Epidermoid Cyst
Figure 1: (Top Left) A low-density lesion in the left cerebellopontine angle on CT could represent a number of lesions, including arachnoid cyst or epidermoid cyst. T2WI (top right) and T1WI postcontrast (middle left) give little additional diagnostic information, with the lesion still matching CSF signal. (Middle Right) FLAIR imaging, as in this case, often demonstrates an epidermoid cyst to have different signal than CSF. (Bottom) Diffusion-weighted imaging is the most helpful sequence with these lesions, demonstrating often dramatic hyperintensity.
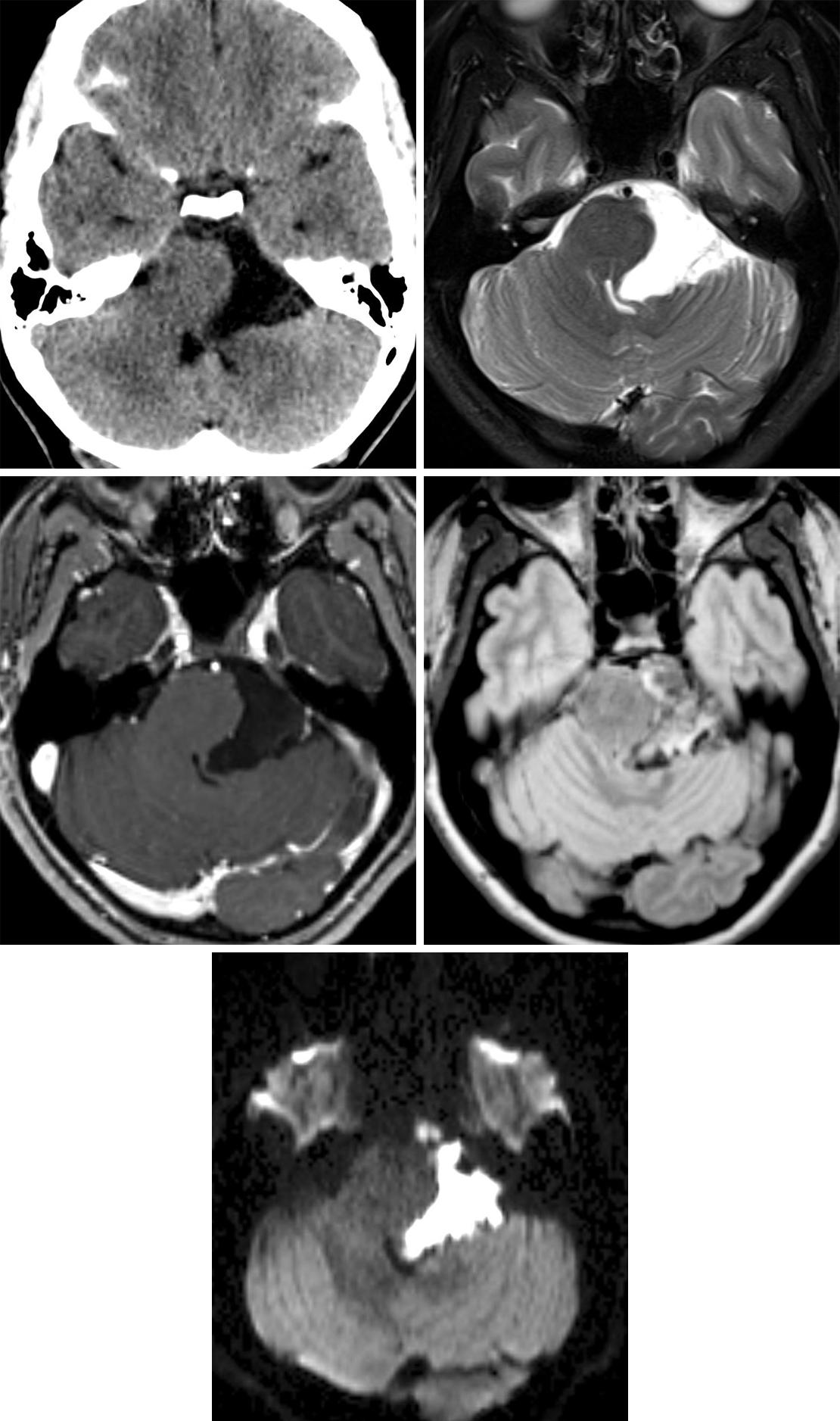
Figure 2: This large epidermoid cyst looks similar to CSF on T1-weighted (top left) and T2-weighted (top right) imaging, but its identity as a possible simple cyst should be questioned given the degree of heterogeneity that is often visible on FLAIR (middle left). Diffusion restriction visible as bright signal on DWI (middle right) and dark signal on ADC (bottom left) is the hallmark of epidermoid cysts and can greatly help to differentiate them from other simple cysts, such as arachnoid cysts. (Bottom Right) This epidermoid cyst has a small amount of nodular contrast enhancement in the periphery, a finding that is present only rarely.
BASIC DESCRIPTION
- Benign ectodermal inclusion cysts of congenital or acquired etiology
- Most common congenital intracranial tumor (~1%)
PATHOLOGY
- Congenital: arise from ectodermal epithelium in the third to fifth weeks of embryogenesis during the process of neural tube closure
- Sporadic
- May be seen in association with dermal sinus tracts or vertebral anomalies
- Rare acquired lesions are thought to have a post-traumatic etiology, often spinal in location when secondary to lumbar punctures
- Epidermoid cyst growth by desquamation and formation of cholesterol/keratin crystals
- Gross pathologic features include shiny or “pearly” appearance within an outer connective tissue wall
- Cyst contains solid cholesterol crystals and keratin
CLINICAL FEATURES
- Patient age of 20–60 years most common
- No gender predilection
- Presenting signs and symptoms depend on tumor size and location
- Headache, cranial neuropathies (cranial nerves V [trigeminal nerve], VII [facial nerve], and VIII [vestibulocochlear nerve] most common)
- Cyst rupture can cause chemical meningitis
- Often asymptomatic
- Malignant degeneration into squamous cell carcinoma is rare
- Treatment: microsurgical resection; gross-total resection is often difficult because of involvement of adjacent structures and specifically attachment of the tumor pearls to the cerebrovascular structures
- Prognosis: recurrence common with incomplete tumor resection or secondary to cerebrospinal spinal fluid (CSF) seeding; malignant degeneration into squamous cell carcinoma is rare
IMAGING
- General
- Most cases (90%) are intradural and located within the basal cisterns (cerebellopontine angle, fourth ventricle, parasellar)
- Minority of cases (10%) are extradural and may arise within the bony calvarium (diploic space) or spine
- Variable size, round or lobulated mass
- Slow but insinuating or invaginating pattern of growth, often encases or surrounds adjacent nerves and vasculature
- CT
- Well-defined, usually hypodense mass similar in density to CSF
- <5% appear hyperdense, often due to proteinaceous, iron-rich, or hemorrhagic contents
- Calcifications are common
- Typically do not enhance on contrast-enhanced CT
- MRI
- T1WI
- Signal intensity typically greater than that of CSF but less than that of brain parenchyma
- Highest signal often seen at the margin of the tumor
- Signal intensity greater than that of brain parenchyma indicates a “white epidermoid,” brighter because of its higher degree of fatty components or blood products
- Rare hypointense “black epidermoids” caused by low triglyceride and unsaturated fatty acid contents
- T2WI
- Isointense to hyperintense to CSF
- Rare hypointense signal due to iron content or Ca++
- FLAIR: intermediate to hyperintense due to incomplete dropout of fluid signal
- DWI: demonstrates often markedly increased signal (restricts) with corresponding ADC value near that of brain parenchyma (in contrast to an arachnoid cyst which will not restrict)
- T1WI+C: typically nonenhancing, although minimal enhancement at the margin of the tumor might be seen; significant enhancement might suggest malignant degeneration
- T1WI
IMAGING RECOMMENDATIONS
- MRI with FLAIR and DWI/ADC
For more information, please see the corresponding chapter in Radiopaedia.
Contributor: Rachel Seltman, MD
References
Gao PY, Osborn AG, Smirniotopoulos JG, et al. Radiologic-pathologic correlation. Epidermoid tumor of the cerebellopontine angle. AJNR Am J Neuroradiol 1992;13:865–872.
Mohanty A, Venkatrama SK, Rao BR, et al. Experience with cerebellopontine angle epidermoids. Neurosurgery 1997;40:24–30.
Osborn AG, Salzman KL, Jhaveri MD. Diagnostic Imaging (3rd ed). Elsevier, Philadelphia, PA; 2016.
Ren X, Lin S, Wang Z, et al. Clinical, radiological, and pathological features of 24 atypical intracranial epidermoid cysts. J Neurosurg 2012;116:611–621. doi.org/10.3171/2011.10.JNS111462.
Tampieri D, Melanson D, Ethier R. MR imaging of epidermoid cysts. AJNR Am J Neuroradiol 1989;10:351–356.
Velamati R, Hageman JR, Bartlett A. Meningitis secondary to ruptured epidermoid cyst: case-based review. Pediatr Ann 2013;42:248–251. doi.org/10.3928/00904481-20130522-12.
Vellutini EA, Fernandes de Oliveira M, Ribeiro APC, et al. Malignant transformation of intracranial epidermoid cyst. Br J Neurosurg 2014;28:507–509. doi.org/10.3109/02688697.2013.869552.
Please login to post a comment.