Pineoblastoma
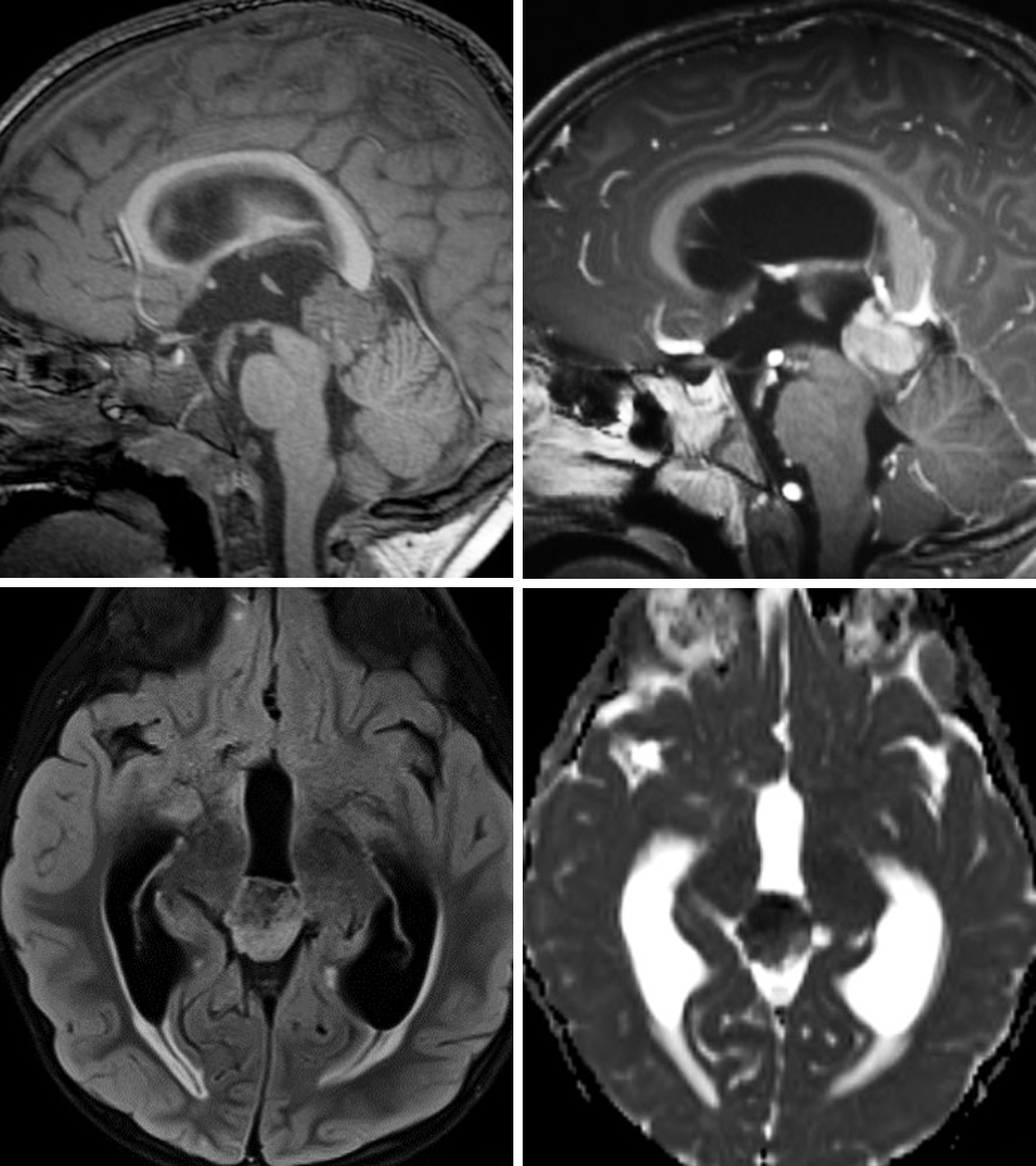
Figure 1: (Top Left) This pineoblastoma demonstrates invasion into the superior tectal plate on sagittal T1WI. (Top Right) After administration of intravenous contrast, the lesion demonstrates avid, heterogeneous enhancement. (Bottom Left) Axial FLAIR demonstrates hyperintensity typical of most tumors. (Bottom Right) This lesion has also caused obstructive hydrocephalus at the cerebral aqueduct. ADC imaging shows low-signal/restricted diffusion reflecting this lesion's hypercellularity.
Figure 2: This complex cystic lesion centered in the pineal region demonstrates enhancement when comparing precontrast (top left) and postcontrast (top right) sagittal images. The mass appears well circumscribed, a finding that could be present with pineoblastomas. They can look very similar to germ cell tumors or even lower-grade primary pineal tumors. The restricted diffusion on DWI (bottom left) and ADC imaging (bottom right) also implies hypercellularity of a higher-grade tumor.
Figure 3: (Top Left and Top Right) Although centered in the pineal region, this heterogeneously enhancing lesion demonstrates the infiltrative appearance on axial and coronal postcontrast T1 imaging that can help to distinguish pineoblastoma from lower-grade primary pineal tumors. (Bottom) Cystic/necrotic changes are also visible in this large lesion on sagittal T2 imaging.
BASIC DESCRIPTION
- Malignant, invasive pineal parenchymal tumor arising from embryonic pineocyte precursors (PNET)
PATHOLOGY
- WHO grade IV
- Invades adjacent structures, often including the cerebral aqueduct
- Cerebrospinal fluid (CSF) dissemination common
- Hypercellularity and increased mitoses are characteristic features
- Associated with germline DICER1 mutations (DICER1 syndrome) and RB1 (bilateral retinoblastoma and pineoblastoma)
CLINICAL FEATURES
- Most commonly afflicts children in the first decade of life (mean age, 3 years)
- No clear gender predilection
- Common presenting signs/symptoms
- Hydrocephalus: headache, nausea, vomiting, altered mental status, papilledema
- Parinaud syndrome (upgaze palsy)
- Absent serum tumor markers (differentiates from many germ cell tumors)
- Prognosis: poor prognosis; 5-year survival, ~50%
IMAGING FEATURES
- General
- Lobulated, poorly marginated pineal mass
- Might be indistinguishable from lower-grade pineal tumors
- Often larger and more invasive than pineocytomas
- Peripheral (“exploded”) calcifications common
- Commonly invades adjacent structures, including cerebral aqueduct, corpus callosum, thalamus, brainstem, and vermis
- Could see superior displacement of cerebral veins and mass effect on the tectum
- CT
- Heterogeneous density, irregular pineal mass
- Peripheral calcification
- Variable, patchy enhancement on contrast-enhanced CT imaging
- MRI
- T1WI: heterogeneously hypointense to isointense
- T2WI: heterogeneous signal; hyperintense peritumoral edema within the surrounding brain parenchyma common
- T1WI+C: heterogeneous enhancement
- DWI: diffusion restriction in solid component of mass common
- MRS: elevated Cho, decreased NAA
IMAGING RECOMMENDATIONS
- http://doi.org/10.1177/1051228405001514MRI without and with intravenous contrast including both brain and spine due to risk of CSF dissemination
For more information, please see the corresponding chapter in Radiopaedia.
Contributor: Rachel Seltman, MD
References
Cuccia V, Rodríguez F, Palma F, et al. Pinealoblastomas in children. Childs Nerv Syst 2006;22:577–585. doi.org/10.1007/s00381-006-0095-6.
Gasparetto EL, da Cruz LCH Jr, Doring TM, et al. Diffusion-weighted MR images and pineoblastoma: diagnosis and follow-up. Arq Neuropsiquiatr 2008;66:64–68. doi.org/10.1590/s0004-282x2008000100015.
Hirato J, Nakazato Y. Pathology of pineal region tumors. J Neurooncol 2001;54:239–249. doi.org/10.1023/a:1012721723387.
Nakamura M, Saeki N, Iwadate Y, et al. Neuroradiological characteristics of pineocytoma and pineoblastoma. Neuroradiology 2000;42:509–514. doi.org/10.1007/s002349900243.
Osborn AG, Salzman, KL, Jhaveri, MD. Diagnostic Imaging (3rd ed). Elsevier, Philadelphia, PA; 2016.
Reis F, Faria AV, Zanardi VA, et al. Neuroimaging in pineal tumors. J Neuroimaging 2006;16:52–58. doi.org/10.1177/1051228405001514.
Please login to post a comment.