Cerebral Hemorrhage
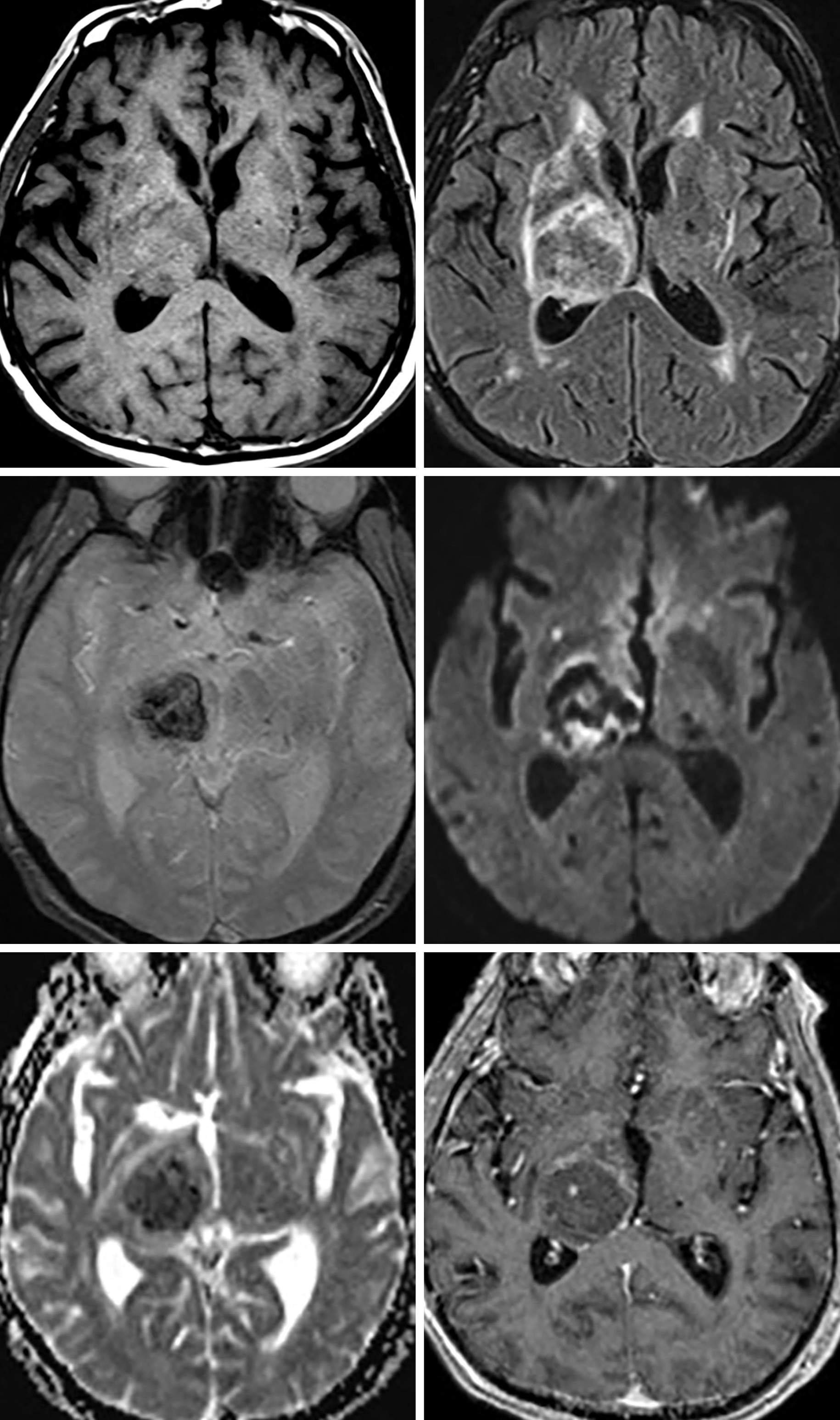
Figure 1: Moderately sized lesion in the right thalamus with T1-isointense signal (top left) and heterogeneous isointense and hyperintense signal on FLAIR imaging (top right) with associated susceptibility artifact centrally on SWI (middle left). (Middle Right and Bottom Left) Note the mild amount of reduced diffusivity, which in this case is likely due to the susceptibility artifact from the hemorrhage on DWI/ADC. (Bottom Right) Enhancement could be present in the periphery, as in this case, particularly in the subacute stage. Note that the age of the blood products is not clear by signal intensities. The signal characteristics are often heterogeneous, as seen in this case, which makes accurate staging difficult and potentially inaccurate.
Description
- Many causes including hypertension, infarction, underlying malignancy, arteriovenous malformation, cerebral amyloid angiopathy, drug abuse, etc
- Highly vascularized malignant primary brain tumors tend to bleed spontaneously and should always be included in the differential diagnosis of nontraumatic intracerebral hemorrhage
- Up to 10% of patients with a brain tumor can experience a diagnostic delay if CT is the only imaging modality
Pathology
- Variable depending on the underlying etiology
Clinical Features
- Symptoms
- Headache, sensorimotor deficits, altered mental status, herniation syndromes
- Age and gender
- Variable depending on the underlying etiology
- Prognosis
- Related to location and size
- Approximately 25% of patients die within the first 48 hours
Imaging
- General
- Round, oval, or irregular
- Location varies with etiology
- Hypertension: striatocapsular > thalamus > pons and cerebellum
- Thrombosis: follows arterial or venous territories
- Amyloid: peripheral/lobar
- Malformations and malignancies: any location
- Modality specific
- CT
- Hyperdense hematoma with surrounding hypodense edema in the acute setting
- Hematoma becomes less dense with time
- CTA/CTV
- Only helpful when thrombosis is suspected
- MRI
- Signal characteristics correspond to the age of the blood products
- Hyperacute (<24 hours)
- T1 isointense, T2 hyperintense
- Intracellular oxyhemoglobin
- Acute (24 hours to 3 days)
- T1 isointense, T2 hypointense
- Intracellular deoxyhemoglobin
- Early subacute (3–7 days)
- T1 hyperintense, T2 hypointense
- Intracellular methemoglobin
- Late subacute (7 days to 3 weeks)
- T1 hyperintense, T2 hyperintense
- Extracellular methemoglobin
- Chronic (>3 weeks)
- T1 and T2 hypointense
- Extracellular hemosiderin
- T2*
- Often hypointense signal, particularly with hemosiderin deposition
- Contrast
- Can demonstrate enhancement if underlying malignancy or vascular malformation
- Small amount of reactive enhancement can also be present around a subacute hematoma
- MRA/MRV
- Helpful when looking for thrombosis
- Conventional angiography
- Helpful when looking for thrombosis or underlying vascular malformation
- Dual-energy CT
- Can prove useful for rapidly identifying the underlying etiology
- Many recent studies have demonstrated the utility of dual-energy CT for detecting underlying vascular malformations and malignancy in the setting of an intracranial hemorrhage
- CT
- Imaging recommendations
- Start with NECT
- If etiology is clear from history, no need for further imaging
- If unclear, recommend CTA to evaluate for underlying vascular malformation or thrombosis
- MRI with contrast and T2* sequence
- If CT negative or etiology unclear
- If a vascular etiology is suspected, recommend CTA, MRA, or MRV
- Recommend follow-up MRI or DSA if etiology remains unclear, because a recent hematoma could mask an underlying tumor or vascular lesion
- Dual-energy CT can be a useful tool for detecting underlying tumors in patients with an intracranial hemorrhage of unknown origin
- Start with NECT
- Mimic
- On initial imaging, it can be difficult to distinguish bland hematoma from a vascular malformation or hemorrhagic neoplasm. If initial MRI or angiography is not helpful in delineating the underlying etiology, follow-up MRI or conventional angiography might be necessary. More recent studies suggest that initial evaluation with dual-energy or spectral CT could help identify the underlying etiology.
For more information, please see the corresponding chapter in Radiopaedia.
Contributor: Sean Dodson, MD
References
Bell D, Grant R, Collie D, et al. How well do radiologists diagnose intracerebral tumour histology on CT? Findings from a prospective multicentre study. Br J Neurosurg 2002;16:573–577.
Kim SJ, Lim HK, Lee HY, et al. Dual-energy CT in the evaluation of intracerebral hemorrhage of unknown origin: differentiation between tumor bleeding and pure hemorrhage. AJNR Am J Neuroradiol 2012;33:865–872. doi.org/10.3174/ajnr.A2890
Postma AA, Das M, Stadler AAR, et al. Dual-energy CT: what the neuroradiologist should know. Curr Radiol Rep 2015;3:16. doi.org/10.1007/s40134-015-0097-9
Please login to post a comment.