Epidural Hematoma (EDH)
Figure 1: The left middle cranial fossa biconvex hyperdense epidural hematoma on axial CT (left) is likely secondary to middle meningeal artery injury, usually associated with fracture of the temporal bone in the same area, visible in this patient as nondisplaced fracture on bone window axial CT (right). A small amount of subarachnoid blood is also visible in the interpeduncular cistern (left, arrow).
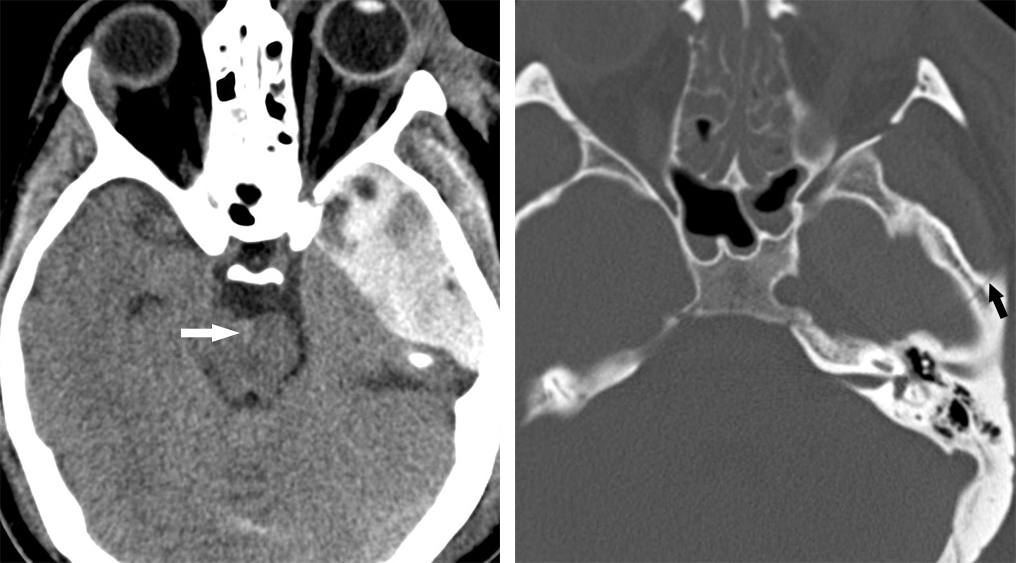
Figure 2: Brain window/level Axial CT (left) through the posterior fossa demonstrates a biconvex epidural hematoma superficial to the right cerebellar hemisphere. Bone window at the same level (right) exhibits an associated overlying nondisplaced fracture of the right occipital bone near the lambdoid suture.
- Hemorrhagic collection within the epidural space, located between the inner table of the skull and parietal layer of dura mater and usually demonstrate associated skull fracture
- Rapid accumulation of blood (within 36 hours), as 95% of cases are due to arterial bleeds
- Location
- 95% are supratentorial - 2/3 in the temporoparietal region (usually due to middle meningeal artery injury) and 1/3 in the parietooccipital region. (See Figure 1)
- 5% infratentorial in the posterior fossa (See Figure 2)
Neuroimaging
- Morphology
- Biconvex (lentiform) collection
- Arterial bleeds do not cross sutures (exceptions are presence of sutural diastasis or calvarial fracture)
- Venous epidural hematomas are much less common
- Often due to fractures that cross sutures
- Hematoma may straddle sutures, dural attachments and may cross falx cerebri or tentorium cerebelli.
- May compress or displace underlying brain, subarachnoid space.
- May cause secondary herniations
- Modalities
- CT without contrast with bone CT algorithm is the primary imaging of choice for trauma
- MRV or MRI obtained if venous EDH suspected
- MRI if hematoma straddles dural sinuses or dural compartments
- CT Findings
- CT without contrast
- Biconvex (lentiform) extraaxial collection with a medial hyperdense displaced dura
- Acute hematoma - Hyperdense 2/3 of the time and of heterogenous density 1/3 of the time;
- Chronic hematoma – Hypodense or Heterogenous density
- An active bleed during scan may show a low-density "swirl" sign with non-clotted lower density fresh blood
- CT Comma sign
- Frontoparietal EDH (head of the comma)
- Temporoparietooccipital SDH (tail of the comma)
- These two extra-axial hemorrhagic lesions are treated as two separate surgical entities
- CT with contrast
- Acute may rarely show contrast extravasation
- Chronic shows peripheral dural enhancement from neovascularization/granulation
- Bone CT – 95% of the cases show skull fracture
- CT without contrast
- MRI Findings
- Hyperacute (<12 hours), intracellular oxyhemoglobin
- T1WI: Isointense to brain
- T2WI: Hyperintense to brain
- Acute (1-3 days), intracellular deoxyhemoglobin
- T1WI: Isointense to brain
- T2WI: Hypointense to brain
- Early subacute (3 -6 days), intracellular methemoglobin
- T1WI: Hyperintense to brain
- T2WI: Hypointense to brain
- Late subacute (7-14 days), extracellular methemoglobin
- T1WI: Hyperintense to brain
- T2WI: Hyperintense to brain
- Chronic >14 days, Ferritin and Hemosiderin
- T1WI: Hypointense to brain
- T2WI: Hypointense to brain
- T2*GRE: Markedly Hypointense
- FLAIR: At least mildly hyperintense to CSF
- Contrast: Peripheral dural enhancement from neovascularization/granulation
- Venous origin of EDH – displaced or occluded dural venous sinus on T1 weighted post contrast images and on MR venography
- Hyperacute (<12 hours), intracellular oxyhemoglobin
- Angiography Findings
- The hematoma appears as an avascular region with mass effect and displaced cortical arteries
- Lacerated middle meningeal artery
- If forming an AV fistula, Tram-track sign with simultaneous opacification of artery and vein
- Displaced dural sinus in venous EDH
- Differential diagnosis
- Acute Subdural Hematoma (aSDH)
- Neoplasms including meningioma, dural based metastasis, lymphoma, sarcoma
- Infection/Inflammation including epidural empyema, granulomatous osseous TB
- Extramedullary Hematopoiesis in blood dyscrasia
For more information, please see the corresponding chapter in Radiopaedia.
Contributor: Priya Rajagopalan, MD
Please login to post a comment.