Spinal Vascular Anatomy
The spinal cord circulation is derived from segmental branches arising from the vertebral arteries, as well as multiple radicular arteries arising from segmental vessels in parallel, including the descending cervical, deep cervical, intercostal, lumbar, and sacral arteries. The venous drainage of the spinal cord is more symmetric and redundant when compared to the arterial system with both minimal anterior to posterior and right to left segmental variation.
Spinal Arterial System
Embryology Overview
Vertebral artery
- Embryogenesis between approximately day 32 and day 40
- Formed from fusion of the longitudinal anastomoses that link cervical intersegmental arteries, which branch from the primitive paired dorsal aorta
- Intersegmental arteries regress
- The seventh Intersegmental arteries remain to form the proximal subclavian artery, including the origin of the vertebral artery
- As the connections to the primitive dorsal aorta disappear, the vertebral artery takes shape and initially has a more beaded anastomotic appearance and a tortuous course
- Basilar artery is formed by fusion of the two primitive vertebral arteries
Spinal Arteries
- Originate from a ventral network on the cord surface connected with segmental aortic branches
- Two primitive longitudinal systems are formed, later becoming a single longitudinal solitary anterior median anterior spinal artery
- Anterior spinal artery formation is followed by a variable regression of segmental feeding vessels and is completed by the fourth month
- Regression is most pronounced in the thoracic and lumbar areas.
- Segmental arteries persist as intercostal and lumbar arteries.
Anatomy
Vertebral Arteries (VA): 4 Segments
- V1 - Extraosseous segment
- Origin from each subclavian artery, coursing superiorly to enter the C6 transverse foramen (80-90%)
- Variations
- Origin of the left vertebral artery from the aortic arch between the left common carotid artery and left subclavian artery has been described in 2-6% of cases
- Origin of the vertebral artery from the arch, enters the C5 transverse foramen in majority of cases
- Origin of the left vertebral artery from the left common carotid artery or external carotid artery (rare)
- Origin of the right vertebral artery from the aorta, carotid arteries, or brachiocephalic arteries (rare)
- Important branches
- Segmental cervical muscular branches
- V2 - Foraminal segment
- ascends from C6 to C2
- Important branches
- Anterior meningeal artery arising between C2 and C3 level
- V3 - Extraspinal segment
- makes a wide extracervical loop between C2 and C1
- prone to dissection/pseudoaneurysm
- Exits top of atlas (C1) transverse foramen
- Lies superior to C1, curving posteromedially around atlantooccipital joint
- Passes posteriorly over the atlanto-occipital joint, turns sharply anterosuperiorly to enter dura at foramen magnum
- Variations
- Persistent first intersegmental artery - vertebral artery courses below the C1 arch after exiting the transverse foramen of C2 and enters the spinal canal without passing through the C1 transverse foramen (3-4%)
- Important branches
- Posterior meningeal artery
- supplies the falx cerebelli and the medial dura of the occipital posterior fossa
- Posterior meningeal artery
- V4 - Intradural, (intracranial)
- Enters the cranium via the foramen magnum.
- Important Branches:
- Anterior spinal artery (1)
- Posterior spinal arteries (2)
- Medullary perforators
- Posterior Inferior Cerebellar Arteries (PICA) originate from this segment with variations
- See also the cranial vascular anatomy chapter for more detailed description and images of the intracranial posterior circulation.
- Variations
- Vertebral artery terminates in the PICA (does not join to form basilar artery)
Figure 1: Axial CT Angiogram neck with contrast. This image demonstrates the most common variant of the aortic arch – an aberrant right subclavian artery (green arrow). This artery variation typically traverses posteriorly to the trachea/esophagus and can result in dysphagia for the patient called dysphagia luscoria. The other vessel origins from the aortic arch are as follows: left subclavian artery (yellow arrow), left common carotid artery (blue arrow), and the brachiocephalic trunk (purple).
Figure 2: CT Angiogram of the neck – maximal intensity projection 3-D reformat, posterior oblique view. This image demonstrates a common variant in which the left vertebral artery arises from the aortic arch (green), creating a four vessel aortic arch. The other artery origins from the aortic arch are as follows: left subclavian artery (yellow arrow), left common carotid artery (blue arrow), and the brachiocephalic trunk (purple). There is a conventional origin of the right vertebral artery origin from the left subclavian artery (red arrow).
Figure 3: Conventional cerebral angiogram with digital subtraction images to review the posterior circulation in the anterior-posterior projection. The catheter is injecting angiographic contrast through the left vertebral artery (yellow arrow) which demonstrates the most distal branch, the posterior inferior cerebellar artery (green arrow). Other artery branches that are included in the image: anterior inferior cerebellar artery (purple arrow), basilar artery (blue arrow), superior cerebellar artery (red arrow), and posterior cerebral artery (pink arrow).
Figure 4: Conventional cerebral angiogram with digital subtraction images of the posterior circulation in the lateral projection. Again the catheter is injecting angiographic contrast into the left vertebral artery (yellow arrow). The distal most branch from the vertebral artery is the posterior inferior cerebellar artery (green arrow). The basilar artery is marked with the blue arrow.
Anterior spinal artery (1)
- Just before joining to form the basilar artery, each of the vertebral arteries give off a branch that joins the corresponding branch from the contralateral vertebral artery to become the anterior spinal artery, which extends caudally
- Lies in the midline on a ventral aspect of the cord, in the groove of the anterior median fissure
- Reinforced by segmental feeders, give rise to central branches which supply the anterior 2/3 of the cord (anterior horns, spinothalamic tracts, and corticospinal tracts)
Posterior spinal arteries (2)
- Originate from the posterior inferior cerebellar arteries or from the intracranial portion of the vertebral arteries.
- Paired longitudinal system of vessels on the dorsal cord medial to the dorsal roots.
- Form a plexiform network between the two arteries.
- Supplies the posterior 1/3 of the cord (posterior columns, with variable supply to the corticospinal tracts).
Figure 5: Axial MRI of the thoracic spine at the T11 vertebral body level with contrast. There are only a couple of arteries that can be identified on MRI lining the spinal cord. Anteriorly, one can typically see the anterior spinal artery (green arrow) while posteriorly, one can typically see one or two of the posterior spinal arteries (yellow arrow). The vessels along the lateral aspect of the spinal canal is the internal vertebral venous plexus (blue arrow).
Segmental anastomoses
- Continuation of both the anterior and posterior spinal arteries in the lower cervicothoracic region and derived from segmental anastomoses. Depending on patterns of embryologic regression, there tends to be an inverse relationship between number and caliber of anterior segmental vessels.
- Posterior intercostal arteries
- Arise from the paired intercostal arteries from the aorta or costocervical trunk of the subclavian artery
- ~11 posterior intercostal arteries on each side
- The 1st and 2nd posterior intercostal arteries arise from the supreme intercostal artery, a branch of the costocervical trunk of the subclavian artery
- The lower nine arteries are the aortic intercostal arteries, so called because they arise from the posterior aspect of the thoracic aorta
- Arise from the paired intercostal arteries from the aorta or costocervical trunk of the subclavian artery
- Segmental arteries arise from the posterior intercostal arteries, numbered by segment level from which they arise, enter the canal through the neural foramen, penetrate the dura, dividing into two main branches:
- Radiculomeningeal (Dural artery), which supplies the nerve root sleeve and the dura
- Radiculomedullary artery
- Radicular artery
- anterior (supply anterior nerve roots)
- posterior (supply posterior nerve roots)
- Medullary artery
- Joins and reinforces the anterior spinal artery and posterior spinal artery
- Dominant cervical radiculomedullary artery (Artery of Lazorthes)
- Occurs between the C5-C7 levels
- Dominant thoracic radiculomedullary artery (Artery of Adamkiewicz)
- Tends to have a left-sided origin (75%) and arises from T9-T12 (60%)
- Less common origins in the lumbar region (25%) and from T6-T8 (10%)
- A dominant upper thoracic (T5 level) radiculomedullary artery is less common (artery of von Haller)
- Posterior thoracic arterial feeding vessels
- Approximately 8 levels
- No right or left lateralization.
- Arterial basket of the conus medullaris
- anterior spinal artery ends at the conus medullaris with variable communicating branches to the posterior spinal artery
- Iliac artery gives rise to the inferior and superior lateral sacral branches, which give rise to the spinal arteries via the anterior sacral foramen
- May also supply the conus medullaris via the cone or conus artery arising from the internal iliac (artery of Desproges-Gotteron)
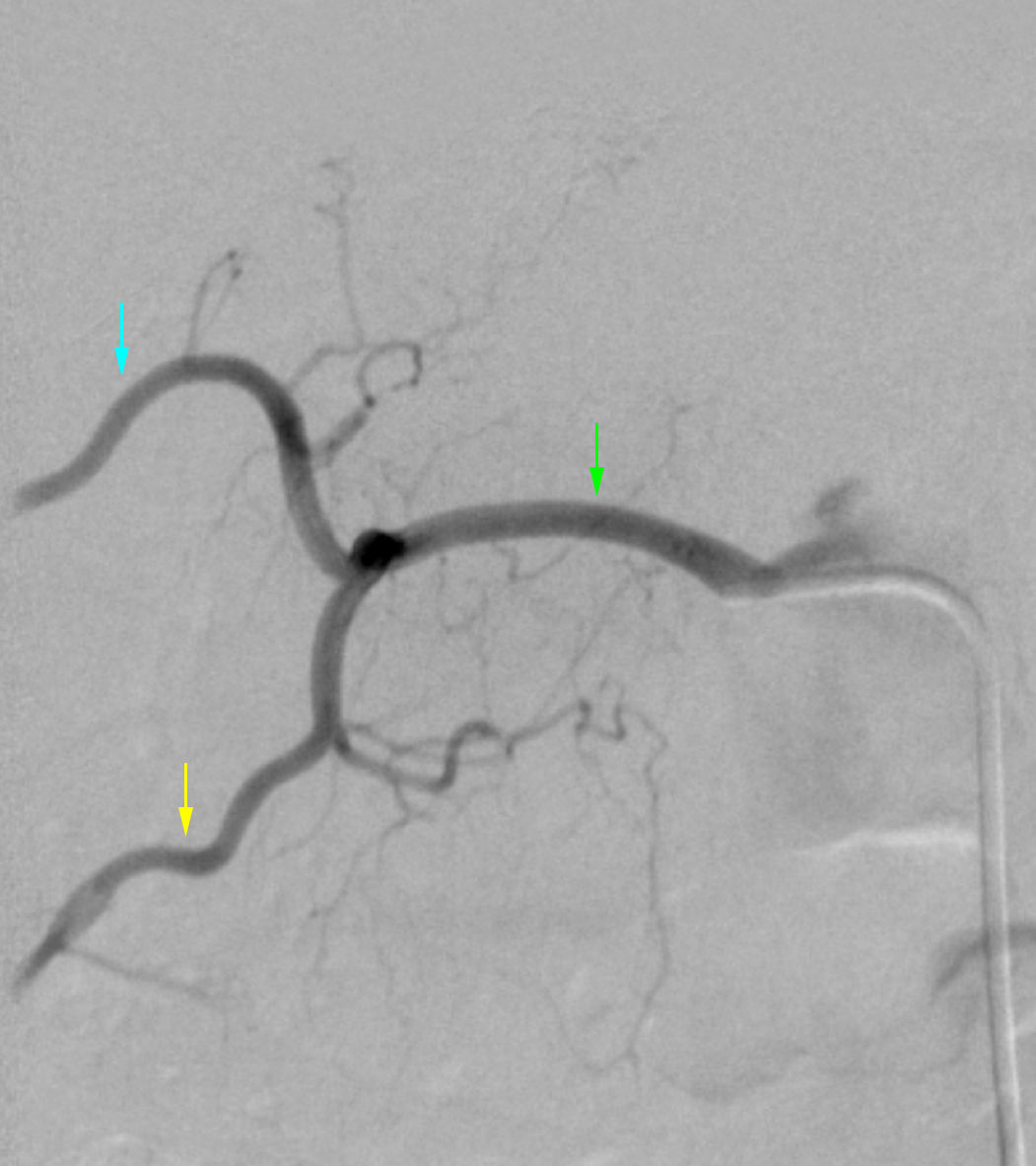
Figure 6: Conventional spinal angiogram utilizing digital subtraction angiography. These images demonstrate the supreme intercostal origin of the cervical spinal artery (blue arrows) which is occasionally visualized but can be difficult to catherize at times.
Figure 7: Conventional angiogram of the spinal arteries. The spinal arteries can opacify a single lumbar level, however, on occasion there may be a common trunk which supplies two levels. This image demonstrates a common trunk (green arrow) that supplies the T11 spinal artery (blue arrow) in addition to supplying the T12 spinal artery (yellow arrow).
Figure 8: Conventional spinal angiogram with digital subtraction angiography technique. Common lumbar spinal artery trunks are also quite common, especially in the lower lumbar spine. This image demonstrates a common trunk (green arrow) for the right L5 lumbar spinal artery (yellow arrow) as well as the left L5 lumbar spinal artery (blue arrow). The artery descending inferiorly is the middle sacral artery (purple artery).
Figure 9: Conventional angiogram with utilization of digital subtraction angiography technique. This angiogram is at the level of the right L1 lumbar artery which demonstrates the Artery of Adamkiewicz, the largest anterior segmental medullary artery (blue arrows). This artery ascends on the mid-sagittal anterior surface of the spinal cord, usually less than 2.5 vertebral body lengths. This image demonstrates the classic hairpin turn at its anastomosis with the anterior spinal artery (green arrow). The radiculomedullary artery (yellow arrow) often demonstrates a small segment of narrowing at the point where the artery pierces the dura of the spinal canal (purple arrow).
Vertebral and Spinal Venous System
Typically, the intrinsic cord venous drainage consists of paired radial draining veins, which drain into the anastomoses on the cord surface. Central veins in the anterior median fissure provide for venous return from the anterior horns and surrounding white matter and form the anterior median vein. The anterior median vein continues caudally along the filum terminale to the end of the thecal sac. The median veins drain to the “trans-dural” medullary (radicular) veins, which leave the intradural space at the root sleeve.
Peripheral and dorsolateral cord drainage is via the radial venous plexus, which extends to the coronal venous plexus on the cord surface, and then drains to the epidural venous plexus (of Batson), plexiform venous channels located at the anterior and posterior midline and antero- and posterolaterally along the line of attachments of the dorsal and ventral rootlets, a
continuous system from the sacrum to the skull base.
Connections with the azygos and hemiazygos venous systems include the vertebral and deep cervical veins (cervical); the intercostal-segmental veins (thoracic); segmental veins connected by the ascending lumbar vein (lumbar). Additionally, the basivertebral veins (intravertebral body), anterior plexus (vertebral body) and posterior plexus (posterior elements) components connect with the superior and inferior vena cava, azygos and hemiazygos systems, and the intracranial dural sinuses.
Intradural veins
Intrinsic cord venous system
- Central and peripheral groups of radial veins drain into anastomoses on the cord surface
- Central group
- Provides return for anterior horns and surrounding white matter
- Drain into central veins in anterior median fissure
- Anterior median vein
- Peripheral dorsolateral group
- Drainage via radial venous plexus to the pial covering of the spinal cord
- Coronal venous plexus on cord surface
- Posterior median vein
- Drains to epidural venous plexus of Batson
- Central group
- Anterior median vein
- Continues caudally along the filum terminale to end of dural sac
- Coronal, median veins drain to medullary veins
- “Trans-dural” medullary veins
- Drain the median veins
- Valveless with functional valve-like mechanism at dural margin
- Leave the intradural compartment at the root sleeve
- Site of spinal dural arteriovenous fistulas
- Epidural plexus
- Surrounds thecal sac
- Drains the medullary veins
- Continuous system from the sacrum to the skull base
- Plexiform venous channels (x6)
- Anterior and posterior midline (x2)
- Antero- and posterolaterally along the line of attachments of the dorsal and ventral rootlets (x4)
- Anastomotic connections to SVC, IVC, azygos/hemiazygos systems, intracranial dural sinuses
- Vertebral venous system
- Large valveless network of the vertebral column
- Extends from sacral hiatus to foramen magnum, ends in the clival plexus, suboccipital sinus
- Highly redundant collaterals, anastomoses
- Three major external complexes:
- Internal
- Basivertebral veins
- External venous complexes
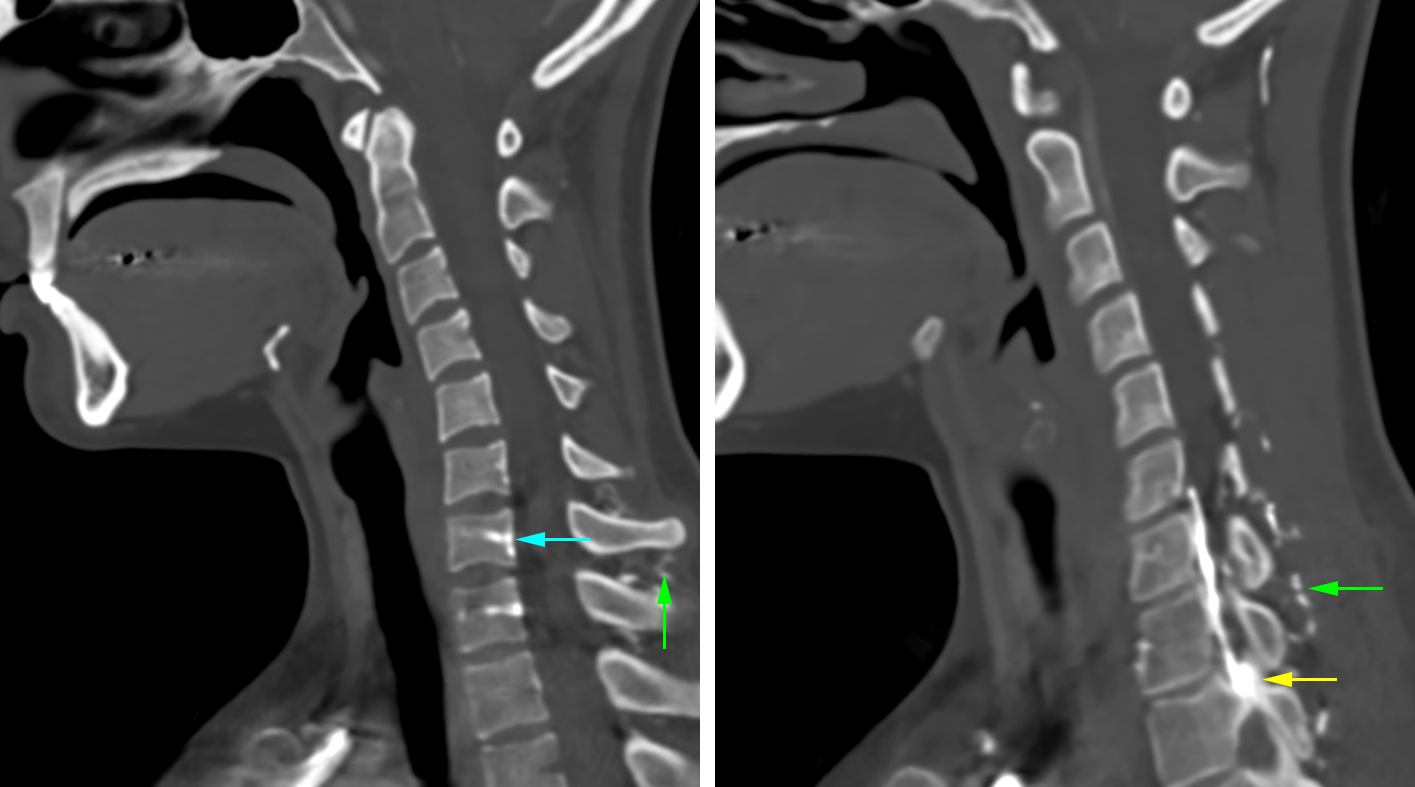
Figure 10: CT angiogram of the neck at the T1 vertebral body with contrast. This image demonstrates the venous plexus that surrounds the spinal canal. Along the posterior aspect of the vertebral body, there is demonstration of the Batson’s venous plexus (blue arrow). From the Batson’s venous plexus centrally, there are additional veins that extend laterally called the anterior epidural venous plexus (green) and travel within and around the corresponding nerve sheaths (yellow arrow) called emissary veins. The vessels that travel through the vertebral body from the Batson’s venous plexus correspond to the basivertebral veins (purple).
Figure 11: Sagittal CT Angiogram of the neck with contrast. The venous plexus surrounding the spinal canal can be visualized occasionally on a CT Angiogram. The Batson’s venous plexus is located along the posterior aspect of the vertebral body (blue arrow). Additionally, there are veins that extend from the Batson’s venous plexus laterally to the level of the neuroforamina which are medullary veins (yellow arrow). There is also an extensive venous network which surround the spinous processes which are referred to as the paraspinal venous network (green).
Figure 12: Coronal CT angiogram of the neck with contrast. The venous plexus occasionally can be visualized on a CT angiogram. On this coronal image, the venous network is within and surrounding the corresponding nerve sheaths (blue arrow) which are called emissary veins.
Figure 13: Axial MRI image of the lumbar spine at the L1 vertebral body level with contrast. With contrast administration, along the anterior aspect of the spinal canal, the Batson’s venous plexus is highlighted (blue arrow). There are additional veins that are extending through the central aspect of the vertebral body corresponding to the basivertebral vein (yellow arrow).
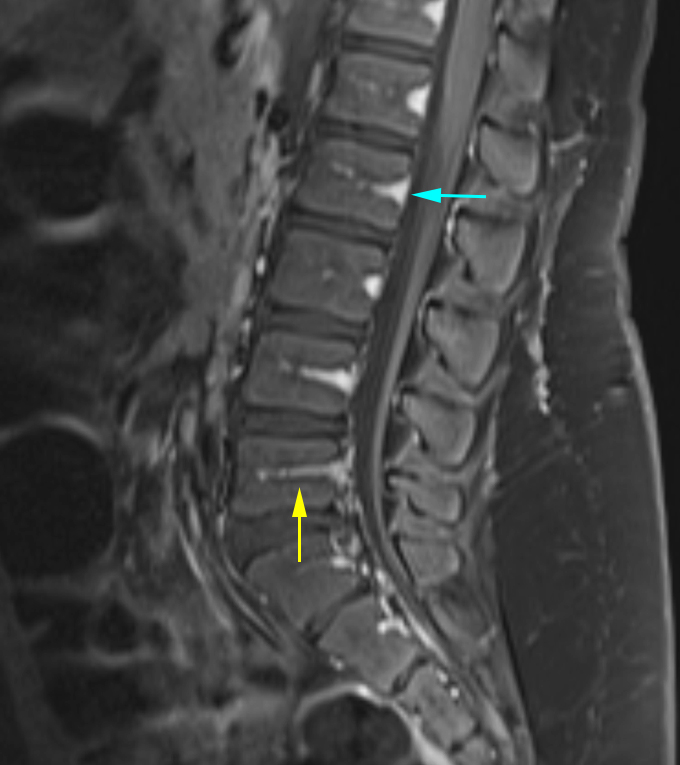
Figure 14: Sagittal MRI image of the lumbar spine with contrast. This image demonstrates the Batson’s venous plexus along the anterior spinal canal (blue arrow). Additionally, there are small veins running through the vertebral body from the Batson’s venous plexus called the basivertebral veins (yellow arrow).
Contributors: Katie Traylor DO, Daniel Murph MD
References
Gailloud P: The artery of von Haller: a constant anterior radiculomedullary artery at the upper thoracic level. Neurosurgery. 73(6):1034-43, 2013
Eskander MS, Drew JM, Aubin ME, Marvin J, Franklin PD, Eck JC, Patel N, Boyle K, Connolly PJ: Vertebral artery anatomy: a review of two hundred fifty magnetic resonance imaging scans. Spine (Phila Pa 1976). 35(23):2035-40, 2010
Becske T, Nelson PK: The vascular anatomy of the vertebro-spinal axis. Neurosurg Clin N Am. 20(3):259-64, 2009
Bell R, Severson MA, Armonda RA: Neurovascular anatomy: a practical guide. Neurosurg Clin N Am. 20(3):265-78, 2009
Debette S, Leys D: Cervical-artery dissections: predisposing factors, diagnosis, and outcome. Lancet Neurol. 8(7):668-78, 2009
Goyal MS, Derdeyn CP: The diagnosis and management of supraaortic arterial dissections. Curr Opin Neurol. 22(1):80-9, 2009
Johnson MH, Thorisson HM, DiLuna ML: Vascular anatomy: the head, neck, and skull base. Neurosurg Clin N Am. 20(3):239-58, 2009
Kim YK, Schulman S: Cervical artery dissection: pathology, epidemiology and management. Thromb Res. 123(6):810-21, 2009
Tubbs RS, Shah NA, Sullivan BP, Marchase ND, Cohen-Gadol AA: Surgical anatomy and quantitation of the branches of the V2 and V3 segments of the vertebral artery. Laboratory investigation. J Neurosurg Spine. 11(1):84-7, 2009
Wang S, Wang C, Liu Y, Yan M, Zhou H: Anomalous vertebral artery in craniovertebral junction with occipitalization of the atlas. Spine (Phila Pa 1976). 34(26):2838-42, 2009
Bagheri SC, Khan HA, Bell RB: Penetrating neck injuries. Oral Maxillofac Surg Clin North Am. 20(3):393-414, 2008
Chen JW: Cervical spine injuries. Oral Maxillofac Surg Clin North Am. 20(3):381-91, 2008
Turan TN, Chimowitz MI: Treatment of intracranial atherosclerotic stenosis. Rev Neurol Dis. 5(3):117-24, 2008
Schmidt WA: Takayasu and temporal arteritis. Front Neurol Neurosci. 21:96-104, 2006
Nelson PK, Setton A, Berenstein A: Vertebrospinal angiography in the evaluation of vertebral and spinal cord disease. Neuroimaging Clin N Am. 6(3):589-605, 1996
Berenstein A, Lasjaunias, P. Surgical Neuroangiography, Volume 5. Endovascular Treatment of Spine and Spinal Cord Lesions. Springer-Verlag, New York, 1992.
Choi IS. Spinal arteriovenous metameric syndrome: angioarchitecture and their prognosis. AJNR Am J Neuroradiol. 2013 Feb;34(2):464-5. doi: 10.3174/ajnr.A3318. Epub 2012 Aug 30.
Clarke MJ, Patrick TA, White JB, Cloft HJ, Krauss WE, Lindell EP, Piepgras DG: Spinal extradural arteriovenous malformations with parenchymal drainage: venous drainage variability and implications in clinical manifestations. Neurosurg Focus 26(1):E5, 2009.
Ferrell AS, Tubbs RS, Acakpo-Satchivi L, Deveikis JP, Harrigan MR. Legacy and current understanding of the often-misunderstood Foix-Alajouanine syndrome. Historical vignette. J Neurosurg. 2009 Nov;111(5):902-6. doi:10.3171/2007.11.17656.
Hurst R, Rosenwasser R. Interventional Neuroradiology. 2008.
Niimi Y, Uchiyama N, Elijovich L, Berenstein A. Spinal arteriovenous metameric syndrome: clinical manifestations and endovascular management. AJNR Am J Neuroradiol. 2013 Feb;34(2):457-63. doi: 10.3174/ajnr.A3212. Epub 2012 Aug 2.
Novy J, Carruzzo A, Maeder P, Bogousslavsky J. Spinal Cord Ischemia: Clinical and Imaging Patterns, Pathogenesis, and Outcomes in 27 Patients. Arch Neurol. 2006;63(8):1113-1120. doi:10.1001/archneur.63.8.1113.
Shapiro M, et al. Neuroangio. http://neuroangio.org. 2015.
Spetzler RF, Kim LJ. Classification and Surgical Management of Spinal Arteriovenous Lesions: Arteriovenous Fistulae and Arteriovenous Malformations. Neurosurgery. Vol 59. Num 5. Nov Supplement 2006. S3-195.
Thron AK. Vascular anatomy of the spinal cord. Wien, New York: Springer, 1988.
Please login to post a comment.