Pineal Region Tumor (Occipital Transtentorial Approach)
For general considerations, diagnosis and evaluation, indications for surgery, and preoperative considerations, please refer to the Pineal Region Tumor (Infratentorial Supracerebellar Approach) chapter.
For the occipital transtentorial route, preoperative magnetic resonance venogram or computed tomography venogram may be considered to locate the bridging veins in the parasagittal occipital region.
The occipital transtentorial approach enters the cranial vault through a unilateral occipital craniotomy. This approach offers wide exposure of the quadrigeminal plate and is particularly useful for large pineal region tumors that extend laterally and inferiorly. This approach is especially favorable for reaching lesions arising from the precentral cerebellar fissure, posterior incisural space, and adjacent structures.
Multicompartment lesions that occupy the pineal region and extend into the posterior thalamus, lateral ventricle, medial temporal lobe, and over the corpus callosum require expanded working angles and may benefit from the use of the occipital transtentorial route. Masses that expand into the depth of the precentral cerebellar fissure and toward the roof of the fourth ventricle are especially reasonable targets for this approach.
Arteriovenous malformations involving the splenium and pineal region can be widely exposed via this approach; early access to the feeding vessels from the posterior cerebral artery is possible without placing the draining veins that join the Galenic system at risk.
The lateral variant of this approach mobilizes the occipitotemporal junction and provides excellent exposure of the posterolateral brainstem, thalamus, and medial temporal lobe. This variant also provides flexible operative working angles under the diencephalic venous system near the precentral cerebellar fissure and fourth ventricular roof/superior cerebellar velum. The interhemispheric variant readily exposes lesions near and superior to the splenium, atrium, velum interpositum, third ventricle, and medial thalamus.
The drawbacks of the occipital transtentorial approach include difficulty with anatomic orientation, the need to divide the tentorium (working around the veins of the deep venous system), and the possibility of a homonymous hemianopsia from occipital lobe retraction. The risk of visual field deficits is minimized by directing the operative trajectory under the occipitotemporal junction or by directing the trajectory along the interhemispheric corridor.
In my opinion, the occipital transtentorial approach is a cumbersome approach that can place numerous normal structures at risk. On the other hand, the paramedian supracerebellar approach and its transtentorial variant are very practical and flexible opportunities for exposing relatively similar operative regions within the precentral cerebellar fissure. However, the occipital transtentorial approach is a reasonable option if the tumor has displaced the deep veins caudally or posteriorly, precluding a safe reach via the infratentorial supracerebellar approach.
Operative Anatomy
The precentralfissure or cerebellomesencephalic fissure is generously exposed via the occipital transtentorial corridor. This space is marked anteriorly by the superior cerebellar peduncles, lingula of the vermis over the superior medullary velum, proximal trochlear nerve, and the quadrigeminal plate, in addition to the pineal body. The roof of this space contains the vein of Galen, splenium, hippocampal commissure, pulvinar, fornix, and parahippocampal gyri. These regions have been traditionally reached via the infratentorial supracerebellar approach.
Click here to view the interactive module and related content for this image.
Figure 1: The steps for the occipital transtentorial approach are shown. Note the panoramic view of the pineal region and the expanded superior-to-inferior operative trajectory (Images courtesy of AL Rhoton, Jr).
Figure 2: A magnified view of the occipital transtentorial approach toward the pineal region and the deep veins is illustrated.
PINEAL REGION TUMOR (OCCIPITAL TRANSTENTORIAL APPROACH)
Patient positioning in a three-quarter prone or lateral position is beneficial for exploiting gravity retraction on the nondominant/ipsilateral occipital lobe. I plan some form of cerebrospinal fluid drainage in advance (either lumbar drain or an external ventricular drain).
Figure 3: A paramedian linear or U-shaped right occipital scalp flap is completed. The medial vertical limb of the U-shaped flap starts to the left of the midline near the torcula. Two or more burr holes over the superior sagittal sinus and torcula facilitate atraumatic elevation of the bone flap that partially unroofs the width of these dural venous sinuses. Lumbar cerebrospinal fluid drainage assists with dural sac and brain relaxation.
INTRADURAL PROCEDURE
Figure 4: Please note the cruciate pattern of the dural incisions. Interhemispheric dissection exposes the straight sinus so that the tentorium can be divided adjacent to it (~1cm away from it). A small nonsignificant parasagittal vein may have to be sacrificed. The inferior sagittal sinus and falx may be divided to facilitate further transfalcine exposure. Direct retraction force on the primary visual cortex is avoided. The occipitotemporal junction is mobilized for lesions near the posterolateral mesencephalon. If the lesion is close to the midline, the interhemispheric space is the focus of the operative corridor. A portion of the tentorium is resected to allow adequate exposure of the lesion. Importantly, the trochlear nerve is mobilized from the tentorial edge before the edge is manipulated.
Importantly, the tentorium is transected in the posterior to anterior direction. The initial portion of the incision is created just anterior to the junction of the torcula and the straight sinus. This incision is extended to the level of the incisura. Retention sutures can mobilize the tentorium laterally and posteriorly, obviating the need for transecting a window in the tentorium. Bleeding from the tentorium is controlled via bipolar coagulation and thrombin soaked gelfoam packing of the venous lakes within the leaflets of the tentorium.
Figure 5: Now the arachnoid bands overlying the tumor and the quadrigeminal cisterns can be seen froma supraposterior perspective. These bands are dissected; the tumor and the adjacent cerebrovascular structures, including the deep diencephalic veins (basal veins and the vein of Galen) are identified early to keep them out of harm's way. A fixed retractor blade "holds" the occipital lobe, but does not retract it. Alternatively and preferably, cotton balls may be used to hold the lobe in place and away from the tentorium.
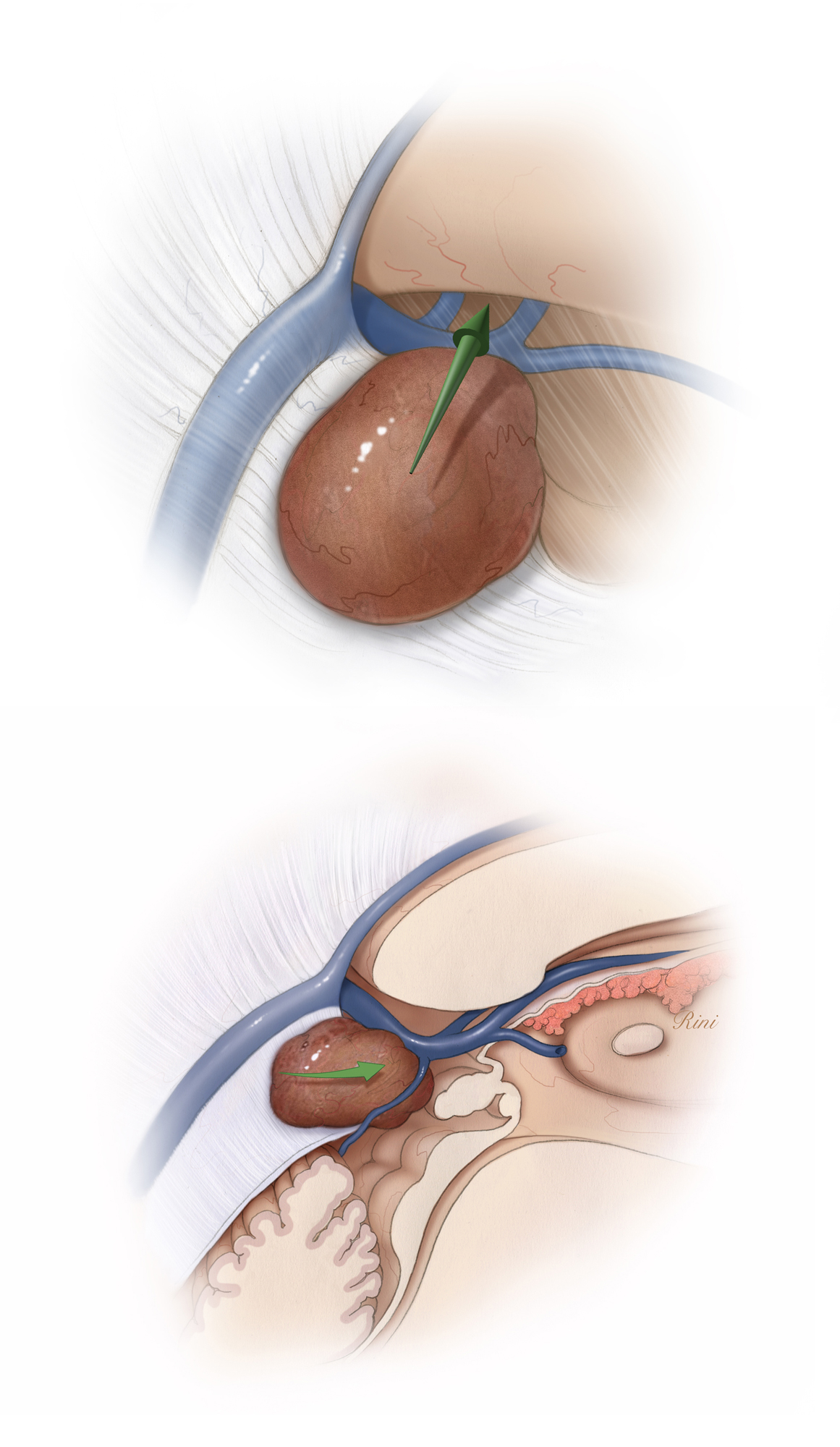
Figure 6: A typical location of a large pineal region tumor and the variations in the displacement of the deep veins are illustrated. The precentral cerebellar vein is coagulated, allowing the vermis to be mobilized away from the operative corridor.
Figure 7: The deep venous anatomy in relation to the tumor is further illustrated. Note that the displacement of the deep veins posteriorly complicates the use of the infratentorial supracerebellar approach.
Figure 8: However, if the deep veins are displaced dorsally (top image) or anteriorly (bottom image), the infratentorial supracerebellar approach is favored.
The tumor generally guides the surgeon as the surgeon dissects its boundaries. If the tumor is invading the medial temporal lobe or the associated ventricles, the choroidal fissure may be split for adequate exposure of the mass. Any tumor adherent to the veins is subtotally removed.
Closure and Postoperative Considerations
The closure and postoperative considerations are discussed in the Pineal Region Tumor (Infratentorial Supracerebellar Approach) chapter. I usually do not place any sutures to reapproximate the tentorium.
Pearls and Pitfalls
- The occipital transtentorial approach is utilized selectively for tumors arising from the precentral cerebellar fissure, posterior incisural space, and adjacent structures. This approach is favored if the deep veins are displaced posteriorly and caudally.
- Multicompartmental lesions that occupy the pineal region and extend into the posterior thalamus, lateral ventricle, medial temporal lobe, and over the corpus callosum are reasonable candidates.
References
Moshel YA, Parker EC, Kelly PJ. Occipital transtentorial approach to the precentral cerebellar fissure and posterior incisural space. Neurosurgery. 2009;65:554-564.
Please login to post a comment.