Open Skull Fracture
The appropriate management strategy (operative versus nonoperative) for a depressed skull fracture continues to remain controversial.
Closed linear fractures, even if depressed, may be left untreated if there is no significant underlying expanding hematoma or mass lesion. A cosmetic deformity may justify operative intervention.
However, compound fractures (open to the outside with an associated skin laceration) coupled with suspected dural tears are indications for neurosurgical intervention because of their high likelihood of subsequent infection and abscess formation. Unfortunately, it is no reliable method to discern if the dura has been violated based on clinical findings or neurologic imaging, thus necessitating neurosurgical exploration.
It is reasonable to expect some form of underlying traumatic brain injury (TBI) with a skull fracture. TBI is commonly classified based on the level of severity of the initial injury and the associated sequelae. The classification of the TBI prognosticates the patient’s outcome in terms of risk of posttraumatic epilepsy, return of global function, and mortality.
The presence of focal neurologic signs is not an indication for surgical intervention for a skull fracture. Focal lesions typically arise from the force of the initial insult and result in a parenchymal hematoma or contusion. Elevation of the depressed fracture in these cases will not be therapeutic because the neurologic deficits are caused by an intraparenchymal, noncompressive injury.
Presentation
The presentation of patients with depressed skull fractures is highly variable, ranging from those who present without any acute neurologic abnormalities to those presenting in a comatose state (GCS ≤ 8). Presentation is further complicated by the location of the injury because the scalp may shift so that the skin laceration does not reside directly over the skull fracture.
Even when the visible skull fracture appears to slightly depressed, the physician should maintain a high index of suspicion for a more serious depressed fracture because the inner table of the skull may separate from the outer table, leading to a dural tear that may be overlooked. Indeed, inappropriate management of depressed skull fractures because of missed diagnoses is the primary risk factor for avoidable complications from these injuries.
The mechanism of insult resulting in a skull fracture has an integral role. As such, it is critical to obtain a thorough history from the patient and eyewitnesses to the event. Assault victims are likely to suffer less severe injuries than those who present after a motor vehicle accident.
Evaluation
Depressed skull fractures require a high index of suspicion and low threshold for acquiring neurologic imaging. The preferred imaging method is a noncontrast computed tomography (CT) scan. This modality with its dedicated bone windows allows high-resolution viewing of the skull, facilitating the diagnosis of small depressed fractures that may be overlooked on frontal or lateral x-rays.
Figure 1: A classic CT scan of a right frontal depressed skull fracture with underlying punctate contusions (upper images) is demonstrated. The fractured fragments are depressed more than the thickness of the skull, so an underlying dural injury is highly likely. The lower images show a right frontal depressed skull fracture extending through the anterior and posterior tables of the frontal sinus (arrows).
Unfortunately, it is often difficult or impossible to ascertain on imaging alone whether or not the dura was violated from a compound depressed skull fracture.
Additional imaging, such as CT or catheter angiography, is indicated if the fracture appears to interact with a dural sinus. Angiography will reveal if the lumen of the dural sinus has been compromised or remains intact. Elevation of skull fractures over the dural venous sinuses is risky and should be avoided if at all possible because an occult sinus injury is not likely to be apparent before the fracture is manipulated during surgery. Repair of the sinus can place its patency at risk.
If a craniotomy is necessary for evacuation of a symptomatic compressive hematoma caused by a fracture over the venous sinus, I leave a strip of bone over the dural sinus during the craniotomy to avoid its further injury via manipulating the overlying bone fragments.
Indications for Surgery
The presence of compressive and symptomatic intracranial extra-axial and parenchymal hematomas is an absolute indication for surgery. Other indications for surgical management of a depressed skull fracture include the following:
- Compound skull fractures depressed greater than the thickness of the cranium may undergo operative intervention because of the high likelihood of associated dural injury.
- Compound depressed fractures may be treated operatively if there is clinical or radiographic evidence of involvement of the posterior wall of the frontal sinus, gross cosmetic deformity, pneumocephalus, or gross wound contamination.
Timing of surgical management
- Prompt operation (usually within 12 hours of injury) is recommended to decrease the risk of infection.
Indications for nonoperative management
- Nonoperative management of a closed depressed cranial fracture is reasonable unless the resultant cosmetic deformity is significant.
- Patients with compound depressed cranial fractures may be treated nonoperatively if there is relatively reliable clinical or radiographic evidence of dural preservation and lack of gross contamination or pneumocephalus.
Despite the above recommendations, significant inconsistencies in the reported patient series prevent reliable conclusions. Conservative management of a compound contaminated skull fractures with potential dural violation may be considered after the lacerations are well debrided and loose bone fragments removed in the emergency room. Next, the wound is meticulously closed. Aggressive treatment with antibiotics is advised.
The rationale for conservative management of depressed cranial fractures arose based on the experience during the era before CT scans were widely available and used for imaging head injuries. During this period, many patients with depressed skull fractures recovered without obvious manifestations of infection or long-term complications via nonoperative methodologies.
I advocate the conservative route when possible.
Preoperative Considerations
Once the decision is made to proceed with surgery, the patient should be hemodynamically stabilized and prepared for general anesthesia. Although prompt surgery is important, an isolated depressed skull fracture does not necessarily constitute an emergency provided there is no expanding intracranial mass lesion putting the patient at risk for herniation.
Most surgeons advocate operating within 12 hours of injury, but delays up to 48 hours do not appear to expose the patient to an increased risk of infection.
Stellate and complex avulsion injuries of the scalp require the assistance of our plastic surgery colleagues during surgery. This arrangement should be made ahead of time so appropriate preparations are made.
REPAIR OF A SKULL FRACTURE
The patient should be placed on the operating table in either the supine or lateral position, depending on the location of the skull fracture. The head is often rested on a donut gel rest. The choice of initial incision depends on the pattern of scalp laceration and fracture location in relation to the scalp vascular pedicles. Cosmesis is another consideration.
If the fracture is located behind the hairline, the “lazy-S” incision incorporating the simple laceration is preferred because it allows adequate exposure and can be easily extended if necessary. If the fracture is located over the forehead, a bicoronal incision behind the hairline is more cosmetically acceptable.
Figure 2: A skull fracture in the lateral frontal bone and behind the hairline is demonstrated. This fracture is both comminuted and depressed. The dashed line represents the lazy-S incision, which incorporates the scalp laceration and facilitates adequate exposure of the underlying fracture.
Upon adequate exposure of the fracture, the scalp edges are debrided and loose bone fragments removed. The operator should carefully proceed with elevation and removal of bone fragments to avoid further damage to the underlying dural venous sinuses and brain parenchyma.
If there is a risk of further injury to the underlying structures with blind elevation of the impacted fragments, I place a burr hole at the periphery of the fractured area, identify the normal dura and elevate the bone fragments in a piecemeal fashion and under direct vision, starting from the area of the burr hole. All depressed and comminuted fragments should be removed and retained so they may be replaced at the end of the operation.
If a bone fragment is embedded in the dural sinus and the sinus was noted to be patent on preoperative imaging, this fragment should not be displaced. Every attempt should be made to avoid maneuvers that lead to sinus wall disruption. For more details regarding management of bleeding from a dural venous sinus, please refer to the chapter on Repair of Dural Venous Sinus Injury.
After removal of the fractured bone fragments, the dura is carefully inspected and any intracranial hematoma should be removed with manual irrigation and suction. If no dural laceration is present and the initial CT scan did not demonstrate any obvious subdural pathology, the dura should not be opened for further inspection. Instead, the surgeon should proceed with closure.
Figure 3: Following removal of the depressed and comminuted fracture fragments, the dura and any intracranial hematoma within the epidural and subdural spaces are exposed. The hematoma is mobilized and evacuated using manual suction and irrigation. If possible, the entire hematoma should be removed and hemostasis secured through further dura incisions. If the symptomatic epidural hematoma extends beyond the edges of the fractured skull, the bony exposure is widened. The operative field should be completely debrided and irrigated profusely with antibiotic solution to prevent leaving an infection source behind.
The underlying brain should be examined for contused and necrotic areas. These areas should be gently aspirated until relatively normal brain is visible. I do not pursue small bone fragments embedded deep in the brain at the cost of further cortical disruption. Aggressive resection of the necrotic brain is not warranted as this maneuver leads to additional injury and bleeding, especially around the functional cortices.
Once the subdural pathology has been addressed, all dural openings are closed in a “watertight” fashion. If the dural edges cannot be approximated, I harvest a piece of pericranium away from the area of the lacerated scalp and use it as an autograft for dural repair. Allograft dura is avoided because of the increased risk of infection associated with its use.
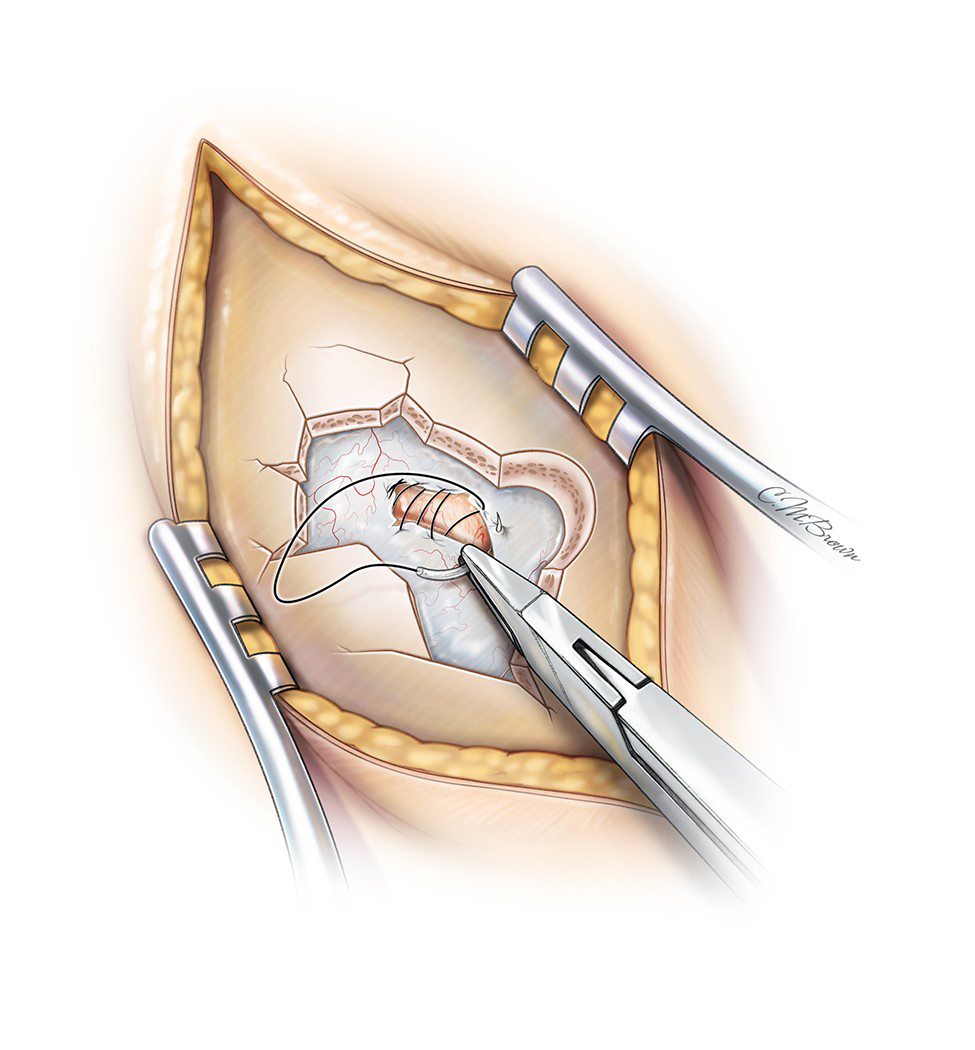
Figure 4: Following removal of the underlying hematoma and adequate debridement and irrigation of the operative field, I suture all dural lacerations in a watertight fashion to minimize the risk of CSF leakage and subsequent infection.
All previously removed bone fragments should be immersed in and cleaned with antibiotic solution. Next, they are reconnected in their original places using cranial miniplates.
An attempt should be made to use the comminuted bone fragments rather than prosthetic cranioplasty in order to minimize the risk of postoperative infection. If it is impossible to reapproximate the fractured skull fragments or if they are grossly contaminated, I prefer to use wire mesh, instead of methyl methacrylate, to reconstruct the skull defect to reduce the risk of infection.
In the event of an established infection in a patient who presented in a delayed fashion after a compound skull fracture, I do not replace the infected fractured bone fragments. Instead, I prefer irrigation and debridement without reconstruction of the skull defect. A delayed cranioplasty is performed no sooner than 4-6 months after the injury. A custom made alloplastic prosthetic implant is used.
Figure 5: Following irrigation and debridement of the brain, dura, and skull fragments, I replace the bone fragments using miniplates.
Finally, the galea and the skin should be approximated.
Figure 6: The skin edges are carefully approximated for a better chance at healing. I often use a temporary subgaleal drain.
Compound Depressed Fractures and the Dural Venous Sinuses
Compound depressed fractures over the dural venous sinuses deserve special considerations in their management. As previously mentioned, a cerebral angiography should be obtained to investigate any interactions between the skull fracture and the underlying sinus.
If a dural venous sinus has been impacted but remains patent with a small but hemodynamically nonsignificant lumenal deformity, a conservative nonoperative strategy is preferred despite the presence of a compound fracture. All attempts should be made to avoid surgical intervention in an otherwise asymptomatic patient. Frequent imaging is warranted to detect any expansion of sizable hematomas.
Broad-spectrum intravenous antibiotics are administered during the hospitalization. After discharge, frequent follow-up visits are necessary to detect early signs of infection, including a brain abscess. A CT scan with contrast is requested approximately two weeks after the event to rule out early stages of an abscess.
A symptomatic occluded sinus requires neurosurgical intervention. Intracranial hypertension due to venous sinus incompetence requires exploration and reestablishment of blood flow. Please refer to the chapter on Repair of Dural Venous Sinus Injury for further details. If the sinus is occluded and the patient remains asymptomatic from such a phenomenon, the sinus may be ligated if evacuation of the associated symptomatic hematoma is warranted.
Once the decision is made to proceed to surgery, special precautions are necessary. All measures for detection and treatment of air embolism should be instituted. These measures include transesophageal echocardiography, precordial Doppler ultrasonography, esophageal stethoscope and capnography (end-tidal carbon dioxide), monitoring end-expired nitrogen, and right heart catheter (this can be used to aspirate air bubbles). The patient’s head should be slightly elevated to minimize bleeding because massive hemorrhage may occur from the sinus, resulting in exsanguination.
Conversely, the patient’s head should not be significantly elevated to minimize the risk of an air embolus. The incision and bone elevation should occur first at points distal and proximal to the dural sinus injury; this technique allows proximal and distal control over the sinus to avoid massive blood loss.
Next, a burr hole is placed next to the fracture lines and the bone fragments are removed gradually from the dura, first from proximal and distal regions relative to the point of sinus injury. Finally, the bone fragments overlying the injured or occluded portions of the sinus are removed. If the venous sinus is patent, I leave a strip of bone over the sinus untouched to minimize the risk of tear in the roof of the sinus from manipulating the overlying bone fragments.
Occluding the sinus at both ends via aneurysm clips or hemostats should control bleeding. If the sinus laceration is small, the edges of its wall are approximated and sutured together using 5-0 nonabsorbable sutures. If the edges of the sinus cannot be approximated, a small section of the pericranium is excised and used as a graft to patch the defect in the sinus wall. Alternatively, a piece of adjacent dura is rotated and sutured in place along the edges of the sinus to reconstruct the roof of the vessel. Gelfoam packing is avoided as this will lead to permanent sinus occlusion. Instead, two small cotton balls may be temporarily inserted in the proximal and distal ends of the exposed lumen to provide temporary occlusion.
The use of postoperative aspirin for maintaining sinus patency is controversial, but recommended.
Figure 7: A tear in the roof of the right transverse-sigmoid junction was repaired using a piece of adjacent dura that was rotated and sewn in place. The vein of Labbe (arrow) was spared.
Depressed Fractures of the Frontal Sinus
It is not unusual for the occupant’s frontal sinus to be fractured during high-impact motor vehicle accidents. The fracture site is considered an important factor when deciding between conservative and surgical management.
If only the anterior wall of the frontal sinus is fractured and it is not displaced, conservative management is reasonable. If the posterior wall of the sinus is fractured, then neurosurgical intervention is strongly considered because the likelihood of a dural injury and CSF fistula is real. I personally have attempted to manage minimally displaced posterior frontal sinus wall fractures expectantly as long as CSF leakage is definitively ruled out.
The clinical signs of a frontal sinus fracture include anesthesia in the distribution of the supraorbital nerves, CSF rhinorrhea, subconjunctival ecchymosis, and depression of the frontal sinus. The CT findings for an occult posterior wall fracture include pneumocranium and intracranial hematoma just posterior to the frontal sinus.
If neurosurgical intervention is required for a frontal sinus fracture, a bicoronal incision behind the patient’s hairline should be used. A large piece of vascularized pericranium is harvested during the exposure and left attached along the orbital rims.
To access the posterior wall of this air sinus, I elevate a portion of its anterior wall. This goal is accomplished using a B1 bit without a footplate to elevate a plate of bone just around the frontal sinus with minimal exposure of the dura. Usually, the anterior wall is also fractured and can be readily elevated.
Next, the mucosa and epithelium of the sinus are methodically removed and curetted away in order to prevent delayed formation of a mucocele. The posterior wall should then be explored. If a depressed fracture or CSF leakage is apparent, the posterior wall should be elevated and the underlying dura inspected and repaired.
Any lacerations in the dura are closed in a watertight fashion using pieces of pericranial free flaps. The posterior sinus wall bone fragments are not replaced. Instead, large fat globules, pieces of temporalis muscle, or bacitracin powder mixed with bone wax are used to exenterate the frontal sinus. The previously prepared large piece of vascularized pericranium is used to thoroughly cover the exposed sinus and is sewn in place to the dura. Finally, the bone fragments of the anterior sinus wall are approximated and secured in place using miniplates.
Please refer to the Bifrontal Craniotomy chapter for further details regarding management of frontal sinus injury.
Posttraumatic Epilepsy
The risk of posttraumatic epilepsy is directly related to the severity of the injury. Early posttraumatic epilepsy occurs within the first 24 hour to 7 days of injury. Late posttraumatic epilepsy occurs after 7 days of injury.
Significant risk factors for the development of late epilepsy include brain contusion with a subdural hematoma, skull fracture, loss of consciousness for more than 24 hours, and age 65 or older. Importantly, early epilepsy is not prognostic for late epilepsy if other potential prognostic factors are appropriately managed.
The prophylactic use of antiepileptic drugs (AEDs) has been shown to be beneficial in the treatment of early posttraumatic epilepsy, but this practice appears to have little to no effect on the development of late posttraumatic epilepsy.
Thus, AED prophylaxis is indicated for the prevention of early posttraumatic epilepsy (within 7 days of the traumatic event), but there is no convincing data indicating that it should be used for preventing the development of late epilepsy. Repair of skull fractures does not affect the incidence of posttraumatic seizures. Therefore, this procedure should not be offered as a treatment option for decreasing the risk of posttraumatic seizures.
Antibiotics for the Treatment of Skull Fractures
Infection including brain abscess is considered a major complication of compound depressed skull fractures, and is a primary reason for neurosurgical intervention.
Although it is clear that patients who present with an established infection must receive antibiotic therapy, it is controversial whether the prophylactic use of antibiotics provides any benefit.
Many studies and metaanalyses have suggested that there is currently no substantial evidence to convincingly support the use of prophylactic antibiotics in reducing the occurrence of meningitis and other infectious complications for calvarial and skull base fractures. Thus, although the use of prophylactic antibiotics for a noninfected depressed skull fracture is comforting, it is not required based on current data.
Protocol for Management of Skull Fractures
Simple, Non-Open Skull Fracture:
- No Specific treatment or antibiotics needed
Basilar skull fracture with CSF leak, or presumed CSF leak (pneumocephalus):
- Give Prevnar13® now followed by Pneumovax23® 8 weeks later
- If patient has had one or both of these vaccines in the past, discuss with pharmacy to determine appropriate vaccination/schedule
- If patient is under the age of 18, discuss with pharmacy to determine appropriate vaccination/schedule
- Evidence does not support prophylactic antibiotic use in patients with basilar skull fractures, regardless of presence or absence of CSF leak
Open Depressed skull fracture, non-operative management:
- Conservative management if NO evidence of ICH, CSF leak, or contamination
- Irrigate/debride and close wound.
- Evidence does not support prophylactic antibiotic use.
Open Depressed skull fracture with operative management:
- Peri-op antibiotics: selection based on the significance of injury, exposure of wound to environment and patient factors (see chart below)
- Prolonged antibiotics - evidence does not support use
- Seizure prophylaxis x 7 days (only if needed based on additional TBI; not recommended for simple isolated skull fracture)
- If dural injury found at surgery, Prevnar13® now followed by Pneumovax23® 8 weeks later
- If patient has had one or both of these vaccines in the past, discuss with pharmacy to determine appropriate vaccination/schedule
- If patient is under the age of 18, discuss with pharmacy to determine appropriate vaccination/schedule
Criteria for operative management (one or more of the following):
- Full thickness or depression >1 cm
- Gross cosmetic deformity
- Evidence of dural tear
- Gross contamination
- Associated operable lesion (hematoma, foreign body, etc.)
| Significance of Injury, Contamination | Exposure of Open Fracture | Antibiotic Selection | Duration | |
| Requires OR but Minor, Minimal Exposure | Limited | First Line Cefazolin |
Cephalosporin Allergy Vancomycin |
Peri-operative* |
| Severe / Significant, Grossly Contaminated | Environmental contamination Soil / Dirt, Water, or Unknown |
First Line Piperacillin / Tazobactam AND Tobramycin x 1 dose only |
Penicillin Allergy Vancomycin, Aztreonam, Metronidazole, and 1x dose Tobramycin |
Peri-operative* |
| Severe / Significant, Grossly Contaminated | Environmental contamination Soil / Dirt, Water, or Unknown |
Cefepime † 2 gm IVPB Q8h over 4 hrs AND Metronidazole 1 gm IVPB Q8h | Cephalosporin Allergy Meropenem 1 gm IVPB Q8h over 4 hrs (no metronidazole needed) |
5 days, ID consult |
| Any | Risk for MRSA | Add Vancomycin (if not otherwise ordered) | Same as otherwise indicated | |
* Peri-operative for MAXIMUM of 24 hours. Pre-operative dose only for patients without contamination. For patients unable to go to OR & get washout of contaminated depressed skull fracture, may consider antibiotics for max 72 hrs. † Dose adjustment needed for renal dysfunction.
Contributor: Jonathan Weyhenmeyer, MD
For additional illustrations of cranial base fractures, please refer to the Jackler Atlas by clicking on the image below:
References
Al-Haddad SA, Kirollos R. A 5-year study of the outcome of surgically treated depressed skull fractures. Ann R Coll Surg Engl. 2002;84:196-200.
Annegers JF, Hauser WA, Coan SP, Rocca WA. A population-based study of seizures after traumatic brain injuries. N Engl J Med. 1998;338:20-24.
Beghi E. Overview of studies to prevent posttraumatic epilepsy. Epilepsia. 2003;44(Suppl 10):21-26.
Braakman R. Depressed skull fracture: data, treatment, and follow-up in 225 consecutive cases. J Neurol Neurosurg Psychiatry. 1972; 35:395-402
Bullock MR, Chesnut R, Ghajar J, Gordon D, Hartl R, Newell DW, Servadei F, Walters BC, Wilberger JE. Surgical management of depressed cranial fractures. Neurosurgery. 2006;58:52–56.
Cooper PR. Depressed skull fracture, in: Apuzzo MLJ (ed). Brain Surgery Complication Avoidance and Management. Churchill Livingstone, 1993, 1273-1282.
Hsiao KY, Hsiao CT, Weng HH, Chen KH, Lin LJ, Huang YM. Factors predicting mortality in victims of blunt trauma brain injury in emergency department settings. Emerg Med J. 2008;25:670-673.
Jennet B, Miller JD. Infection after depressed fracture of skull. Implications for management of nonmissile injuries. J Neurosurg. 1972;36:333-339
Kalaveros N. Current trends in the management of frontal sinus fractures. Injury. 2004;35:340-346.
Ratilal BO, Costa J, Sampaio C, Pappamikail L. Antibiotic prophylaxis for preventing meningitis in patients with basilar skull fractures (review). Cochrane Database Syst Rev. 2011;8:1-33.
van den Heever CM, van der Merwe DJ. Management of depressed skull fractures. Selective conservative management of nonmissile injuries. J Neurosurg. 1989; 71:186-190.
Please login to post a comment.