Selection of Operative Corridor Free
Figure 1: The man in this photograph, a patient of Harvey Cushing’s, suffered from Parinaud’s syndrome and died before a diagnosis and tumor localization was made. The autopsy specimen (right photo) demonstrates a tumor located in the pineal region (images courtesy of Cushing Brain Tumor Registry at Yale University).
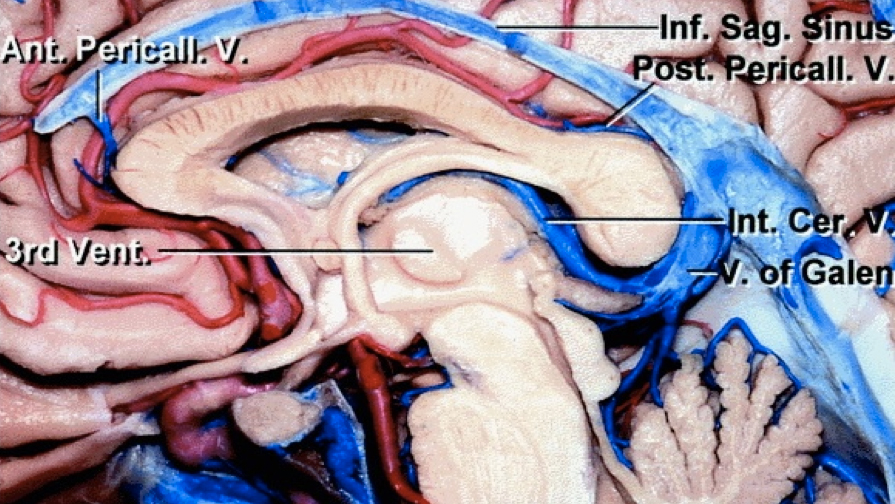
The pineal region is located deep within the center of the cranial vault and consists of the pineal gland and adjacent structures. Although there are no clear-cut boundaries for the pineal region, it is surrounded superiorly by the splenium of the corpus callosum, posteriorly by the vein of Galen, inferiorly by the quadrigeminal cistern and tectum, and anteriorly by the pineal recess and the posterior third ventricle.
Each of these structures can be subject to mass effect from tumors in the pineal area. Importantly, the aqueduct of Sylvius, just anterior to the tectum, may be affected by the tumor’s mass effect, resulting in obstructive hydrocephalus, which usually accounts for most of the presenting symptoms of these tumors.
Click here to view the interactive module and related content for this image.
Figure 2: Midline sagittal view of the pineal region. Note the location of the structures adjacent to the pineal gland (image courtesy of AL Rhoton, Jr).
A wide variety of pathologies occur in the pineal region, including germ cell tumors, parenchymal tumors of the pineal gland, glial cell tumors, and less commonly, meningiomas, lipomas, epidermoids, dermoids, pineal cysts, and vascular lesions.
The types of tumors found in the pineal region vary widely in their appropriate treatment strategy, ranging from nonoperative management to gross total resection, but these lesions are difficult to accurately diagnose radiographically.
The deep location of the pineal region and its adjacent vital neurovascular structures, the heterogeneity of possible pathologies, and the difficulty of reliable preoperative diagnosis all make tumors of the pineal region uniquely challenging entities to surgically manage while consistently maintaining a low morbidity risk.
Presentation
Patients with pineal region tumors commonly present with symptoms of elevated intracranial pressure secondary to obstructive hydrocephalus, including headaches, visual and cognitive disturbances, and impaired gait.
Patients may also present with Parinaud’s dorsal midbrain syndrome, which includes upgaze palsy, eyelid retraction, convergence nystagmus, and light-near dissociation. Symptoms of acute hydrocephalus, such as sudden loss of consciousness, may occur and require emergent cerebrospinal fluid (CSF) diversion.
About half of the patients with these tumors present with signs of cerebellar dysfunction, such as ataxia, from their direct mass effect on the cerebellum. About 10% of patients with germ cell tumors have concurrent lesions in the suprasellar area resulting in pituitary dysfunction, and may rarely present with sleep-awake cycle disturbances and psychosis.
Evaluation
If the patient presents acutely with mental status changes such as obtundation, a computed tomography (CT) scan is obtained to evaluate the extent of hydrocephalus. Immediate CSF diversion in the form of an external ventricular drain (EVD) may be necessary.
If the patient presents electively, evaluation begins with a thorough history and comprehensive physical and neurologic exam, with particular attention to the function of the pupils, extraocular muscles and the cerebellum.
Imaging studies include magnetic resonance (MR) imaging with and without gadolinium enhancement. MR venography (MRV) is helpful in assessing the tumor’s mass effect on the deep venous drainage systems, including their direction of displacement and patency; both factors are important considerations for surgical planning.
Unfortunately, imaging alone is insufficient for offering a reliable diagnosis for tumors such a germinomas that can be managed nonoperatively. Laboratory measurement of CSF levels of beta-human chorionic gonadotropin (beta-hCG), alpha-fetoprotein (AFP), and placental alkaline phosphatase (PLAP) can help diagnose germ cell tumors and prevent unnecessary attempts at biopsy/resection and their attendant morbidity. For non-germ cell tumors, optimal management is impossible without tissue diagnosis. For more information about these CSF markers, please refer to the chapter on Pineal Region Tumors.
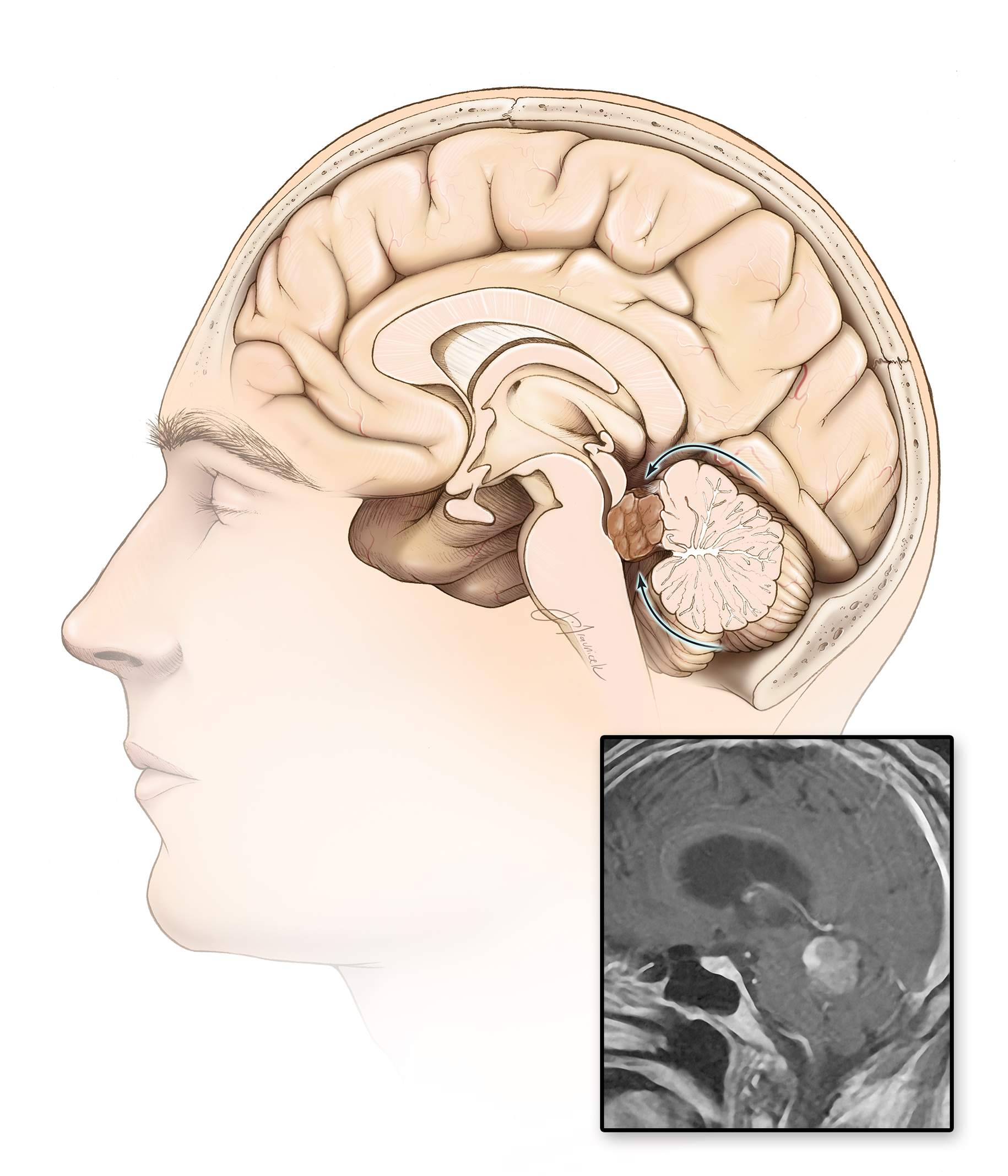
Figure 3: Different tumor subtypes in the pineal region are demonstrated. The top images show a germinoma in a young boy; the middle images belong to an adult patient with a pineoblastoma; and the bottom images show a hemorrhagic pilocytic astrocytoma. Note that in the images of the bottom row, the deep diencephalic veins are paradoxically displaced posteriorly (blue arrow). This important preoperative finding will affect the choice of operative approach and intraoperative dissection methodology. If the operator does not recognize this unusual location of the veins, the risk of injury to the veins during exposure and dissection is significant. The imaging similarities between the tumors in the top two rows prevent any reliable preoperative diagnosis without adjuvant diagnostic tools.
Management Strategies
The initial treatment of pineal region tumors may include CSF diversion because acute obstructive hydrocephalus is one of the common presenting symptoms. Urgent management of symptomatic hydrocephalus is accomplished by bedside ventriculostomy.
Definitive treatment of hydrocephalus favors endoscopic third ventriculostomy (ETV) over ventriculoperitoneal shunting (VPS), especially in younger patients with long life expectancies, because ETV enables the patient to avoid many of the potential complications associated with VPS including the risk of peritoneal seeding of malignant cells. Mildly symptomatic hydrocephalus or asymptomatic ventriculomegaly may not require treatment because tumor resection facilitates their resolution by reconstituting the CSF pathways.
Definitive treatment of pineal region tumors varies according to pathology. Approximately one-third of these tumors are benign and therefore potentially surgically curable via gross total resection. Conversely, germinomas are highly radiosensitive and resection is not warranted.
Tissue sampling or other similar diagnostic tools such as CSF analysis is necessary to confirm the need for gross total resection and, more importantly, to avoid the risks of this procedure altogether. There is no uniformly accepted protocol for the evaluation and management of pineal region tumors.
Many surgeons prefer an initial biopsy, followed by gross total resection if indicated by tumor pathology. This methodology prevents an unnecessary open surgery, but in cases where gross total resection is indicated, it subjects the patient to two operations. Also, needle biopsy of pineal region tumors has a greater risk of hemorrhage than biopsy of other regions of the brain due to the adjacent vascular structures, the need to cross over more than one pial plane, lack of surrounding tissues for providing tamponade, and the high hemorrhage rate of many tumor pathologies found in the pineal region.
Some surgeons prefer planned gross total resection for any symptomatic tumor, and if the pathology found on intraoperative frozen sections does not warrant resection, a less aggressive resective approach is chosen. However, this strategy is not part of my philosophy.
Endoscopic biopsy may be paired with endoscopic third ventriculostomy in order to treat hydrocephalus and obtain tissue for diagnosis in one operation. This approach also has the advantage of maintaining potential operative corridors to be used for gross total resection, if it is indicated by tumor pathology. The disadvantages of this policy are the significant risk of intraventricular hemorrhage from the tumor in these circumstances and the difficulty of performing a third ventriculostomy and a biopsy through the same burr hole without placing the forniceal bodies at some risk.
The following figure illustrates my algorithm for determining how to deal with pineal region tumors found on imaging.
Figure 4: The recommended decision tree to deal with uncertainties associated with the diagnosis of a pineal region tumor is indicated.
If the patient is suffering from symptomatic acute hydrocephalus, an external ventricular drain can provide an opportunity to test CSF for markers. An exception to the algorithm in the above figure is the lack of positive markers in a prepubertal boy presenting with or without diabetes insipidus who can be directly treated with adjuvant therapies.
My preferred approach is to perform an endoscopic third ventriculostomy with biopsy for the lesion causing hydrocephalus. Germinomas are radiated, whereas malignant nongerminomatous germ cell tumors receive chemotherapy and radiation followed by a “second-look” surgery.
If the CSF tumor markers are inconsistent with a germ cell tumor, I perform an open biopsy, and if indicated by intraoperative frozen section pathology, I attempt gross total resection. Adjuvant treatments are administered as indicated by final pathologic diagnosis. Gross total resection is not achieved at the expense of neurologic function. Densely adherent tumors (especially to the deep veins) necessitate subtotal resection.
The decision algorithm shown here is based on findings in the current literature, which are somewhat limited and at times inconclusive. I do not adhere rigidly to this management algorithm for every patient.
SURGICAL APPROACHES
The pineal region can be reached through several different surgical corridors depending on the specific location and characteristics of the tumor and the surgeon’s experience/comfort level.
Figure 5: Different surgical approaches to the pineal region are shown. The supracerebellar infratentorial (midline and paramedian variant) routes are most commonly utilized. Other supratentorial approaches to the region are also described. These approaches include the posterior interhemispheric sub- or transsplenial (transcallosal), occipital transtentorial and least likely the transcortical transventricular.
Midline Supracerebellar Infratentorial Approach
This is the most favored route to the pineal region and is also most familiar to neurosurgeons.
Figure 6: The midline supracerebellar infratentorial approach allows the surgeon to utilize the natural corridor between the cerebellum and tentorium cerebelli to reach the pineal region. This approach offers advantages because it is simple and familiar to most neurosurgeons.
Since most pineal tumors are midline infratentorial lesions, the midline supracerebellar infratentorial approach offers the most direct route to the surgical target. Most pineal tumors are situated ventral to the deep diencephalic venous structures, so this corridor allows reasonable exposure of the tumor while leaving the veins relatively untouched.
During surgery, the patient may be placed in the sitting position so that gravity retraction on the cerebellum widens the supracerebellar operative corridor. There is minimal accumulation of blood and fluids within the operative field. Considering the risks of air embolism and the uncomfortable operating posture that the surgeon must assume when the patient is in this position, I believe the only reasonable indication for the sitting position these days is pineal region tumor surgery.
There are also disadvantages associated with this approach. The corridor is narrow and does not readily allow for dissection of the inferior aspect of the tumor that is covered by the apex of the culmen. Numerous midline bridging veins are often sacrificed, leading to cerebellar congestion, further limiting the exposure. For more details about this approach, please refer to the chapter on Midline Supracerebellar Craniotomy.
Paramedian Supracerebellar Infratentorial Approach (My Preferred Approach)
For the past few years, I have used the paramedian supracerebellar approach with very satisfying results for small to giant midline pineal region masses. Both sides of the midline are accessible via this trajectory.
Figure 7: The paramedian supracerebellar infratentorial approach combines the benefits of both midline supracerebellar infratentorial and occipital transtentorial approaches without placing some of the normal structures at risk. However, this route is technically challenging to work through because the operative corridor is narrow and long.
This approach is performed with the patient in the lateral position, alleviating the disadvantages of the sitting position. Only one transverse sinus and cerebellar hemisphere is placed at risk and the torcula is not manipulated. It utilizes the corridor between the lateral cerebellar hemisphere and the tentorium where fewer bridging veins reside and the numerous midline veins are avoided.
Because the paramedian tentorial surface of the cerebellum is sloped inferiorly compared with the midline culmen, the caudal reach of the operative corridor is widened and the working angles attain higher degrees of freedom.
Finally, the tentorium can be divided to increase the exposure, if needed. For further details regarding the corresponding technical nuances, as well as the advantages and disadvantages of this approach, please refer to the chapter on Paramedian Supracerebellar Craniotomy.
Occipital Transtentorial Approach
The occipital transtentorial approach enters the cranial vault through a unilateral occipital craniotomy. This approach offers a wide exposure of the quadrigeminal plate and is particularly useful for large tumors extending laterally and inferiorly.
A three-quarter prone or lateral position is beneficial to exploit gravity retraction on the nondominant occipital lobe. A paramedian linear or U-shaped right occipital scalp flap is completed. The medial vertical limb of the U-shaped flap starts to the left of the midline at about the level of the torcula. Two burr holes over the superior sagittal sinus and torcula facilitate elevation of a bone flap that unroofs these dural venous sinuses. Lumbar CSF drainage assists with brain relaxation.
Interhemispheric dissection exposes the straight sinus so that the tentorium can be divided adjacent to it. The inferior sagittal sinus and falx can be divided to facilitate further transfalcine exposure. The arachnoid overlying the tumor and the quadrigeminal cisterns can be seen from a supraposterior perspective. Please see the Pineal Region Tumor (Occipital Transtentorial Approach) chapter for further details.
The drawbacks of this approach include difficulty with anatomic orientation and dividing the tentorium appropriately, working around the veins of the deep venous system, and the possibility of a homonymous hemianopsia from occipital lobe retraction. Overall, this is a cumbersome approach that places numerous normal structures at risk. However, it is a reasonable option when the tumor has displaced the deep veins caudally or posteriorly, precluding a safe reach via the supracerebellar infratentorial approach.
Click here to view the interactive module and related content for this image.
Figure 8: The steps for the occipital transtentorial approach are shown. Note the panoramic view of the pineal region and the superior-to-inferior operative trajectory (images courtesy of AL Rhoton, Jr).
Posterior Interhemispheric Transcallosal Approach
The posterior interhemispheric transcallosal route is best suited for tumors originating dorsal or rostral to the deep venous structures, displacing the veins ventrally. This configuration can occur with tectal and posterior thalamic tumors that mimic pineal region masses.
This approach utilizes an interhemispheric corridor along the parieto-occipital junction. The splenium is divided and the tumor is revealed underneath. The surgeon works between (intervenous) or along (paravenous) internal cerebral veins. This approach provides the most direct route to the tumors dorsal to the deep venous system, but it may cause a partial disconnection syndrome if the splenium is not affected by the tumor; it also places the internal cerebral veins at risk.
For more details, please refer to the chapter on Posterior Interhemispheric Transcallosal Intervenous/Paravenous Variant.
Figure 9: This pineal region epidermoid (note the hyperintense signal on the diffusion weighted sequence in the left upper image) extended into the third ventricle and affected the splenium. This tumor was explored and resected via the posterior interhemispheric transcallosal intervenous route. The deep veins were displaced dorsally in this patient (right lower image).
Other Considerations
Combined approaches may be necessary to fully disclose superior fourth ventricular tumors that reach the supratentorial space and giant tumors that affect the pineal region but extend caudally to the level of the superior fourth ventricle.
Figure 10: A combined infratentorial-supracerebellar and telovelar approach may be necessary for tumors along the superior fourth ventricle and extending into the pineal region. The supracerebellar route alone is likely to be inadequate to create enough tumor exposure without undesirable retraction on the cerebellum.
Pearls and Pitfalls
- Careful preoperative evaluation of pineal region masses can spare the patient from an unnecessary operative procedure.
- The paramedian supracerebellar craniotomy provides flexible working angles for resection of most pineal region masses.
- The selection of the appropriate operative corridor should allow the surgeon to protect the vital neurovascular structures while facilitating gross total resection of the tumor.
References
Ellis J, Moise G, Bruce J. Meningiomas of the third ventricle and pineal region, in: Demonte F, McDermott M, Al-Mefty O, (eds): Al-Mefty’s Meningiomas, 2nd ed. New York: Thieme Medical Publisher, 2011:323-330
Kennedy B, Bruce J. Surgical approaches to the pineal region. Neurosurg Clin N Am 2011; 22:367-380
Please login to post a comment.