Giant and Multicompartmental Pituitary Adenomas
This is a preview. Check to see if you have access to the full video. Check access
Resection of a Giant Pituitary Adenoma
Please note the relevant information for patients suffering from pituitary adenomas is presented in another chapter. Please click here for patient-related content.
Giant pituitary adenomas are usually described as tumors larger than 4 cm that generally extend within 6 mm of the foramen of Monro. They are reported in 5% to 14% of surgical pituitary tumor series. The histologic characteristics of giant pituitary adenomas do not correlate with their size or invasive nature; most of these tumors contain benign cells.
Most giant pituitary adenomas require surgical excision. An exception to this rule is the rare giant prolactinoma, which has a high rate of response and regression with dopamine agonist therapy.
Over the last century, surgery for giant pituitary adenomas has evolved from transcranial macrosurgical techniques associated with significant morbidity to transcranial microsurgical techniques, and ultimately to endonasal endoscopic transsphenoidal approaches with improved patient outcomes.
However, in inexperienced hands, the transnasal approaches can potentially result in subtotal resection of pituitary tumors and especially the giant ones. The residual tumor can induce a postoperative apoplectic event, leading to irreversible neurologic deterioration including blindness and thalamic dysfunction.
Many classification systems have been used to describe multicompartmental pituitary adenomas. Yasargil classified those tumors into four subgroups: 1) suprasellar-suprachiasmatic: tumors that grow more than 2 cm above the planum sphenoidale and in front of the chiasm, 2) suprasellar-retrosellar: tumors that extend into the interpenduncular cisterns, 3) parasellar-cavernous: tumors that extend into the cavernous sinuses, and 4) paninvasive: tumors that extend in all directions.
Similarly, Hardy initially classified tumors into four types: (A) tumors with extension into chiasmatic cisterns, (B) tumors with extension into the third ventricle, (C) tumors with extension toward the foramen of Monroe, and (D) tumors extending into the anterior or middle cranial fossae. A modified Hardy classification was subsequently constructed in which grade C tumors with 3 cm of extension into the third ventricle and grade D tumors with more than 3 cm of extension beyond the foramen of Monroe, each with at least 2 cm of extension superior to the jugum sphenoidale, were considered giant macroadenomas.
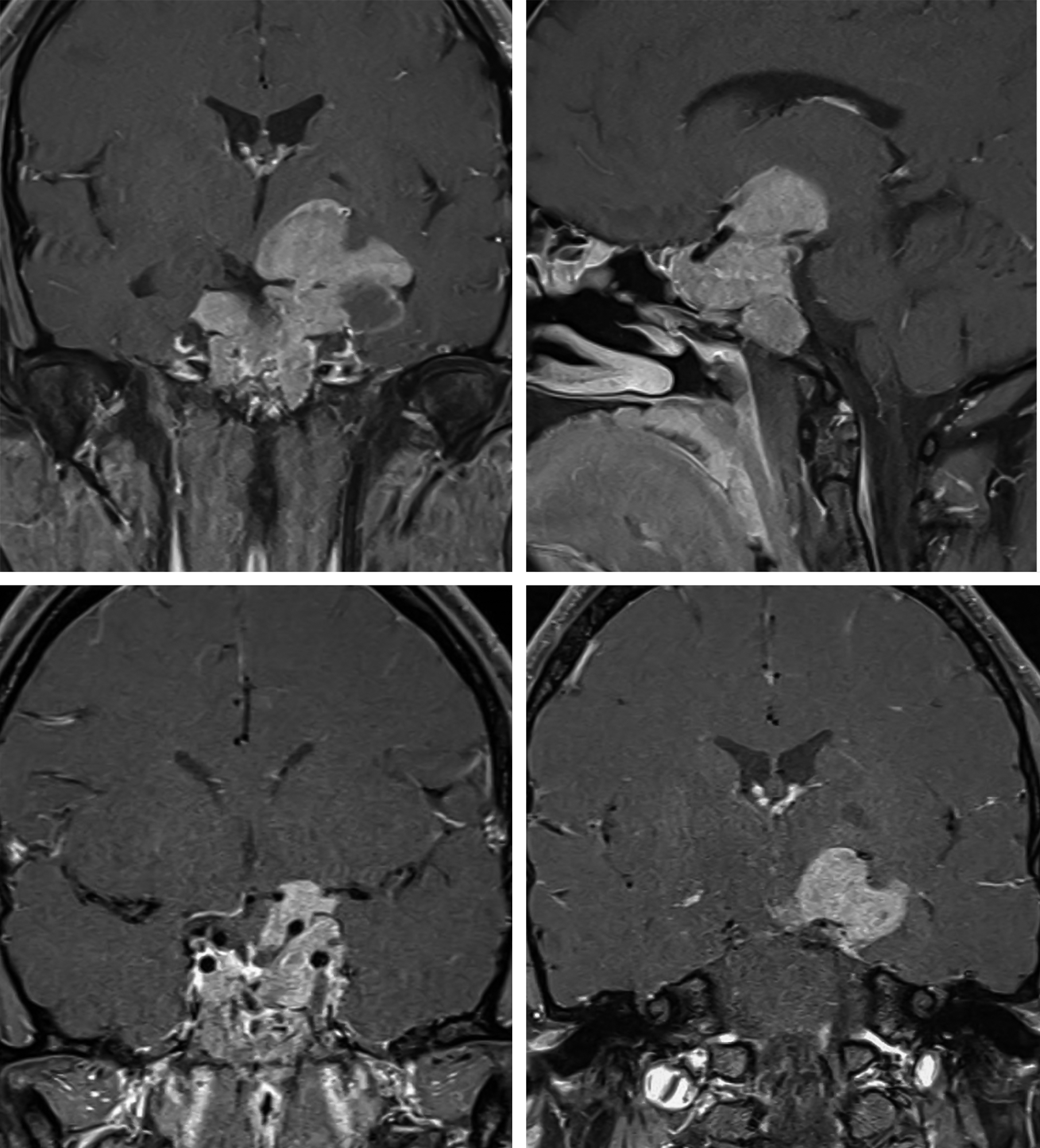
Figure 1: Giant pituitary adenomas can present in a variety of shapes; the morphology of the tumor can significantly affect the technical difficulty of resection. A compact globular morphology is shown in the images in the top row. Cavernous sinus invasion is not evident. Endoscopic endonasal transsphenoidal surgery is effective in gross total tumor resection while preserving the pituitary gland (bottom row).
Figure 2: The asymmetric tumors with significant cavernous sinus invasion are included (top row of images); this morphology provides more technical challenges and effective resection is unlikely. Transsphenoidal surgery was successful for removal of the majority of this partially cystic tumor, but the lateral intracavernous component was not reachable (bottom row). Please note the fat packing in the sella.
Figure 3: The mutilobulated and asymmetric morphology of this tumor led to a number of challenges during its resection due to the very narrow operative corridors available to reach the tumor’s apex. The initial endoscopic transsphenoidal transcavernous approach relieved the mass effect on the optic apparatus, but only part of the tumor was removed (bottom row of images). A transcranial (pterional) operation was subsequently undertaken.
Operative Anatomy as Related to Tumor Extension into the Cavernous Sinus
The cavernous sinuses are extradural vascular spaces and are formed by the space between the meningeal and endosteal layers of the medial part of the middle fossa dura. The medial wall of the cavernous sinus contains two parts: sellar and sphenoidal. The sellar part separates the pituitary gland from the contents of the cavernous sinus. The sphenoidal part lies lateral to the body of sphenoid bone and is related to the carotid sulcus. The lateral wall of the cavernous sinus is composed of two layers. The endosteal layer encases the cranial nerves traversing the lateral wall of this venous sinus.
The intracavernous carotid artery may be in direct contact with the lateral edge of the pituitary gland or separated by a venous space.
Click here to view the interactive module and related content for this image.
Figure 4: The medial wall of the cavernous sinus with its relationship to the cavernous carotid and the pituitary gland are shown (upper photos). Please note the location of the abducens nerve within the cavernous sinus and the position of the vidian nerve in relation to the carotid artery (middle and bottom photos). (Images courtesy of AL Rhoton, Jr.)
The degree of cavernous sinus invasion is usually described using the Knosp-Steiner Criteria. Knosp described this criterion based on evaluation of coronal magnetic resonance (MR) imaging scans that include the gland and the cavernous carotid arteries. Grade 0: no invasion of the medial wall of the cavernous sinus; Grade 1: the tumor extends up to the medial aspect of the cavernous carotid artery; Grade 2: the tumor extends to the lateral aspect of the artery; Grade 3: the tumor extends lateral to the artery, but does not fill the cavernous sinus; Grade 4: the tumor fills the cavernous sinus.
Diagnosis, Indications for Surgery, and Preoperative Considerations
Please refer to the chapter discussing Pituitary Macroadenoma in the Brain Tumor Volume.
EXTENDED ENDOSCOPIC ENDONASAL APPROACH TO GIANT PITUITARY ADENOMA
Transcranial approaches have traditionally been described for management of giant pituitary adenomas. However, in experienced hands, the extended endoscopic endonasal approaches with their broadened operative trajectories have almost eradicated the need to use transcranial corridors for resection of giant tumors. I do not believe combined/concurrent transnasal and transcranial approaches are necessary for even the most giant tumors.
Indeed, the endoscopic approach provides improved resolution for differentiating tumor from anatomically normal tissue when compared with microscopic transcranial approaches. Importantly, the improved endoscopic visualization allows safer and more aggressive intrasellar microsurgery to remove the difficult-to-reach components of the giant tumors. This approach is also the most practical route to the tumor in the retrochiasmatic space. The practical transcranial approaches to this specific region are limited.
When comparing the traditional microscope-assisted transsphenoidal approach with the endoscopic endonasal approach, the latter operative route allows resection of the planum sphenoidale and tuberculum sellae, providing an additional unobstructed view of the suprasellar extension of the multicompartmental tumors.
Similarly, an extended approach affords wide visualization of the clivus and unobstructed resection of adenomas that extend posterior to the sphenoid sinus.
Furthermore, the extended endoscopic approach permits resection of the tumor extending into the cavernous sinus from a mediolateral viewpoint via angled endoscopes and dissectors. The mediolateral operative course minimizes injury to the neurovascular structures that are located on the lateral wall of the dural sinus.
Following or “chasing” the tumor from the sella into the cavernous sinus and its decompression provides and creates the most effective corridor for safe and efficient transcavernous tumor removal along the relatively less visualisable operative corners. Blind tumor manipulation is a recipe for disaster and often leads to perforator avulsion.
Residual tumor that is unresectable from the extended transnasal approach may be removed through transcranial approaches, treated with stereotactic radiation, or monitored conservatively.
I prefer to install a lumbar drain immediately preoperatively in most patients who have a giant pituitary adenoma. Injection of a modest amount of air during the later stages of tumor resection can potentially aid with the much-needed diaphragmatic descent, delivering the tumor that is not readily deliverable into the operative cavity.
Patient Setup and Approach
Some details of transnasal endoscopy are briefly reiterated here. The patient is positioned supine with his or her head on a “horseshoe” to allow for dynamic intraoperative head repositioning. The head is slightly extended and elevated to promote venous drainage. Furthermore, the head should be turned 15 to 20 degrees toward the lead surgeon to facilitate the operator’s ergonomic body posture.
The extent of skull base resection may guide the need for a fat or fascia lata grafts. Regardless, it is ideal to prepare and drape the abdomen and the thigh in case the nasal septal flap is insufficient for prevention of a postoperative cerebrospinal spinal fluid leak.
I like to stand across the operating table from my rhinologist colleague because I am left-handed and he is right handed. The patient’s head is turned slightly toward me during the microsurgical part of the operation so that I do not need to lean forward. The surgical assistant and operative instruments are positioned on the side of the operating table, contralateral to the neurosurgeon, so that instruments can be readily transferred.
Once the patient is appropriately prepped and draped, the endoscope is inserted into either the left or right nostril. Throughout the operation, it is important to avoid traumatizing the nasal mucosa during the passage of the instruments. The middle turbinate is mobilized laterally, revealing the superior turbinate. The superior turbinate is then also retracted laterally to expose the sphenoid ostia.
The mucosa surrounding the sphenoid ostia is coagulated and the posterior portion of the nasal septum and vomer are removed to increase the operative field of view and permit the use of surgical instruments through both nostrils. Next, the entire rostral wall of the sphenoid sinus is removed using Kerrison rongeurs. The bone at the floor of the sella is very thin and at times nonexistent in giant tumors. Invasive tumors erode through the dura and fill the sphenoid sinus, obliterating all important operative anatomic landmarks.
During removal of the lateral sphenoid septa, the surgeon diligently resects the bone over the carotid arteries. Preoperative CT/CT angiography allows adequate visualization of the course of the carotid arteries and their relationship to the sphenoid sinus. If the tumor extends over the tuberculum sellae or planum sphenoidale, partial removal of the posterior ethmoid sinuses may be needed.
The optic and carotid protuberances and the opticocarotid recesses are identified for anatomic orientation. Bone removal extends over the medial edges of both cavernous sinuses. Inadequate bone removal is the most common cause of subtotal tumor resection. This principle is especially applicable to giant tumors that resist the descent of their suprasellar portion if their lateral extensions into the sella are not addressed because of restricted bone exposure.
Next, the opening of the sellar floor is extended anteriorly to include the posterior part of the tuberculum. Further skull base bone removal (such as clivus resection) is dictated by the particulars of each tumor. Again, generous bone exposure is the key maneuver when handling giant tumors that frequently resist the descent of their suprasellar capsule into the sella. If I am unable to inspect the medial walls of the cavernous sinuses and assure effective removal of the lateral tumor capsule, I am most likely unable to promote the descent of the “head of the snowman” (the common shape of these tumors).
Figure 5: The inadequate extent of bone removal at the lateral and anterior floor of the sella (“traditional” bone removal for “standard” macroadenomas) precludes the operator from reaching the lateral and anterior borders of giant tumors. Suboptimal removal of the lateral edges of the tumor will prevent the descent of the symptomatic suprasellar section.
Resection
The normal pituitary gland should be estimated on MR imaging, and the initial dural incision should be directed away from the gland and carotid arteries. The dura is opened in the form of a cruciate incision and the flaps of dura are retracted away via their bipolar coagulation. The microDoppler is a helpful adjunct in localization of the cavernous carotid arteries during completion of dural incisions.
Tumor removal starts with central internal decompression using the suction device and ring curettes. I often use two suction devices to remove easily deliverable tumor efficiently. Almost all giant tumors are soft and frequently cystic. If the tumor is firm, an ultrasonic aspirator is utilized under direct vision.
The order of operative steps for tumor removal is important because it helps prevent premature herniation of the arachnoid and/or diaphragma sellae into the resection cavity, which would obstruct the field of view and decrease the chance for an adequate resection.
First, the inferior and central portion of the tumor should be debulked followed by the lateral portions: I resist the temptation to remove the readily visible anterosuperior portions of the tumor as this would cause the diaphragm to prematurely descend, obscuring the lateral poles of the tumor. If the tumor is well circumscribed within the sella (for example, no extension into the cavernous sinus is apparent), then the lateral tumor capsules can be peeled away from the medial wall of the sinus.
If the tumor extends into the cavernous sinus, then the tumor is “chased” into the dural venous sinus; stepwise tumor debulking will provide additional space for exposure of the tumor components residing within the sinus. Opening the cavernous sinus lateral to the carotid artery is possible and should be done with great caution. MicroDoppler mapping is mandatory to avoid vascular injury.
A “conservative strategy” for intracavernous tumor removal is advised. Neurophysiological monitoring and stimulation mapping of the abducens and oculomotor nerves is necessary for the transcavernous approach as the intracavernous septations and clinoidal ligaments can be mistaken for the nerves, leading the surgeon to stop too soon. Please see the Endoscopic Cavernous Sinus Surgery chapter for more details.
Following aggressive removal of the lateral tumor extensions, the suprasellar portion of the mass is evacuated. The tumor should be debulked internally because this maneuver will facilitate the tumor capsule to collapse down into the sella. Another common cause of inadequate tumor descent is limited central tumor debulking. If the tumor fails to descend despite its aggressive enucleation (for example, when the tumor is firm and adherent), transtubercular and transplanum routes may facilitate visualization of the edge of the anterior/top of the tumor capsule and its mobilization into the sella. Injection of air into the lumbar drain (10 cc aliquots, maximum of 60 cc) is also reasonable.
The diaphragm of giant tumors becomes quite patulous during tumor removal, and sizable tumor remnants may be easily overlooked within these folds. In addition, hour-glass-shaped tumors with a small diaphragmatic hiatus can offer special challenges to the operator who is attempting to expose the symptomatic suprasellar part of the mass. In these situations, the endoscope, with its panoramic field of view, allows me to use blunt dissectors to manipulate the diaphragmatic folds relatively atraumatically while additional tumor fragments are delivered out of the limited spaces between these folds.
Figure 6: The patulous folds of the diaphragm are shown after portions of the giant adenoma have been resected. The cleft where the suction device is located most likely contains additional tumor fragments tracking into the suprasellar space.
Figure 7: I also employ hydroscopy to elevate the folds and inspect the tumor contents within the clefts. The operator should remain patient to allow the tumor fragments to descend intraoperatively via the use of the Valsalva maneuver and intrathecal air injections through the lumbar drain.
I find the “four-hand” technique especially useful here. My ENT colleague uses an angled ring curette over a small piece of cottonoid patty to hold the patulous diaphragm away from my operative corridor while I use the suction device and another blunt ring curette to remove tumor and work around the planes of these folds. The use of the 30-degree endoscope is necessary to move the head of the endoscope out of the working space of these instruments since the presence of these four instruments can easily lead to the “swording” effect.
Figure 8: The “four-hand” technique is shown. The ENT colleague places the endoscope and the retracting ring curette (over the cottonoid patty) in one nostril while the neurosurgeon places a suction device and ring curette in the other nares.
Figure 9: Following gross total resection of the tumor, the diaphragmatic folds are released and the diaphragm freely herniates through the resection cavity.
If the tumor erodes through the diaphragm and into the third ventricle, the diaphragmatic defect can be expanded sharply, allowing for more radical tumor resection. Any tumor that involves the third ventricle or surrounds the optic apparatus should be dissected under direct visualization.
Closure
The diaphragmatic defect is usually not large and repairable with fat globules. However, large defects that expose the suprasellar contents require the “gasket-seal” technique and a nasoseptal flap for their reconstruction.
I pay special attention to place and buttress the fat globules (wrapped in Surgicel) in the area where the diaphragmatic tear is present. Aggressive indiscriminate filling of the sella with fat is not advised and may lead to optic apparatus compression. As the diaphragm in giant tumors is quite patulous, the exact point of the leak should be recognized before the fat globules are placed. Medpor (Porex, Newnan, GA) is helpful to create a solid barrier at the sellar floor and keep the fat in place.
A dura sealant product is then used to seal the nasoseptal flap into place.
OTHER CONSIDERATIONS
Paramedian Transsphenoidal Approach
This approach is useful for Knosp Grade 1-3 tumors. The approach and closure are essentially similar to those for classic or traditional pituitary adenomas. The extended endoscopic transtuberculum and transplanum routes facilitate exposure and resection of tumors extending into the suprasellar cisterns.
Coagulation and transection of the superior intercavernous sinus is important to expose tumors extending into the anterior suprasellar cisterns. Tumor resection begins with resection of the intrasellar portion of the mass. The diaphragmatic defect caused by the tumor is then expanded via sharp dissection under direct vision to reach the suprasellar mass and dissect it from the optic chiasm and the anterior cerebral arteries.
The carotid arteries are mapped appropriately using a microDoppler device during the approach and intermittently during tumor resection. Neuronavigation provides another source of frequent feedback during tumor manipulation. Venous bleeding can usually be readily controlled with FloSeal (Baxter, Deerfield, IL) packing followed by gentle tamponade using a small piece of cottonoid patty.
The carotid arteries should not be aggressively manipulated to minimize their risk of vascular dissection.
Transpterygoid Approach
This extended endoscopic approach is useful in resection of adenomas involving the lateral or anteroinferior compartments of the cavernous sinus (Knosp Grade 4). A complete sphinoethmoidectomy is necessary for adequate exposure. Pre- and intraoperative identification of pneumatized lateral sphenoid recesses are paramount to avoid surprise postoperative cerebrospinal fluid leaks.
Careful bone removal between the opticocarotid recess, the paraclival carotid artery medially and the orbital apex laterally is required to expose the anterior and lateral cavernous sinus compartments. The Vidian canal at the base of the sphenoid sinus is a useful landmark that identifies the transition from the petrous to the paraclival segments of the carotid artery.
Tumor resection is achieved in the same way as the midline transsphenoidal approach, except that when the tumor is confined to the lateral part of the cavernous sinus, a separate dural opening lateral to the carotid artery is often needed. As stated before, the dural incision lateral to the carotid artery is guided by microDoppler mapping. Careful piecemeal tumor resection avoids injury of the carotid artery and abducens nerve, both within the cavernous sinus.
The trigeminal nerve and oculomotor nerves are encased in the lateral wall of the venous sinus and are therefore relatively protected if not encased or displaced by the tumor. Intraoperative monopolar stimulation (~2 mA) can identify the abducens and oculomotor nerves during resection. The sympathetic nerves encasing the cavernous carotid artery and intracavernous ligaments should not be mistaken for the abducens nerve. Stimulation mapping differentiates these nerves and other trabecular septations/ligaments that can mimic the appearance of the nerves.
Reconstruction typically demands a nasoseptal flap.
The transcranial approach to intracavernous tumors involves the use of modified Dolenc skull base approaches. Please see the Trigeminal Schwannoma chapter for more details. Briefly, the combined intradural/extradural transcavernous approach involves a pterional craniotomy and extradural anterior clinoidectomy, partial orbitotomy, optic canal decompression, and intradural entry into the cavernous sinus via the space between V1 and V2.
Other Personal Reflections
Intradural pituitary transposition is unnecessary and should be avoided. This form of transposition leads to venous sacrifice of the gland; this sacrifice is not tolerated and usually leads to panhypopituitarism.
A conservative resection strategy is recommended for tumors located lateral to the carotid artery. Adjuvant radiation therapy may be warranted for residual tumors that show interval growth on serial scans.
There are specific instances when the extended endonasal endoscopic approach may be inferior to the traditional transcranial approaches. These include but are not limited to the following:
- active sinonasal infections in an acutely decompensating patient,
- dolichoectatic carotid arteries (“kissing” carotids), making removal through the transsphenoidal approach cumbersome or unsafe,
- fibrous and highly vascular tumors that have failed prior endonasal resection attempts, and
- large suprasellar tumors that reside above an atrophic sella.
Postoperative Considerations
Please refer to the chapter on Pituitary Adenoma: Diagnosis and Operative Considerations.
Pearls and Pitfalls
- The goals of surgery, which should be carefully planned preoperatively, partly dictate the extent of tumor resection within the cavernous sinus.
- Conservative resection of tumors within the lateral part of the cavernous sinus is recommended.
- Given the panoramic visualization and resectability capabilities provided by the extended endoscopic approaches, there is limited role for transcranial approaches during surgery for giant pituitary adenomas.
Contributor: Wael Hassaneen, MD and Jonathan Weyhenmeyer, MD
References
Ceylan S, Koc K, Anik I. Endoscopic endonasal transphenoidal approach for pituitary adenomas invading the cavernous sinus. J Neurosurg. 2010; 112: 99-107.
Funaki T, Matsushima T, Celda-Peris M, Valentine RJ, Joo W, Rhoton AL. Focal transnasal approach to the upper, middle, and lower clivus. Neurosurgery. 2013; 73 (2 Suppl Operative): ONS 155-191.
Hardy J, Vezina JL. Transsphenoidal neurosurgery of intracranial neoplasm. Adv Neurol. 1976;15:261-273
Hofstetter CP, Moshel Y, Nanaszko M, Anand VK, Schwartz TH. Extended endonasal, endoscopic transphenoidal approach versus craniotomy for giant pituitary macroadenomas (chapter 24), in Schwartz TH and Anand VK (eds): Endoscopic Pituitary Surgery. Endocrine, Neuro-opthalmologic, and Surgical Management. American Association of Neurological Surgeons and Thieme, 2012, pp 248-261.
Jane JA, Thapar K, Kaptain GJ, Maartens N, Laws ER. Pituitary surgery: transsphenoidal approach. J Neurosurg. 2002; 51: 435-444.
Jho DH, Jho DH, Jho HD. Endoscopic endonasal pituitary and skull base surgery (chapter 22), in Quiñones-Hinojosa A (ed): Schmidek & Sweet Operative Neurosurgical Techniques. Philadelphia: Elsevier, 2012, pp 257-279.
Koutourousiou M, Gardner PA, Fernandez-Miranda J, Paluzzi A, Wang E, Snyderman CH. Endoscopic endonasal surgery for giant pituitary adenomas: advantages and limitations. J Neurosurg. 2013; 118: 621-631.
Mohr G, Hardy J, Comtois R, Beauregard H. Surgical management of giant pituitary adenomas. Can J Neurol Sci. 1990; 17:62-66.
Pasquini E, Frank G. Endoscopic pituitary surgery in the cavernous sinus. Endoscopic pituitary surgery (chapter 21), in Schwartz TH and Anand VK (eds): Endocrine, Neuro-opthalmologic, and Surgical Management. American Association of Neurological Surgeons and Thieme, 2012, pp 212-226.
Prevedello DM, Solari D, Carrau RL, Gardner P, Kassam, AB. Endoscopic endonasal approach for cranopharyngiomas (chapter 25), in Quiñones-Hinojosa A (ed): Schmidek & Sweet Operative Neurosurgical Techniques. Philadelphia: Elsevier 2012, pp 303-310.
Wooodworth G, Patel K, Shin B, Burkhardt J, Tsiours AJ, McCoul ED, Anand VK, Schwartz TH. Surgical outcomes using a medial- to- lateral endonasal endoscopic approach to pituitary adenomas invading the cavernous sinus. J Neurosurg. 2014; 120: 1086-1094.
Please login to post a comment.