internal cerebral veins may have been displaced by the tumor to the contralateral side over the capsule, or they may course through the tumor.
If these veins are over the capsule, I can debulk the tumor more rapidly. However, I regularly reconfirm the exact location of the veins with extracapsular dissection and direct visualization.
When the veins are engulfed by the tumor, only a debulking procedure is completed, based on the route of the veins within the mass. In these cases, aggressive tumor removal is not advised because its risks outweigh its benefits.
Closure and Postoperative Considerations
For a detailed discussion of recommendations for closure and the postoperative care of patients with ventricular tumors, see the Principles of Intraventricular Surgery chapter.
Case Example
The following case describes the operative events for removal of a recurrent large posterior third ventricular epidermoid via the posterior interhemispheric transcallosal intervenous route.
Figure 15: This young patient presented with progressive hemiparesis and was found to have a recurrent large posterior third ventricular epidermoid tumor reaching the pineal region and the superior medullary velum. The right upper image demonstrates the route of the internal cerebral vein.
Figure 16: A right-sided posterior interhemispheric approach was undertaken for resection of the mass described in the prior figure (Figure 15). Patient positioning is illustrated. The neck is tilted away from the floor ~45 degrees. Some colleagues prefer the neutral head positioning with the patient in the supine position as described in the previous illustrations of the current chapter; this head configuration maintains the anatomic relationship of the cerebrovascular structures and readily orients the operator to the deep structures. On the other hand, the lateral head position (top photos) exploits gravity retraction to mobilize the ipsilateral hemisphere away from the midline (second image). An incision within the affected splenium immediately exposed the tumor (third row). The intervenous variant of this approach was necessary; the right internal cerebral vein was identified (blue arrow). I transected the falx to expand the working trajectory toward the contralateral third ventricle (fifth row). During tumor removal, the fourth ventricle was apparent (bottom image). Please see the video at the beginning of this chapter for further details.
The Posterior Interhemispheric Subsplenial/Transsplenial Route
This approach is rarely employed but is worth mentioning so that it can be considered when the venous anatomy is favorable. This approach is reasonable for more posteriorly and superiorly located targets that separate the internal cerebral veins and provide a wide a intervenous corridor. After the interhemispheric approach is complete, the edge of the splenium is moblized and the tumor is brought into view. If the splenium is very attenuated by the tumor, it may be partially transected to expand the operative working space.
Figure 17: The splenium is mobilized and gently retracted to bring the lesion into view (Top). Alternatively, a small but affected portion of the splenium may be transected for reaching a more anterior lesion that primarily resides within the splenium (bottom).
Pearls and Pitfalls
- The posterior interhemispheric transcallosal intervenous/paravenous approach is reasonable for exposure of large posterior third ventricular lesions that displace the deep veins posteriorly. The applications of this approach are limited.
Contributors: Frederick A. Boop, MD and Paul Klimo Jr., MD, MPH
*Redrawn with permission from Tew JM, van Loveren HR, Keller JT. Atlas of Operative Microneurosurgery, WB Saunders, 2001. © Mayfield Clinic
Please login to post a comment.