Posterior Inferior Cerebellar Artery Aneurysm
This is a preview. Check to see if you have access to the full video. Check access
Clip Ligation of a Posterior Inferior Cerebellar Artery (PICA) Aneurysm
This is a preview. Check to see if you have access to the full video. Check access
Challenging Atherosclerotic PICA Aneurysm
Like all other cerebral aneurysms, posterior inferior cerebellar (PICA) aneurysms are most frequently diagnosed either after their rupture or incidentally via imaging for an unrelated symptom such as headaches. After basilar apex aneurysms, PICA aneurysms are the most common posterior circulation aneurysm subtype.
Upon its rupture, the proximity of the aneurysm to the medulla oblongata is likely to lead to a loss of consciousness, as well as respiratory and cardiac arrest. Large aneurysms can rarely present with symptoms and signs of brainstem and lower cranial nerve dysfunction. Embolic phenomenon from thrombotic aneurysms can lead to lateral medullary (Wallenberg) syndrome.
Indications for Microsurgery
Although natural history studies suggest a very low rupture risk for lesions under 7 mm, the majority of aneurysms that present with hemorrhage are indeed under 7 mm in size; this phenomenon presents a conundrum for the neurosurgeon. These studies have not targeted posterior circulation aneurysms adequately, and therefore the true natural history, including the hemorrhagic risk of PICA aneurysms, is unknown. Nonetheless, most clinicians apply the natural history data from anterior circulation aneurysms to those of the posterior circulation.
Young age of the patient and irregular morphology of the sac all portend a higher rupture risk, and these factors should prompt treatment of aneurysms that are even as small as 5 mm.
The clipping-versus-coiling debate continues to haunt neurosurgeons. The tradeoffs between minimally invasive coil embolization versus the more durable clip ligation continue to complicate decision making in aneurysm surgery. The small caliber of the PICA and the broad neck of the associated aneurysms place the PICA at some risk during coil embolization. Therefore, microsurgery remains a viable option for select patients.
Patients with PICA aneurysms who are older, who have medical morbidities, and who harbor narrow-neck aneurysms should undergo endovascular management; whereas young patients and those with wide-neck aneurysms should be considered for microsurgical clipping. As always, the microsurgical experience of the treating clinician plays a central role in the offered choice of therapy.
Evaluation
Spontaneous fourth ventricular hemorrhage in the absence or presence of subarachnoid hemorrhage (SAH) requires a vascular study to rule out a PICA aneurysm. The occurrence of radiographic hydrocephalus after such an aneurysm rupture reaches 95%.
The morphology of the vertebral artery (VA) should be assessed, and a hypoplastic VA ending in PICA should be noted because this vascular variation is likely to affect the tolerance of distal neural territories to temporary or permanent VA occlusion. Reduplicated PICA and dominant anterior inferior cerebellar arteries (AICA’s) supplying the PICA territory are also important factors in this tolerance. In addition, the size of the posterior communicating arteries can determine if proximal VA occlusion is safe.
Proximal fusiform aneurysms involving the perforating arteries may require revascularization, but distal ones can be treated with Hunterian ligation.
Catheter angiography provides superior imaging of proximal PICA perforating arteries and the robustness of collateral flow. In addition, it establishes the diagnosis of dissection that is not uncommon in this vascular territory.
A CT angiogram is effective for demonstrating the relevant composition of the vasculature in relation to the corresponding posterior fossa bony anatomy, including the foramen magnum and clivus. Midline aneurysms related to ectatic posterior circulation can be very challenging to reach microsurgically and endovascular options should be explored.
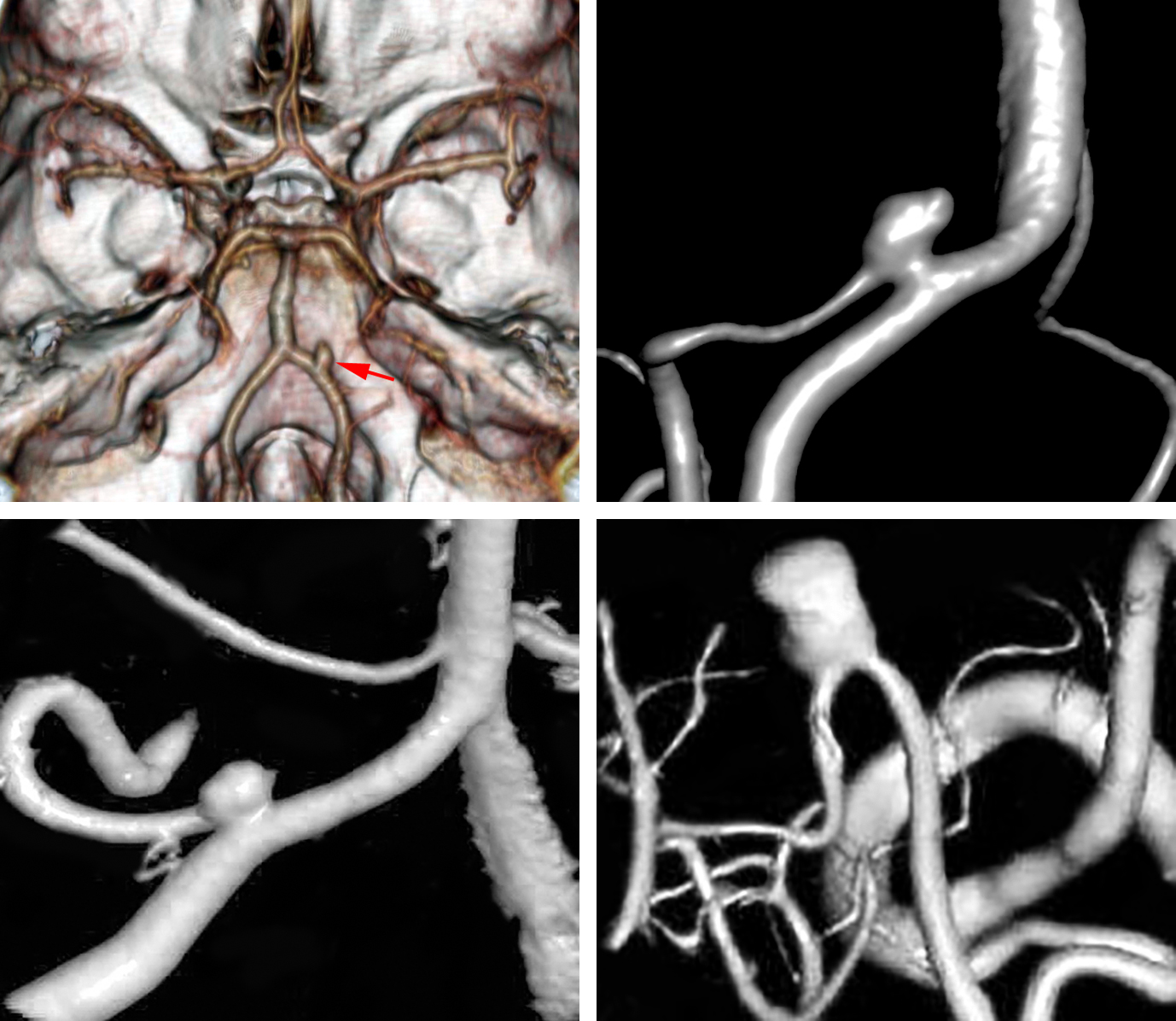
Figure 1: A medially located PICA aneurysm is demonstrated (upper images). Another more classic proximal (left lower image) and more distal AChA (right lower image) aneurysms are also included. Note the typical finding of the PICA’s origin incorporated into the aneurysm neck.
Preoperative Considerations
The clipability versus coilability of the aneurysm should be discussed with other microsurgeons and interventionalists in a multidisciplinary conference. Presence of calcification anywhere in the aneurysm excludes its suitability for primary clip ligation because the small caliber of the PICA is highly likely to be compromised via closure of the clip blades.
Dissecting aneurysms that primarily incorporate the VA proximal or distal to the origin of the PICA are straightforward to manage via proximal VA occlusion. However, those incorporating the origin of PICA require microsurgical intervention and revascularization, most likely through PICA-PICA side-to-side anastomosis.
Operative Anatomy
The vertebral artery originates as the first branch of the subclavian artery and enters the transverse foramen of the sixth cervical vertebral body. At C-3, the artery turns laterally and enters the foramen of C-2. After exiting through the foramen, it curves behind the atlantooccipital joint to lie horizontally along the posterior arch of C-1.
As the vertebral artery courses medially, it curves rostrally and passes through the foramen magnum. Along the transverse segment of the vertebral artery, there are usually muscular branches that anastomose with branches of the external carotid artery. Bleeding from these branches should not be confused with bleeding from the VA itself.
The posterior meningeal branch often originates from the middle portion of this VA segment. After the VA penetrates the dura, it courses laterally and then ventrally to join the contralateral VA to form the basilar artery. In approximately two-thirds of patients, this union occurs at or just below the inferior pontine sulcus. In approximately 15%, one VA is dominant, and in 5-10%, a nondominant VA ends at the PICA and does not join the contralateral VA (hypoplastic VA).
Branches of the vertebral artery include the PICA, direct perforating branches to the medulla, the anterior spinal artery, small meningeal branches, and, occasionally a posterior spinal artery. The site of the origin of the PICA arising from the VA varies from below the foramen magnum to the level of the vertebrobasilar junction.
The PICA has the most complex relationship to the cranial nerves (CNs) of any artery. The VA courses anterior to the glossopharyngeal, vagus, accessory, and hypoglossal nerves. The proximal part of the PICA passes around or between these nerves and often stretches or distorts the rootlets of these and adjacent nerves.
The inferior olive protrudes from the anterolateral surface of the medulla near the VA and the origin of the PICA. The hypoglossal nerve joins the brainstem on the anterior border of the olive while the glossopharyngeal, vagus, and accessory nerves arise along the posterior border of olive. Most PICAs arise at the level of or lateral to the olive.
Figure 2: Operative anatomy of the lower cerebellomedullary cisterns is demonstrated. Partial condylectomy was performed in this specimen; this maneuver is unnecessary for almost all PICA aneurysms. The red arrow points to the origin of the PICA on the VA. Note the intimate relationship of these vessels to the lower cranial nerves (image courtesy of AL Rhoton, Jr.)
The PICA is divided into five segments, and four are in the surgeon’s view as seen from the transcondylar approach: 1) anterior medullary, 2) lateral medullary, 3) tonsillomedullary, 4) telovelotonsillar, and 5) cortical.
The anterior medullary segment courses from the PICA origin to the level of CN XII and then becomes the lateral medullary segment. After this, it crosses the entry points of CNs IX-XI at the brainstem and loops inferiorly before turning 180 degrees dorsally to course between the cerebellar tonsil and the medulla.
When the PICA crosses CNs IX-XI, it becomes the tonsillomedullary segment, and when it reaches the midpoint of the tonsil along its ascent next to the medulla, it transitions to the telovelotonsillar segment. The artery continues superiorly, running on the inferior medullary velum, and then makes another 180-degree loop and courses caudally again before exiting the tonsillobiventral fissure to travel along the surface of the cerebellum. Once it reaches the surface of the cerebellum, it transitions to its cortical segment.
Click here to view the interactive module and related content for this image.
Figure 3: The morphology of the right intradural (left image) and left extradural (right image) PICA from a posterior view is depicted in these photos. The first three major PICA segments, namely the anterior medullary, lateral medullary and tonsillomedullary segments, also provide arterial supply to the brainstem. Any segment of the PICA in close proximity of the brainstem can provide vascular support to the brainstem and should be preserved (images courtesy of AL Rhoton, Jr).
Unfortunately, the vast anatomical variations with respect to the origin of PICA and morphology of VA preclude any reliable preoperative planning until the lower CNs are exposed in surgery and their routes identified.
MICROSURGICAL CLIP LIGATION OF POSTERIOR INFERIOR CEREBELLAR ARTERY ANEURYSMS
I expose proximal PICA aneurysms via a conservative transcondylar approach with minimal or most often no drilling of the condyle. In essence, this is a lateral suboccipital craniotomy to the level of the condyle. This approach does not risk destabilizing the occipitocervical junction and provides flexible operative working angles to deploy the clip.
Distal PICA aneurysms are exposed via a midline suboccipital craniotomy.
The patient is positioned in the park-bench position. The goal is to position the head in order to create the most ergonomic working angle directly along the axis of the VA. I widen the space between the shoulder and the suboccipitus; the mastoid bone is the highest point in the operative field. Thus, the head is flexed until the chin is only two fingerbreadths away from the sternum and rotated 45 degrees toward the floor.
A hockey-stick shaped incision is made from the C3 to the inion, then curving laterally to the level of the mastoid bone where is curves slightly inferiorly again. A myofascial cuff is left along the nuchal line for approximation of the soft tissue flap during closure. The muscles are detached from the bone and mastoid region and retracted inferolaterally in a single myocutaneous layer.
The foramen magnum and posterior arch of the C1 is exposed to expand the inferior-to-superior operative trajectory. A generous craniectomy extends from the foramen magnum inferiorly to the sigmoid sinus and occipital condyle laterally; the transverse sinus is not unroofed.
If the occipital condyle protrudes conspicuously out directly into the operative field, it will limit intradural access to some of the more medially-located PICA aneurysms. In these situations, every millimeter of condylectomy aids dramatically in the exposure, analogous to the sphenoid ridge osteotomy during the pterional approach.
It is important to recognize that drilling of more than one-third of the condyle is a possible risk for long-term instability of the craniocervical junction. The limit of the one-third condylectomy is the condylar emissary vein. Most PICA aneurysms are quite proximal on the intracranial VA, just above the foramen magnum. Thus the extra effort at widening the operative corridor at the foramen magnum results in substantially improved surgical access.
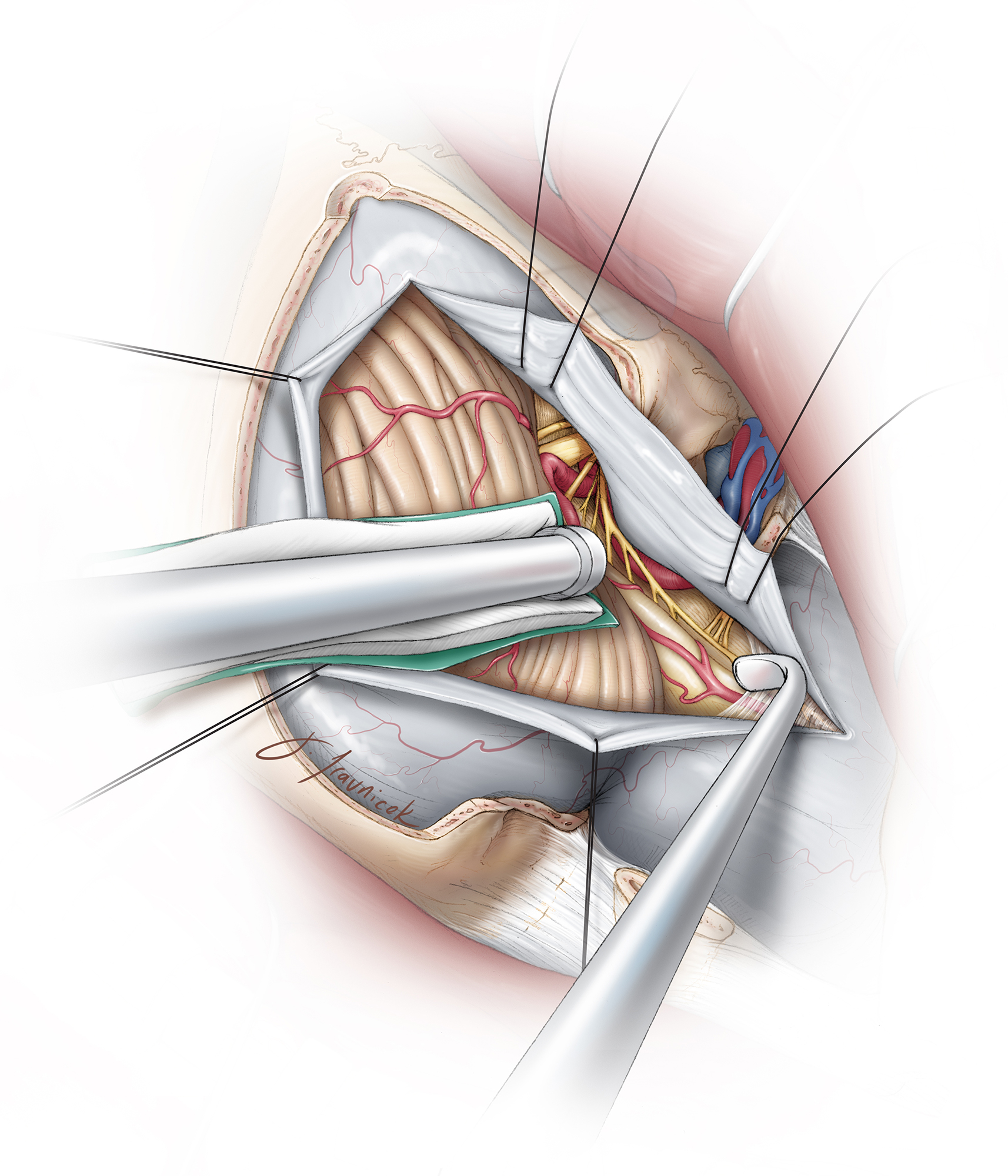
Figure 5: Musculocutaneous dissection for a right-sided lateral suboccipital craniotomy is illustrated (upper images). Condylectomy is not necessary for most PICA aneurysms; however, bone resection should at least extend to the level of the condyle (left lower image). The extent of bone resection in relation to the extradural vertebral artery is shown (right lower image).
INTRADURAL PROCEDURE
Initial Exposure
Meticulous proximal-to-distal dissection along the intradural course of VA is warranted. The anatomy of the lower cranial nerves in relation to the aneurysm is crucial in affecting the technical difficulties of clip ligation.
Figure 6: The dura is opened in a curvilinear fashion, with the flap pulled laterally via retraction sutures along the deeper, more medial aspects of the dura to maximize the operative corridor toward the lateral brainstem. The VA is recognized early and the arachnoid membranes over this artery are opened to release cerebrospinal fluid (CSF). A demagnified view of the operative field is illustrated. Note the direction of the retraction vector on the lateral cerebellum.
Microdissection to Secure Proximal Control
The first step is to gain proximal control of the VA as it courses under the dentate ligament. The dentate ligament can be cut to improve exposure where it tethers the cervical cord to the lateral dura. Its distinguishable white color identifies it from the accessory nerve. The ligament ends at the lateral foramen magnum dura as opposed to the nerve that continues superiorly to enter the jugular foramen.
A section of the VA that is free of spinal perforators is prepared for proximal control.
Figure 7: A high-magnification view of the pontomedullary cistern and its contents are shown. Note the typical close anatomic relationship between the PICA and CN XII. A generous inferior-to-superior operative trajectory is necessary to avoid injury to the lower cranial nerves. The location of the PICA’s origin is highly variable along the VA. Overall, this neurovascular anatomy is highly inconsistent; ruptured aneurysms fill the corresponding cisterns with blood and complicate dissection. The best strategy is to follow the course of VA and identify the nerves early.
Aneurysm Dissection
Following exposure of the intradural VA to the level of the lower cranial nerves, the tonsil is gently elevated supramedially, exposing the tonsillomedullary segment of the PICA. Next, I trace the artery proximally to its origin off the VA; this is where the aneurysm is found.
Likewise, the VA is traced distally to the PICA’s origin and aneurysm neck. The final pathway, whether it is along the VA or the PICA, may involve dissection of the lower CNs. The triangle bordered by CNs X-XI and the brainstem is the corridor through which the aneurysm is tackled.
The arachnoid veil that encompasses CN IX-XI is incised sharply; CN XII usually becomes visible coursing near the PICA origin. The accessory nerve serves as a constant landmark in the middle of the field to orient the surgeon. If necessary, the arachnoid layers surrounding all of the CNs should be dissected to expand the exposure. I attempt to avoid working between the nerve fibers to prevent their injury.
This dissection will expose the origin of CN XII at the brainstem deep to CNs IX-X. The lower CNs are gently mobilized using dynamic retraction, most often superiorly or occasionally inferiorly, to expose the aneurysm neck. Once the base of the aneurysm is exposed, the distal VA, turning medially, anteriorly and away from the instruments, must be visualized to ensure its safety during permanent clip application.
Figure 8: The distal aspect of VA may be obscured by the aneurysm. A combined gentle lateral mobilization of the aneurysm neck (using a fine dissector) and medial displacement of the brainstem (using a fine-tipped suction) barely identifies the distal VA (inset image). Dissection of the VA should be carried out from proximal to distal along the medial aspect of the VA, beyond the aneurysm, to give the surgeon a sense of the course of the VA distal to the aneurysm. One can occasionally trace the lateral aspect of the VA distally beyond the aneurysm to define the distal VA. Temporary proximal occlusion of the VA is highly beneficial during these high-risk maneuvers.
Most PICA aneurysms point superiorly. The dissection around the neck of the aneurysm can be quite challenging because of the small working space and often very broad base of the aneurysm involving the small-caliber PICA. These obstacles set the stage for the use of fenestrated clips to show their worth.
Clip Ligation
Most small PICA aneurysms are handled via a single fenestrated clip encircling the PICA. Large aneurysms demand a tandem clipping technique using a fenestrated clip to close the distal neck and protect the PICA while a single straight clip collapses the proximal neck. Adherent cranial nerves may also be included in the fenestration. A fenestrated clip frequently obviates the need to separate a tightly adherent distal aneurysm wall from the VA adventitia.
Due to the often less than ideal anatomy and morphologic relationship of the aneurysm dome to the PICA, VA and lower cranial nerves, I rarely need to compromise and plan alternative techniques such as definitive clip occlusion of the proximal vertebral artery. This maneuver is safe as long as the PICA itself remains patent and is supplied in a retrograde fashion via the contralateral VA. A robust, preferably dominant contralateral VA and competent vertebrobasilar junction should be confirmed through careful study of the preoperative angiographic images.
If the rare medially situated aneurysm is inaccessible through the CNs or these nerves seriously obstruct the operative angles, the microsurgical procedure should be aborted and endovascular opportunities explored. Persistent manipulation of these nerves leads to high morbidity associated with their dysfunction.
Figure 9: Clip deployment via dynamic mobilization of the lower cranial nerves is illustrated. The obvious blind spot is the distal VA; its patency can be evaluated only after clip application and gentle rotation of the clip. Note the use of a fenestrated clip to preserve flow in the PICA (upper image). A small neck remnant may be necessary to avoid stenosis at the proximal section of the PICA (lower image) because the PICA often originates from the neck of the aneurysm.
Figure 10: Once the clip is applied, careful inspection of the blades is required to ensure effective neck occlusion and patent arteries. The CN XII may be incorporated within the fenestration, if necessary.
Figure 11: PICA aneurysms may be clip ligated via straight clips based on the configuration of the local anatomy. The temporary clip is placed on the proximal VA (upper image) and the location of the distal VA is marked with the red arrow (lower image).
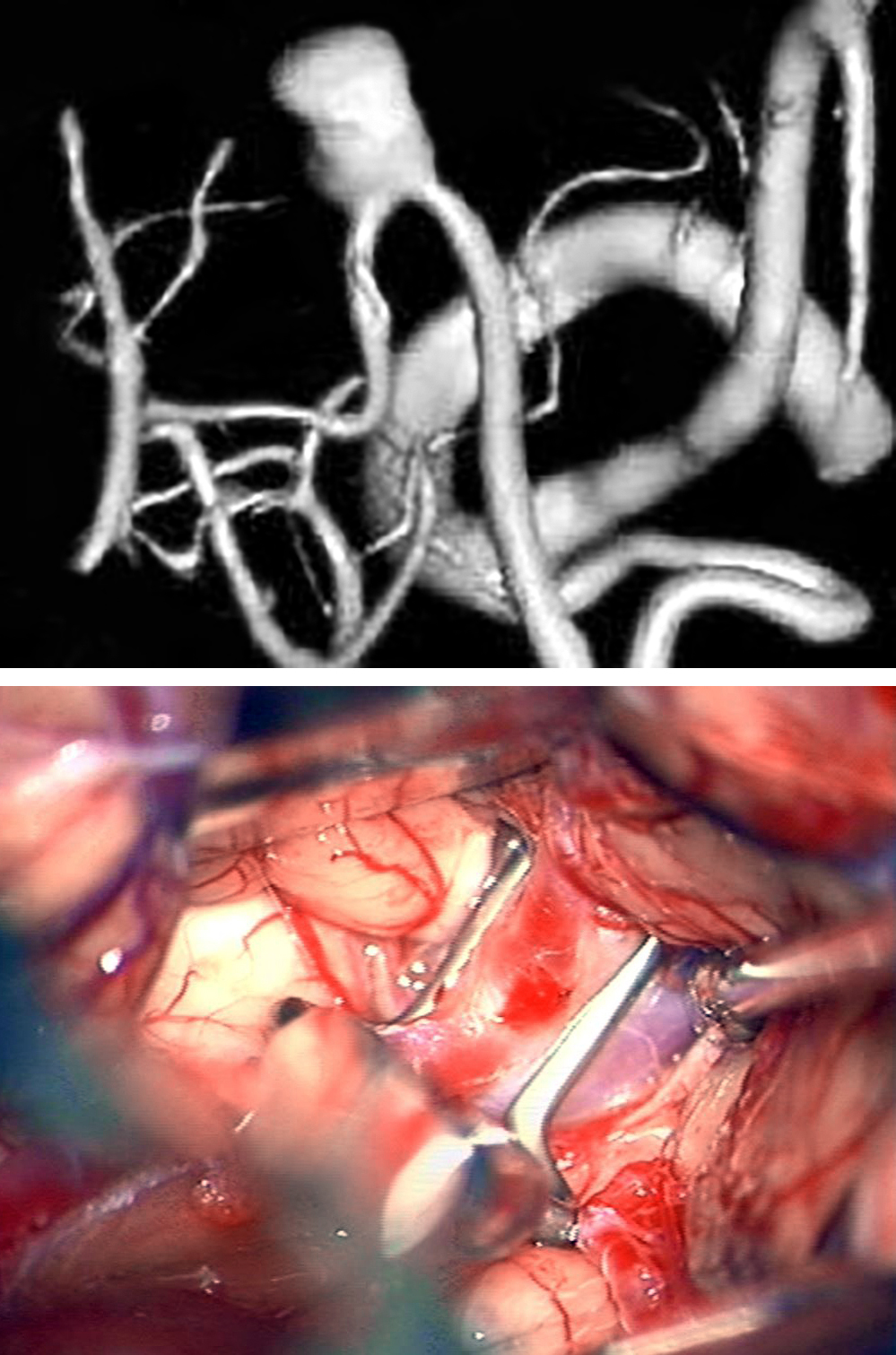
Figure 12: This right-sided PICA aneurysm (upper image) was clipped using an angled clip. Both proximal and distal temporary clipping (middle photo) was required because of the suspicion of a pseudoaneurysm. The final clip construct is demonstrated (lower photo).
Challenging PICA Aneurysm
Figure: 13: A more classic PICA aneurysm (upper angiogram) was clip excluded using an angled fenestrated clip. The distal VA is marked with a red arrow and the aneurysm is marked with * (middle image). The anatomic relationship of CN XII is demonstrated. The final clip construct and the location of the clip blade (arrow) are also shown (lower image).
Figure 14: A distal PICA aneurysm with a fusiform neck (upper image) along the floor of the fourth ventricle was clipped using an angled fenestrated clip (lower image) via the telovelar approach.
Fusiform Distal PICA Aneurysm
Revascularization
Bypass techniques can be considered for calcified or thrombotic aneurysms. One ideal donor vessel is the tonsillomedullary segment of the contralateral PICA that often travels in close proximity to the corresponding segment of the ipsilateral PICA. A side-to-side anastomosis is effective and relatively easy to conduct. Extracranial-to-intracranial bypass can also be accomplished using the occipital artery.
Distal PICA loops allow aneurysmal excision and end-to-end reanastomosis because of the availability of the extra length of the PICA loops. Other options include excision and reimplantation of the PICA onto the VA. Sole occlusion of the PICA just distal to the aneurysm and away from the perforating segments has also proven effective for causing aneurysmal thrombosis.
For selected giant lesions causing mass effect on the brainstem, deconstruction and flow reversal using a combination of surgical and endovascular techniques can be considered. A thoughtful plan should precede any intervention.
Postoperative Considerations
During the immediate postoperative recovery period, the patient should be monitored for potential airway obstruction or aspiration caused by injury to the lower cranial nerves. Large aneurysms require extensive manipulation of the lower cranial nerves and are associated with development of postoperative CN’s neuropraxia; appropriate measures should be taken, in particular, leaving the patient intubated until the patient’s level of consciousness allows otolaryngologic evaluation.
Pearls and Pitfalls
- Appropriate bony removal at the lateral aspect of the craniotomy and foramen magnum provides flexible intradural working angles. Although removal of the condyle is not necessary, bony resection should extend to the condyle.
- Manipulation of the lower cranial nerves is associated with morbidity and should be minimized. One should resort to definitive proximal VA occlusion or endovascular options if the lower cranial nerves are found to be at significant risk upon their exposure.
- Identification of the distal VA is imperative before clip application. This step should not be ignored because of its technical difficulty.
Contributors: Tarun Bhalla, MD, PhD, and Clemens M. Schirmer, MD, PhD
References
Lawton MT. Seven Aneurysms: Tenets and Techniques for Clipping. New York: Thieme Medical Publishers, 2011.
Samson DM (ed). Intracranial Aneurysm Surgery: Techniques. Mount Kisco, NY: Futura Publishing, 1990.
Please login to post a comment.