Subependymoma
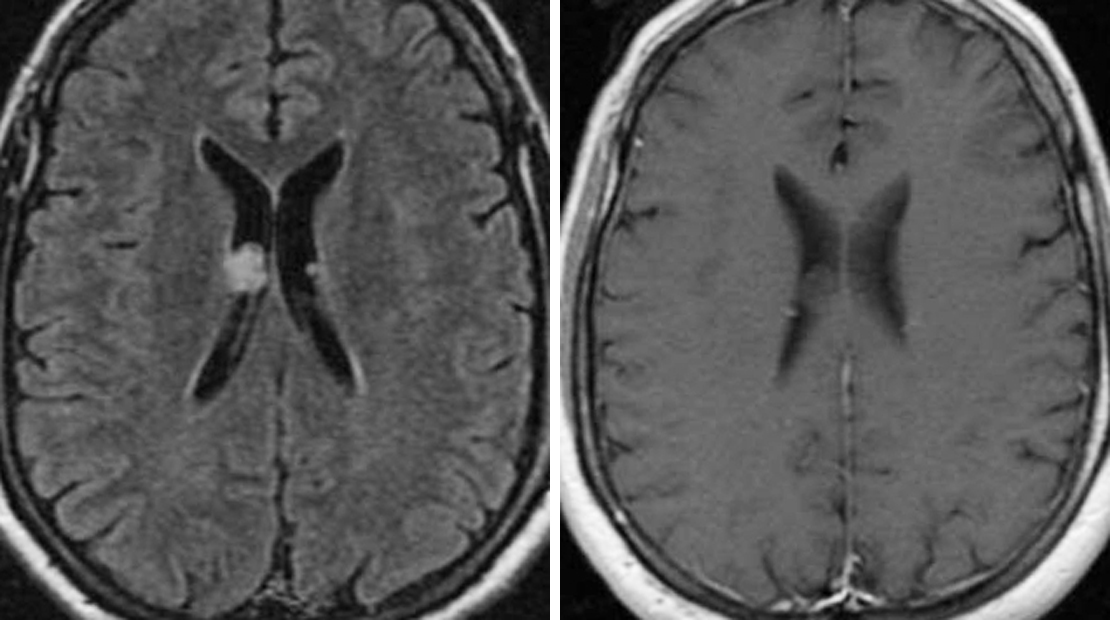
Figure 1: (Left) This small FLAIR-hyperintense intraventricular nodule represents a subependymoma, a fairly common and benign tumor. (Right) Enhancement is variable, but this example shows no significant enhancement on postcontrast T1WI.
Figure 2: Often nearly invisible on CT imaging (top left), subependymomas are intraventricular tumors that are usually much more evident in FLAIR imaging (top right). (Bottom) This left frontal horn subependymoma demonstrates no appreciable enhancement on postcontrast T1WI.
Figure 3: Axial noncontrast head CT imaging demonstrates a calcified lesion in the fourth ventricle. Sagittal FLAIR (top right), axial T1-weighted (without contrast) (second row, left), axial T1-weighted (postcontrast) (second row, right), DWI (third row, left), ADC (third row, right), and axial T2FS (bottom) images demonstrate a nonenhancing mass arising from the floor of the fourth ventricle without restricted diffusion. The appearance and location of this lesion are classic for subependymoma.
BASIC DESCRIPTION
- Benign, intraventricular tumor, likely arising from subependymal glial precursor cells
PATHOLOGY
- WHO grade I
- Solid, avascular, lobulated mass
- Large tumors can show calcification, hemorrhage, and cystic components
- Sporadic
- Usually arising from floor of the fourth ventricle or septum pellucidum or lateral wall of the lateral ventricle
CLINICAL FEATURES
- Afflicts middle-aged or older adults (in their fifth or sixth decade of life)
- Male gender predilection
- Common presenting symptoms:
- Usually asymptomatic
- With larger tumors, symptoms are often related to increased intracranial pressure (ie, nausea, vomiting, headaches, ataxia)
- Treatment
- Conservative management with serial imaging if asymptomatic
- If symptomatic, gross-total resection for lateral ventricular tumors and subtotal resection for fourth ventricle tumors; might require CSF shunt for hydrocephalus
- Recurrence is rare after resection
- Very good prognosis for patients with supratentorial subependymoma
IMAGING FEATURES
- General
- Well-defined, lobulated, nonenhancing ventricular mass
- Fourth ventricular tumors might grow through the foramen of Magendie
- CT
- Isodense to hypodense
- ±Calcification and cysts in larger tumors
- Usually little to no enhancement on contrast-enhanced CT imaging
- MRI
- T1WI: homogenous, hypointense to isointense relative to white matter
- T2WI: hyperintense; heterogeneous signal due to cystic components and hemorrhage in larger tumors
- FLAIR: hyperintense, no edema of adjacent brain parenchyma
- T2*/GRE/SWI: signal blooming secondary to calcification
- T1WI+C: little to no enhancement most common
IMAGING RECOMMENDATIONS
- MRI with contrast; CT imaging can be helpful for the identification of small calcifications
For more information, please see the corresponding chapter in Radiopaedia.
Contributors: Rachel Seltman, MD, and Jacob A. Eitel, MD
References
Bi Z, Ren X, Zhang J, et al. Clinical, radiological, and pathological features in 43 cases of intracranial subependymoma. J Neurosurg 2015;122:49–60. doi.org/10.3171/2014.9.JNS14155.
Chiechi MV, Smirniotopoulos JG, Jones RV. Intracranial subependymomas: CT and MR imaging features in 24 cases. AJR Am J Roentgenol 1995;165:1245–1250. doi.org/10.2214/ajr.165.5.7572512.
Hou Z, Wu Z, Zhang J, et al. Clinical features and management of intracranial subependymomas in children. J Clin Neurosci 2013;20:84–88. doi.org/10.1016/j.jocn.2012.05.026.
Louis DN, Ohgaki H, Wiestler OD, et al (eds). WHO Classification of Tumours of the Central Nervous System: Subependymoma. IARC Press, Lyon, France; 2007:70–71.
Osborn AG, Salzman KL, Jhaveri MD. Diagnostic Imaging (3rd ed). Elsevier, Philadelphia, PA; 2016.
Smith AB, Smirniotopoulos JG, Horkanyne-Szakaly I. From the radiologic pathology archives: intraventricular neoplasms: radiologic-pathologic correlation. Radiographics 2013;33:21–43. doi.org/10.1148/rg.331125192.
Silverstein JE, et al. MRI of intracranial subependymomas. J Comput Assist Tomogr 1995;19:264–267. doi.org/10.1097/00004728-199503000-00018.
Please login to post a comment.