Cerebritis/Abscess
Abscesses begin as focal areas of infected brain called cerebritis, which may result from direct spread (commonly iatrogenic or from mastoiditis, sinusitis, or meningitis) or from hematogenous spread. There are four characteristic zones of an abscess that include a cavity of central necrosis, a capsule composed of fibroblasts, reticulin and collagen, peripheral edema, and areas of extraparenchymal spread (meninges, ventricles, CSF spaces, bone, blood vessels).
Imaging Features
There are 4 stages of brain infection between cerebritis and abscess, which are as follows:
- Early cerebritis
- Late cerebritis
- Early capsule
- Late capsule
The lesions are either located near extra-axial infection or at common sites of hematogenous spread that are usually supratentorial, usually in the anterior circulation (ACA and MCA), and usually at the grey-white matter junctions and basal ganglia.
The most distinguishing characteristics of abscesses are peripheral enhancement around a cavity of central necrosis and pus. Without further information, however, the finding of solitary or multiple ring-enhancing lesions is not specific and the differential diagnosis is broad, including neoplasms, demyelinating disorders, other infections, and subacute insult to the brain parenchyma like contusion or stroke.
- CT:
- Early cerebritis
- Ill-defined low-density area
- Possible patchy enhancement
- Late cerebritis
- Ill-defined low-density area with mass effect
- Subtle ring-like enhancement PLUS persistent central enhancement
- Early capsule
- Discrete low-density lesion with mass effect and surrounding ill-defined low-density of the brain tissue reflecting edema
- Discrete ring-like enhancement of the capsule
- Late capsule
- Decreasing size of the low-density mass and decreasing mass effect
- Decreasing hypodense surrounding edema
- Thickening of the enhancing capsule but decreased size of the cavity
- Possible development of satellite abscesses
- Early cerebritis
- MRI:
- Early cerebritis:
- T1: Ill-defined area of decreased signal
- T2/FLAIR: Ill-defined area of increased signal
- DWI/ADC: increased signal on both (edema, NOT restricted diffusion)
- T1 post-contrast: Patchy enhancement
- Late cerebritis:
- T1: low signal center, iso-intense rim
- T2: high signal center, hypointense rim (presumed to be due to high concentration of free oxygen radicals causing local disruption of the magnetic field and loss of signal)
- FLAIR: increased signal within and surrounding the lesion
- DWI/ADC: increased signal within and surrounding the lesion on both (edema, transitioning to restricted diffusion)
- T1 post-contrast: irregular rim enhancement
- Early capsule:
- T1: Discrete iso- to hyperintense rim, low signal center
- T2: High signal center, low-signal rim, surrounding high signal of edema
- FLAIR: Increased signal within and surrounding the lesion
- DWI/ADC: Central increased DWI signal and decreased ADC signal (restricted diffusion due to high degree of cellular debris – bacteria and inflammatory response cells).
- T1 post-contrast:
- Thin, avidly enhancing rim, absent central enhancement (necrotic center).
- The ventricular side of the capsule is often thinner and more prone to rupture, allowing for the development of satellite abscesses and intraventricular extension. The cause is felt to be relatively poorer blood flow and poorer fibroblast migration from the deep white matter.
- Typical findings of ventriculitis include intraventricular restricted diffusion, intraventricular debris (incomplete suppression of the CSF fluid signal on FLAIR sequence), periventricular edema and enhancement of the ventricular walls (usually mild and thin).
- MR spectroscopy: Central necrosis shows increased lactate and amino acids.
- Late capsule:
- T1: Thicker capsule, decreased size of the cavity
- T2/FLAIR: decreased surrounding edema
- DWI/ADC: Persistent restricted diffusion in the necrotic center (high DWI, low ADC), decreased surrounding edema (high DWI and high ADC)
- T1 post-contrast: Thick enhancing capsule, decreased size of the non-enhancing central cavity
- Early cerebritis:
- Nuclear Medicine:
- PET:
- Abscesses show peripheral uptake of F-18 fluorodeoxyglucose and C-11 methionine.
- PET:
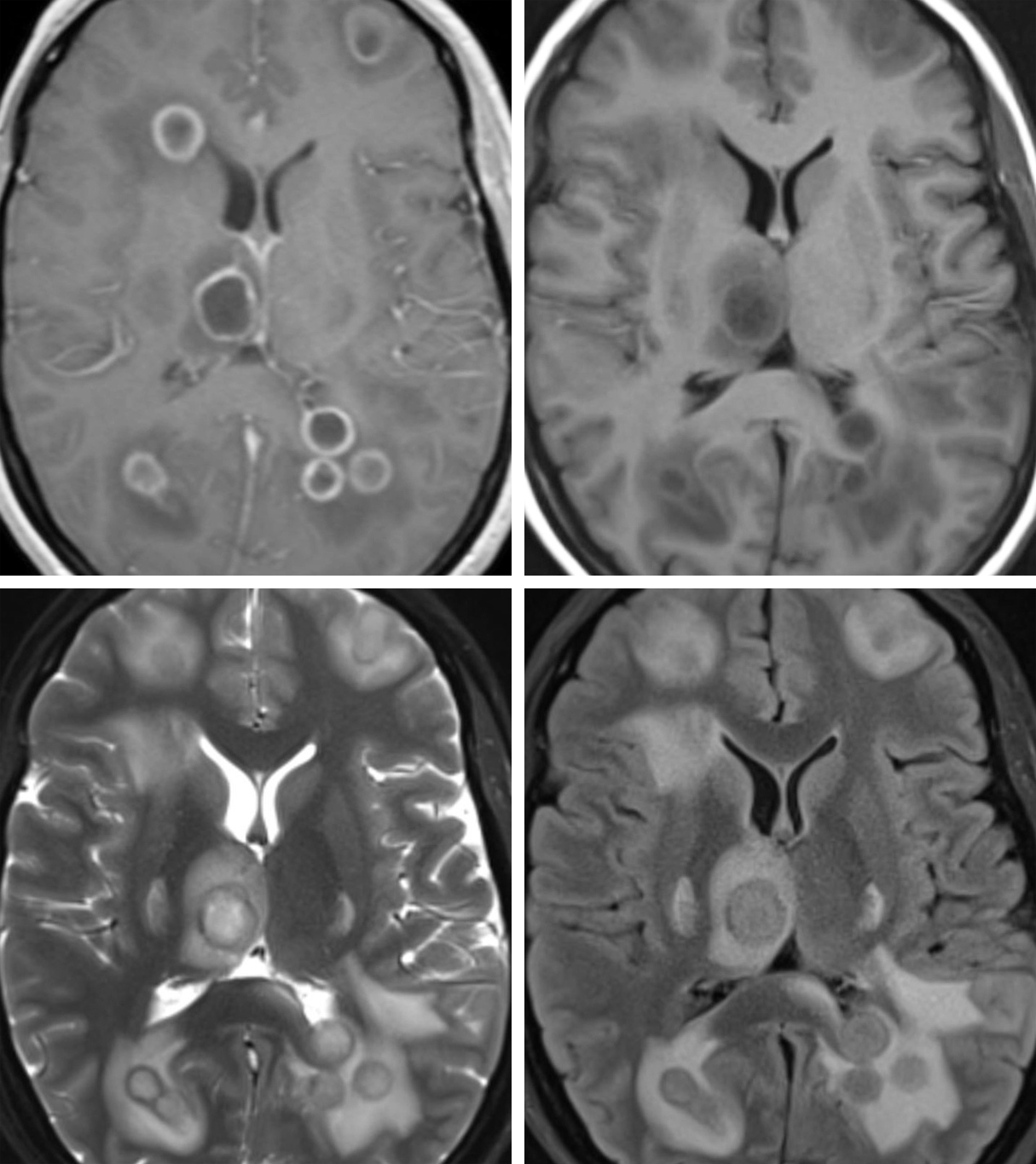
Figure 1: Post-contrast T1 weighted image (top row left) demonstrates multiple supratentorial ring-enhancing lesions with a thin capsule consistent with Early Capsule stage. Not shown here – the side of the capsule that is nearest a ventricle is often thinner, making it prone to rupture with intraventricular extension causing life-threatening ventriculitis or development of satellite abscesses. Prior to the administration of contrast, the abscesses (top row right) are less conspicuous, only visible as hypointense lesions with slightly less dark surrounding edema. The capsule itself is often mildly hyperintense. The T2-weighted image (bottom row left) from this same patient illustrates the high signal-intensity necrotic center and high-signal surrounding vasogenic edema typical of abscesses. The capsule is low signal, which is believed to be due to alteration of the local magnetic field by high concentrations of oxygen free radicals. The findings on FLAIR (bottom row right) are similar to those on T2: high signal necrotic center and surrounding vasogenic edema. Not shown here – Spread of infection into the ventricles or extra-axial CSF spaces may result in incomplete suppression of fluid signal leading to subtly abnormally increased signal of the intraventricular CSF.
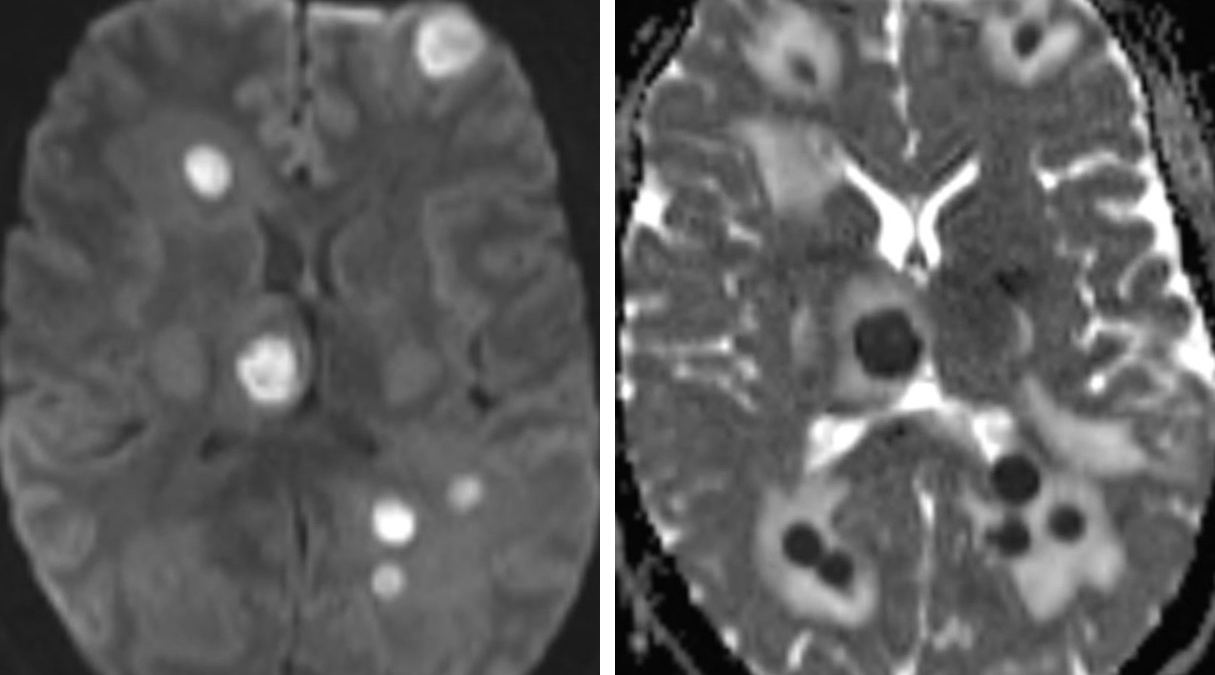
Figure 2: The necrotic center of an abscess is highly cellular, likely contributing to the restricted diffusion of water leading to characteristic high central DWI signal (top row left) and low ADC signal (top row right). In contrast, perilsional vasogenic edema appears as increased ADC signal.
Figure 3: F-18 fluorodeoxyglucose (FDG) PET/CT with intravenous contrast: Multiple ring-enhancing lesions with perilesional low-density edema are visible on CT (top row left). On PET (top row right), only the right thalamus lesion is definitely seen, which appears as a ring of increased radiotracer uptake (coded as red/pink in this color scheme). Lesions smaller than about 7 mm may not generate adequate PET signal to be visible.
Differential Diagnosis
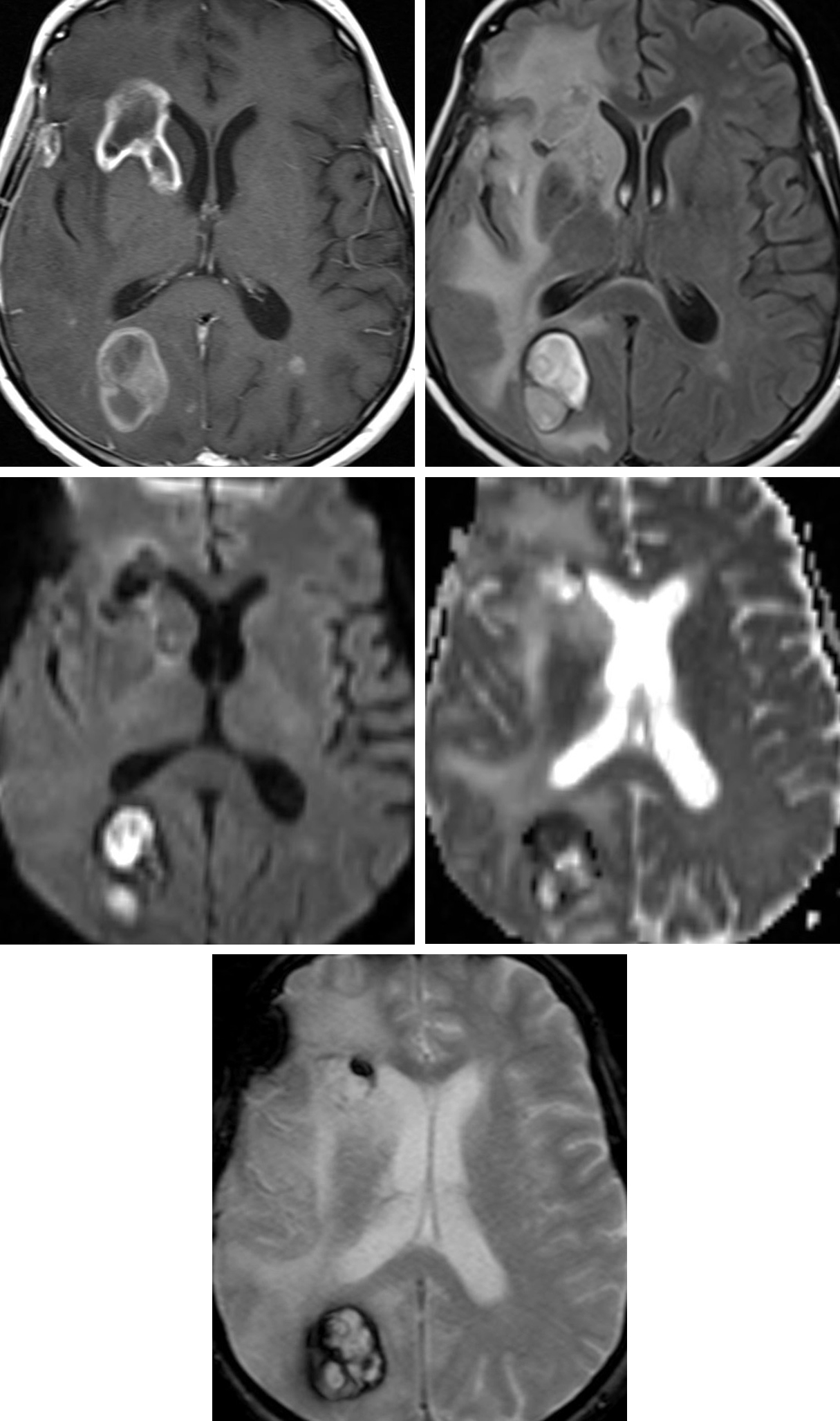
Figure 4: Metastases mimicking abscess. A poorly-differentiated lung adenocarcinoma on Chest CT (top row left) progressed to cerebral metastatic disease. Metastatic lesions often have a ring-enhancing pattern on T1 post-contrast sequence (top row right) that is very similar in appearance to abscesses. The surrounding hyperintense edema on FLAIR (bottom row) is also usually visually indistinguishable from that of abscess. Metastases usually do not have the restricted diffusion much more typical
Figure 5: Multifocal Glioblastoma mimicking abscess. Multiple ring-enhancing lesions on T1 post-contrast image (top row left) demonstrate surrounding hyperintense edema on FLAIR (top row right) and restricted diffusion on DWI (middle row left) and ADC (middle row right) that is very similar to abscess. The presence of GRE hypointensity (bottom row) gives us a clue that the restricted diffusion is actually from hemorrhage. Other anatomic and distribution-pattern clues are also usually present to help distinguish abscess from GBM.
- Infarct (subacute infarcts can present as nodular or ring-enhancing lesions with restricted diffusion, mimicking cerebritis or abscess, as in this case of infarct in the left corona radiata)
Figure 6: If imaged in the early subacute stage, an infarct may easily mimic pyogenic abscess, particularly in the setting of lacunar infarcts. As in this left corona radiata lacunar infarct, these often demonstrate enhancement on T1 post-contrast images (top row left) and persistent mild restricted diffusion on DWI (top row right) and ADC (bottom row).
- Atypical Infections (neurocysticercosis, cryptococcosis, toxoplasmosis, tuberculosis and many others) and this case, which is tuberculous meningitis with intraparenchymal extension in the inferior frontal lobes that presents as multiple, cystic ring-enhancing lesions, but these do not cause restricted diffusion)
Figure 7: Tuberculous meningitis in the basal cisterns extends into the cerebral parenchyma and demonstrates a ring-enhancing pattern on T1 post-contrast image (left), but these lesions have no restricted diffusion on DWI (right) that is nearly always present in pyogenic abscesses. This is a common useful differentiating feature for atypical infections.
- Cerebral Parenchymal Contusion
- Primary CNS lymphoma, particularly in the immunocompromised setting
- Demyelinating disease
Figure 8: This patient’s distributions of FLAIR hyperintense lesions (top row left) is very typical for multiple sclerosis. One of these lesions demonstrates a rim of enhancement on T1 post-contrast image (top row right) indicating active demyelination. These lesions often demonstrate an incomplete rim of enhancement, a helpful differentiating feature from abscess. Diffusion restriction that is almost always present in abscess is nearly always absent in the center of demyelinating lesions.
- Radiation necrosis
Figure 9: New peripherally enhancing lesions on coronal T1 post-contrast images (top row) appeared several months after resection of oligodendrogioma with subsequent radiotherapy. The lesions slowly resolved within 3 months, a temporal pattern most compatible with radiation-induced injury. This iatrogenic insult may also mimic pyogenic abscess, particularly when restricted diffusion is present within the lesion. On DWI image (bottom row), this patient’s necrosis demonstrated no restricted diffusion (arrows).
Contributor: Jordan McDonald, MD
References
Enzmann DR, Britt RH. Clinical staging of human brain abscesses on serial CT scans after contrast infusion: Computerized tomographic, neuropathological, and clinical correlations. J Neurosurg. 1983; 59: 972-989.
Fukui MB, Williams RL, Mudigonda S. CT and MR imaging features of pyogenic ventriculitis. AJNR Am J Neuroradiol 2001;22(8):1510–1516.
Haimes AB, Zimmerman RD, Morgello S, et al. MR imaging of brain abscesses. AJR Am J Roentgenol. 1989; 152: 1073-1085.
Lai PH, Chang HC, Chuang TC, et al. Susceptibility-weighted imaging in patients with pyogenic brain abscesses at 1.5T: characteristics of the abscess capsule. AJNR Am J Neuroradiol 2012;33(5):910–914.
Mishra AM, Gupta RK, Saksena S, et al. Biological correlates of diffusivity in brain abscess. Magn Reson Med 2005;54(4):878–885.
Pal D, Bhattacharyya A, Husain M, Prasad KN, Pandey CM, Gupta RK. In vivo proton MR spectroscopy evaluation of pyogenic brain abscesses: a report of 194 cases. AJNR Am J Neuroradiol 2010;31(2):360–366.
Rath TJ, Hughes M, Arabi M, Shah GV. Imaging of cerebritis, encephalitis, and brain abscess. Neuroimaging Clin N Am 2012;22(4):585–607.
Shih RY, Koeller KK. Bacterial, fungal, and parasitic infections of the central nervous system: Radiologic-pathologic correlation and historical perspectives. Radiographics. 2015; 35(4): 1141-1169.
Tsuyuguchi N, Sunada I, Ohata K, et al. Evaluation of treatment effects in brain abscess with positron emission tomography: Comparison of fluorine-18-fluordeoxyglucose and carbon-11-methionine. Annals of Nuclear Medicine. 2003; 17(1): 47-51.
Please login to post a comment.