Neurocysticercosis
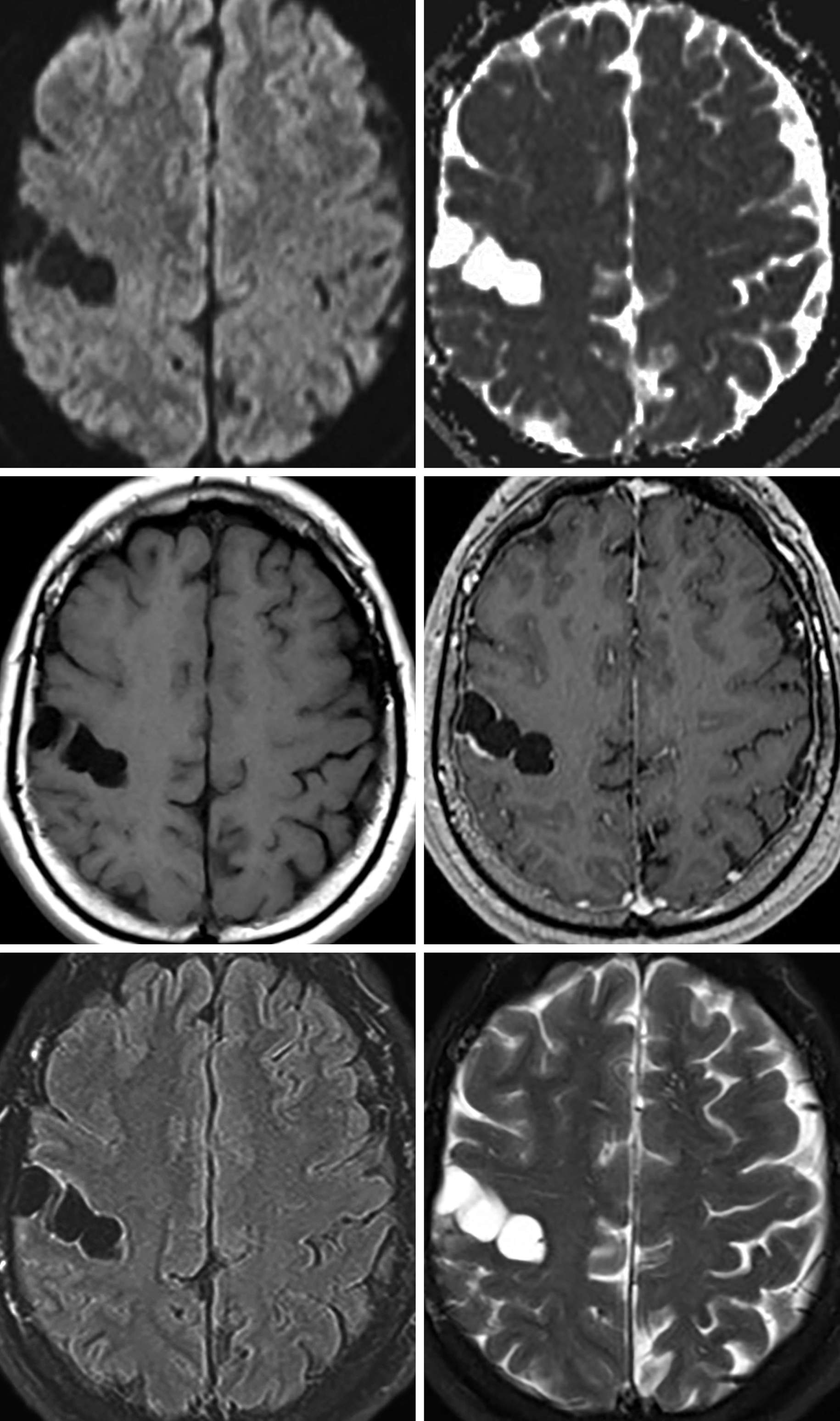
Figure 1: Cluster of cyst-like structures in the right central sulcus compatible with racemose neurocysticercosis. (Middle Right) Notice that there is only minimal rim enhancement. Often, when in the subarachnoid space or basilar cisterns, neurocysticercosis will take on a grape-like appearance with minimal to no enhancement.
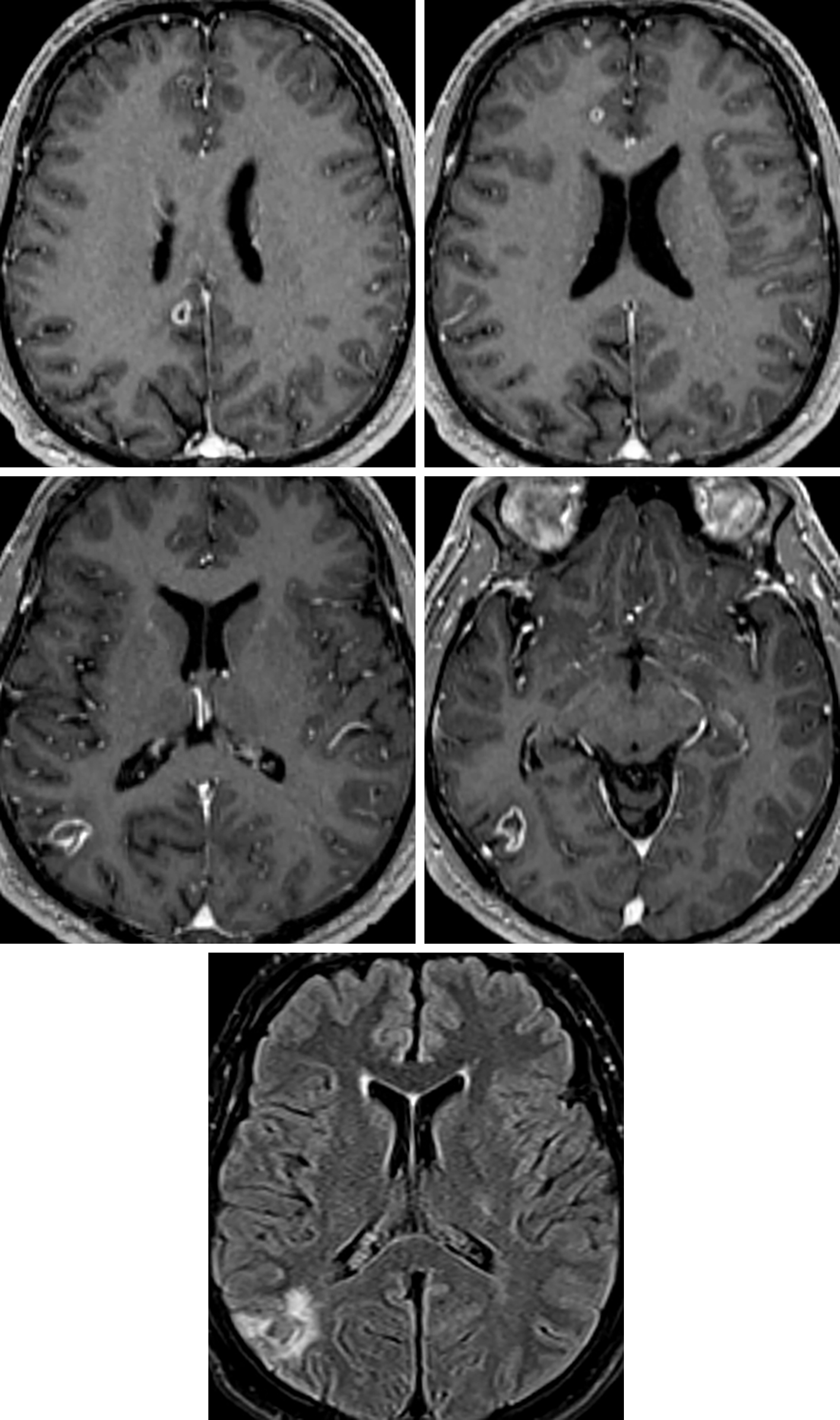
Figure 2: Multiple peripherally enhancing neurocysticercosis lesions (top left, middle right) look remarkably similar to brain metastases, with a similar amount of associated hyperintense vasogenic edema on FLAIR imaging (bottom). (Middle Left) The patient’s clinical scenario and the presence of an eccentric mural nodule in some of the lesions can help to narrow the differential.
Description
- Intracranial parasitic infection caused by the pork tapeworm Taenia solium
Pathology
- Four pathologic stages
- Vesicular
- Colloidal vesicular
- Granular nodular
- Nodular calcified
Clinical Features
- Symptoms
- Typically asymptomatic until larvae degenerate
- Seizure, headaches, hydrocephalus
- Demographics
- Any age but commonly young and middle-aged adults
- Slight male predominance
- More commonly seen in certain locations, such as Latin America
- Prognosis
- Increased morbidity and mortality with intraventricular neurocysticercosis
Imaging
- General
- Imaging varies with developmental stage and host response
- Often multiple stages in same patient
- Usually small lesions that can have exuberant cerebral edema, depending on the stage
- Most commonly visible within the subarachnoid space over the cerebral convexities
- May develop an inflammatory response that seals the sulcus and can be mistaken for a parenchymal lesion
- Racemose subtype: grape-like lesions in the basal cisterns
- CT
- Vesicular
- Small thin-walled cyst isodense to cerebrospinal fluid (CSF)
- Central dot sign—hyperdense dot within the cyst represents a protoscolex
- Vesicular
- Colloidal vesicular
- Usually small hyperdense cyst with a thick ring-enhancing fibrous capsule and surrounding edema
- Granular nodular
- Involuting enhancing nodule
- Nodular calcified
- Small calcified nodule
- MRI
- Vesicular
- T1, T2, and FLAIR
- Cystic lesions isointense to CSF, may see discrete eccentric intermediate-signal-intensity scolex
- T1, T2, and FLAIR
- Colloidal vesicular
- T1, T2, and FLAIR
- Cyst is hyperintense to CSF
- T1, T2, and FLAIR
- Granular nodular
- T1, T2, and FLAIR
- Thickened, retracted cyst wall, edema decreases
- T1, T2, and FLAIR
- Nodular calcified
- Shrunken low-signal-intensity lesion on all sequences, seen most easily on GRE/SWI
- May not be visible
- DWI: not particularly helpful
- GRE/SWI: useful for demonstrating calcified scolex
- Contrast
- Vesicular: minimal enhancement of the scolex
- Colloidal vesicular: enhancement of the wall and scolex
- Granular nodular: nodular or ring-like enhancement
- Nodular calcified: minimal
- Vesicular
- Imaging recommendations
- MRI with contrast (include SWI)
- Mimic
- Depends on the phase of disease at which the particular lesion is. In the vesicular phase, can mimic an arachnoid cyst or enlarged perivascular space. The multiplicity and location of the lesions can help distinguish them. When in the colloidal vesicular or granular nodular phase, they can be difficult to distinguish from metastatic disease. Oftentimes, the most helpful way to distinguish them is by identifying multiple lesions in multiple different stages.
For more information, please see the corresponding chapter in Radiopaedia.
Contributor: Sean Dodson, MD
References
Kimura-Hayama ET, Higuera JA, Corona-Cedillo R, et al. Neurocysticercosis: radiologic-pathologic correlation. Radiographics 2010;30:1705–1719. doi.org/10.1148/rg.306105522
Lucato LT, Guedes MS, Sato JR, et al. The role of conventional MR imaging sequences in the evaluation of neurocysticercosis: impact on characterization of the scolex and lesion burden. AJNR Am J Neuroradiol 2007;28:1501–1504. doi.org/10.3174/ajnr.A0623
Rabelo NN, et al. Differential diagnosis between neoplastic and non-neoplastic brain lesions in radiology. Arq Brasi Neurocir Braz Neurosurg 2016;35:45–61. doi.org/10.1055/s-0035-1570362
Shih RY, Koeller KK. Bacterial, fungal, and parasitic infections of the central nervous system: radiologic-pathologic correlation and historical perspectives: from the radiologic pathology archives. Radiographics 2015;35:1141–1169. doi.org/10.1148/rg.2015140317
Please login to post a comment.