Sensorimotor Mapping for Glioma
This is a preview. Check to see if you have access to the full video. Check access
Central Lobule Glioma: Principles of Mapping to Maximize Safe Resection
The goal of tumor surgery is to maximize tumor resection while avoiding neurologic deficit. Effective maximal resection leads to seizure control, improvement of symptoms caused by mass effect, a decreased risk of sampling error, and in patients with low-grade gliomas, a decreased risk of malignant transformation. The extent of resection also is associated with time to tumor progression and overall survival.
Because the greatest risk of tumor recurrence occurs within 2 cm of the contrast-enhancing region or tumor borders, the ideal resection strategy should preferably extend slightly beyond these borders. However, the loss of survival advantage is lost when a significant postoperative neurologic deficit such as hemiparesis is incurred. Therefore, the safety of glioma surgery near the perirolandic region is crucial for its consideration in the care of the patient.
The presence of functional cortices and white matter tracts of the central lobule (sensorimotor cortices) often limits the extent of resection. Cortical stimulation is used to circumnavigate the eloquent brain. Using this method, a very focal region of the sensory or motor cortex is depolarized, resulting in uncontrolled motor responses or paresthesias.
Cortical stimulation mapping can be conducted in two ways: Under anesthesia (sleep mapping) or under conscious sedation (awake mapping). Undoubtedly, sleep mapping is more comfortable for the patient and should be performed if it will provide necessary and reliable information for a safe resection.
Indications for the Procedure
Sensorimotor mapping is typically used for resection of intra-axial lesions and, most frequently, gliomas near or partially infiltrating the sensorimotor cortices and corona radiata. I do not use this method for cavernous malformations or metastasis unless mapping information can guide the exact location of the initial corticotomy within the normal cortex to reach the deep lesion. Infiltrating tumors associated with the supplementary motor area and internal capsule are also suitable candidates for mapping.
I use mapping (awake or sleep) primarily for low-grade gliomas affecting the central lobule. The use of this technique for resection of high-grade gliomas (HGGs) directly infiltrating the functional cortices and tracts often leads to neurologic morbidity, despite preservation of these functional areas. Subtotal resection of these HGGs is also associated with postoperative neurological decline and risk of hematoma formation. However, I do use mapping for specific HGGs that do not directly infiltrate the functional areas, but are adjacent to them. This strategy allows mapping for safe resection in nonfunctional peritumoral regions in expectation of radical tumor removal.
More specifically, I prefer to use sleep mapping if the tumor does not directly infiltrate the central lobe and its associated white matter tracts but is anatomically within millimeters of these vital structures. Instead, I use awake mapping for tumors that directly infiltrate these structures as shown on preoperative anatomical magnetic resonance (MR) or functional MR (fMR) imaging. Patients with tumors that infiltrate the postcentral gyrus undergo awake mapping because stimulation of this gyrus leads to subjective paresthesias that are not detectable in an anesthetized patient.
For details of awake mapping, please refer to the chapter on Language Mapping for Glioma. Awake mapping provides the most reliable mapping method (compared with sleep mapping) with minimal interference from the anesthesia. This is the reason for my preference to map the functional cortex while the patient is awake for low-grade gliomas that infiltrate directly into the central lobule. In addition, the direct feedback of an awake patient and continuous intraoperative examinations are the most reliable monitoring tools that encourage the surgeon to be more aggressive during tumor resection.
Preoperative Considerations
In most cases, motor mapping does not require the patient to be awake, therefore patient cooperation is less critical than the one required for awake mapping.
Preoperative evaluation of sensorimotor function is important. Significant hemiparesis hinders cortical and subcortical mapping; the patient should at least have antigravity movement in the corresponding extremities preoperatively. Also, children under the age of 6 may have decreased cortical excitability. Somatosensory evoked potentials (SSEPs) should be used instead to identify the central sulcus when motor cortex excitation is not feasible.
Preoperative imaging determines the need for motor mapping. The sensorimotor cortices can be anatomically localized using preoperative MRI. This radiographic localization is often more reliable for central lobule than the speech cortices. Long-standing lesions such as cortical dysplasias, arteriovenous malformations, and gangliogliomas can displace function.
Figure 1: The radiographic landmarks for the central sulcus are demonstrated. The second, more posterior vertical sulcus, from the end of the horizontal superior frontal sulcus (green arrows) is the central sulcus (red arrow) (left image). A more reliable method is as follows: I trace the cingulate sulcus (green arrows) on midsagittal MRI images posteriorly, then superiorly (marginal sulcus) to its end. The marginal sulcus is just posterior to the rolandic cortex (central lobule) bounded by the red arrows, right image.
Functional imaging is increasingly used for mapping the sensorimotor cortices. This method is relatively reliable for localizing the central lobule and can determine the need for awake versus sleep mapping based on the degree of functional cortex infiltration by the tumor. Functional MRI is more reliable for identifying sensorimotor than for localizing language function. It is a valuable complementary tool, but cortical stimulation is the gold standard for mapping function and securing a safe resection.
Figure 2: The location of this tumor just anterior to the motor cortex required motor mapping to allow its maximal safe removal. The blue arrow marks the superior frontal sulcus and the red arrow marks the central sulcus (left image). Functional imaging (fMRI) located the tumor just anterior and medial to the central lobule (middle image). Postoperative MRI demonstrates gross total resection of the mass (right image). This patient suffered from temporary foot weakness that completely resolved in 4 weeks. Development of any permanent neurologic deficit can blunt or eliminate any survival advantage gained by resection. Because of direct infiltration of the tumor into the motor cortex, awake mapping with periodic intraoperative exams were deemed necessary to ensure and justify aggressive tumor resection.
Operative Anatomy
An indepth understanding of the cortical anatomy in relation to the surface landmarks is beneficial for pre- and intraoperative planning.
Click here to view the interactive module and related content for this image.
Figure 3: Relationship of the cranial sutures to the cortical surface. The central sulcus is usually 3.5 to 4.5 cm behind the coronal suture. The lower portion of the precentral gyrus is located just posterior to the pars opercularis, and the similar portion of the postcentral gyrus is immediately anterior to the supramarginal gyrus. There is a gyral ridge (yellow arrow, middle image) connecting the precentral and postcentral gyri so that the central sulcus never directly joins the Sylvian fissure. Another yellow arrow is placed along the midline at the 50% nasion-inion line, and the red arrow shows the location of the central sulcus approximately 2 cm behind this 50% point (lower image) (images courtesy of AL Rhoton, Jr). These landmarks are important during planning of the craniotomy.
SLEEP MAPPING FOR RESECTION OF GLIOMAS ASSOCIATED WITH THE PARACENTRAL LOBULE
The central lobule should be identified on preoperative imaging to determine the degree of its involvement with the tumor and the need for sleep versus awake mapping.
Neuroanesthesia is imperative for success of any mapping procedure. For details of anesthesia for awake mapping, please refer to the chapter on Language Mapping for Glioma.
The anesthesia for sleep mapping requires avoidance of paralytic medications. Endotracheal general anesthesia is composed of inhalation agents combined with midazolam (Versed) and fentanyl.
Craniotomy
For general details regarding exposure and craniotomy, please refer to other sections of this Atlas, including the Cranial Approaches volume.
Intraoperative navigation guides the extent of an adequate craniotomy. Although the supine patient positioning is adequate for lesions anterior to and within the central lobule, I consider using the lateral position if the lesion is situated just posterior to the lobule. Alternatively, the supine position can be employed with the ipsilateral shoulder highly elevated on a bulky gelrest.
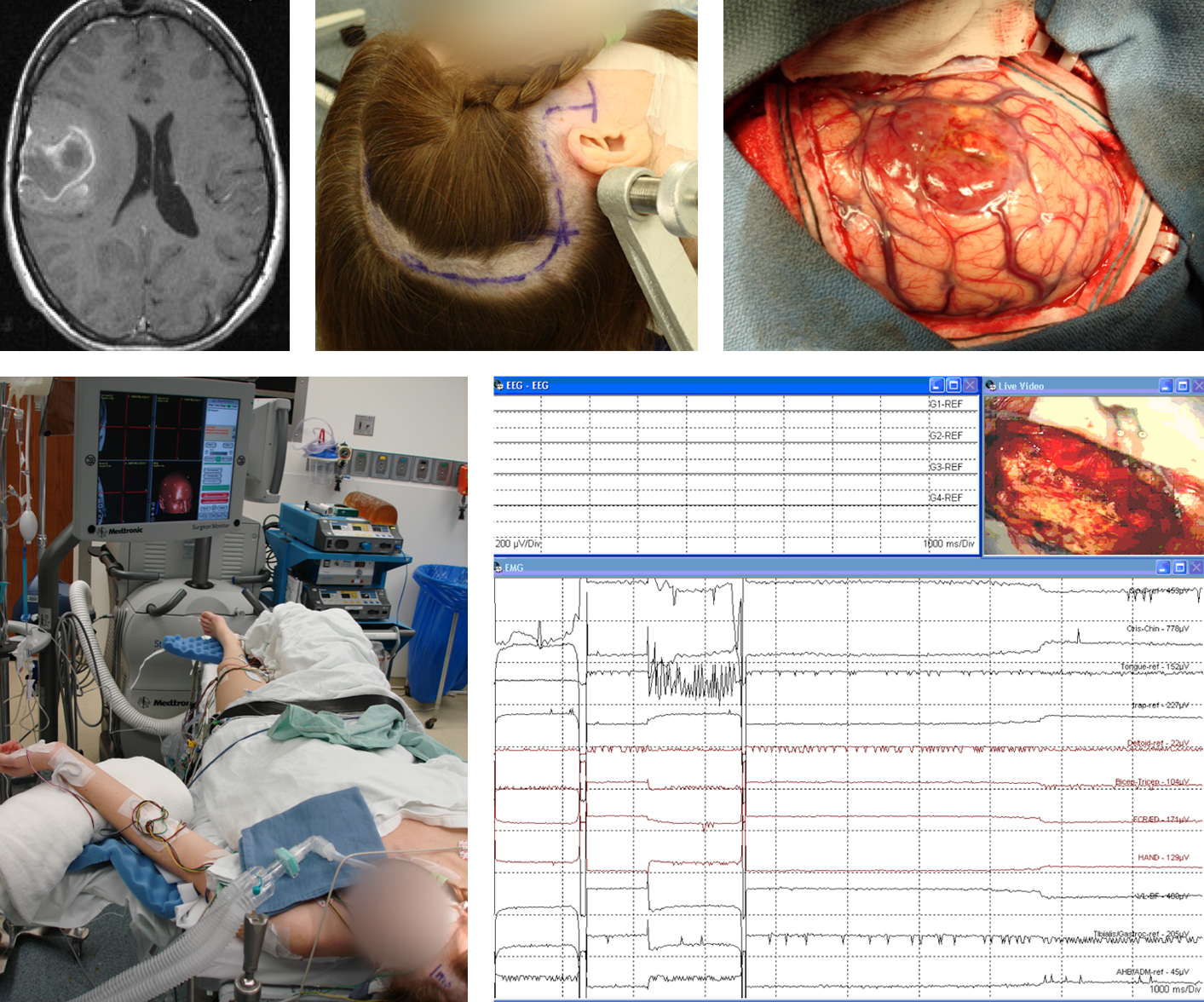
Figure 4: Preoperative MRI, patient positioning and scalp incision for resection of a Grade III anaplastic astrocytoma along the anterior inferior aspect of the right central lobule are demonstrated (upper row). The tumor extends posteriorly into the lower bank of the motor cortex. The bone flap is generous and designed to encompass the central lobule and at least 2 cm of the cortex around the perimeter of the tumor and functional cortices.
For sleep mapping, intraoperative electromyographic (EMG) monitoring is used and the patient’s contralateral limbs are uncovered so the neurophysiology team can readily detect any motor activity via direct visual inspection (left lower image). The contralateral limbs are also left free of intravenous lines and other implants. The right lower image demonstrates stimulation results and resultant facial muscle activity upon subcortical stimulation at the depth of resection cavity.
Mapping Technique
The results of sleep mapping can be affected by the method of anesthesia and immediate feedback via frequent intraoperative neurological exams is not available.
Figure 5: Mapping the motor cortex. A subdural strip electrode is used to detect afterdischarge potentials (Ha: hand; Sh: shoulder; Fo: foot). The location of the tumor is marked by “X.”
Awake stimulation mapping of the sensorimotor cortex is started at 1.5-2mA. This stimulation parameter is increased at 1-2 mA intervals until subjective or objective responses are elicited. Stimulation of the motor cortex leads to brief uncontrolled movements of the corresponding segments of the limb. Stimulation of the sensory cortex leads to subjective paresthesias. Sustained movements signify overstimulation/focal seizures, and ice-cold saline irrigation should be used to prevent progression to a generalized seizure.
For sleep mapping, delivering stimulus lasting 2 to 3s at 2mA is an appropriate starting point. The stimulus can be increased in 1 to 2mA increments to a maximum of 16mA. For comparison, the maximum current used for awake patients is typically 6-10mA. The generator should be set to deliver biphasic square wave pulses (1.25ms per phase) in 4-second trains at 60Hz. The bipolar electrode should be 1mm at its tips, separated by 5mm. Each cortical site is checked three times to ensure accuracy. Afterdischarge potentials indicate that the current is too high and needs to be decreased to avoid unreliable mapping and cortical spread of stimulation.
For mapping the motor cortex corresponding to the patient’s leg, a strip electrode is inserted along the falx and mapping completed over the medial precentral gyrus. Similarly, a subdural strip electrode may be used underneath the edges of the craniotomy where the dural opening is near but not immediately over the motor cortex.
Following cortical stimulation and during subcortical dissection, the descending fibers of the corticospinal tract can be traced anywhere from the cortex to the spinal cord by using the same protocol with slightly (1-2mA) higher stimulation parameters. Because functional fibers may be found engulfed within the tumor, subcortical mapping can be critical to guide tumor resection while preserving function.
After resection of the tumor, a final round of stimulation should be performed to evaluate functional integrity of the tracts. During repeat operations, if the dura is adherent to the underlying cortex and cannot be mobilized without a potential risk of pial injury, subcortical mapping is instrumental in mapping and monitoring function. Transdural cortical mapping is an option, but not very reliable.
Phase Reversal Technique Using Somatosensory Evoked Potentials
Somatosensory evoked potentials can be used to find the sensorimotor cortex quickly and safely using the “phase reversal” technique. An eight-contact strip electrode is placed transversely across multiple gyri and the contralateral median or tibial nerve is stimulated. The space between the two contacts where electrical phase reversal is detected defines the location of the central sulcus. Moving the electrode slightly and repeating this process can help the operator confirm the location of the sulcus.
Phase reversal is a safe and reliable method for identifying the central sulcus for resection of a lesion not directly infiltrating the functional cortices. This information may be used to find the appropriate trajectory and corticotomy site for resection of well-defined lesions such as metastatic tumors and cavernous malformations.
Other Considerations
The nondominant face motor cortex may be removed, apparently resulting in only temporary facial weakness. I have personally removed gliomas that infiltrated the face area and witnessed complete return of facial function as long as the underlying white matter tracts for the adjacent motor cortices were left intact.
During tumor resection, preservation of en passage vessels leading to the central lobule is imperative. Inadvertent injury to these vessels is one of the most common causes of unexplained postoperative neurologic morbidity.
Resection of the cortices just anterior to the motor cortex can lead to transient hemiplegia/hemiparesis or supplementary motor area (SMA) syndrome. Preservation of the underlying descending motor fibers that originate from the motor cortex and travel anteroinferiorly toward corona radiata is critical. This can be accomplished using subcortical mapping. Removal of or injury to the postcentral gyrus leads to disabling proprioception deficits. These deficits improve significantly over time, but some functional limitations in fine hand movement and gait will be permanent.
Case Examples
Case 1: A 32 year-old man presented with seizures and was diagnosed with a parietal low-grade glioma posterior to the central lobule.
Figure 6: Preoperative MRI and fMRI demonstrated the tumor to be posterior and inferior to the motor cortex (in yellow) (upper row). Awake cortical and subcortical mapping allowed reasonable resection of the mass (bottom row). Slight T2 hyperintensity anterior to the resection cavity is most likely residual tumor; subcortical mapping prohibited further resection in this area due to the presence of motor fibers.
Awake Mapping for Peri-Central Lobule Gliomas
Case 2: 35 year-old make presented with intractable seizures.
Figure 7: Preoperative images demonstrate a low-grade glial tumor located in the right periatrial region extending to the medial frontal lobe. Middle panel, upper image (coronal) and lower image (sagittal) functional MR images demonstrate the location of the sensorimotor cortex draped over the upper pole of the tumor. Diffusion tensor imaging (right upper image) reveals displacement of motor fibers by the tumor.
To avoid undue retraction on the ipsilateral functional cortices and reach the lateral pole of the tumor, I attempted a tranfalcine resection of the mass via a contralateral interhemispheric route.
Figure 8: A view of the operative trajectory via the transfalcine route is demonstrated (top image). I used cortical stimulation to map the medial frontal cortices anterior to the tumor. A “cross-court” approach was used to resect the tumor using subcortical mapping. Postoperative images demonstrate gross total resection of the mass without any complicating feature (bottom images).
Peri-atrial Glioma: Awake Mapping and Transfalcine Approach
Case 3: A 45 year-old male presented with left-sided focal motor seizures.
Figure 9: A right-sided central lobule glioma is found on imaging (left upper photo). The location of the lesion in the motor cortex may render it inoperable. However, diffusion tensor imaging (lower row) increased my confidence in the safety of resection by demonstrating the displacement of the functional fiber tracts. A gross total removal was achieved using awake cortical and subcortical mapping without infliction of any postoperative neurological deficit (right upper image).
Peri-Rolandic Glioma: Cortical and Subcortical Mapping
Postoperative Considerations
Antibiotics are used for 48 hours after surgery because of the limitations on sterile draping of the surgical field during awake procedures. Anticonvulsant drugs are used for 7 days in patients without seizures, and postoperative imaging is performed within 48 hours. The steroids are tapered slowly.
The risk of temporary postoperative deficits of sensorimotor function is significant, especially with tumors directly infiltrating the sensorimotor cortices. If function is intact or mildly compromised at the end of the operation, but worsens on the first postoperative day, the opportunity for meaningful recovery is substantial. However, a significant decline at the end of the operation usually signifies an irreversible direct or ischemic injury. The most common reason for neurologic decline on the first postoperative day is subclinical seizures.
Supratherapeutic levels of anticonvulsant medications are necessary for the immediate postoperative period. Seizures delay neurologic recovery and are very disheartening to the patient’s family.
Pearls and Pitfalls
- Careful preoperative imaging evaluation determines the anatomic location of the sensorimotor gyri and selection of an appropriate mapping strategy.
- Phase reversal is a safe and reliable method for identifying the central sulcus for resection of well-defined lesions that do not directly infiltrate the functional cortices.
- Patients with lesions near the central lobule may undergo sleep mapping, but if the lesion directly infiltrates these cortices and their corresponding descending tracts, awake mapping may be more reliable. The awake method is unaffected by anesthesia and allows direct patient feedback via frequent intraoperative neurological examinations.
Contributor: Richard Kim, MD
References
Keles GE, Berger MS. Functional mapping, in Berstein M, Berger MS (eds): Neuro-oncology: The Essentials. New York: Thieme Medical Publishers, 2011.
Please login to post a comment.