Operating Room Etiquette Free
“People may not remember exactly what you did, or what you said, but they will always remember how you made them feel.” Carl W. Buehner
The operating room (OR) is an intimidating setting for most neurosurgery residents, particularly during their early years of training. Every senior resident and attending surgeon can recall an incident of tension in the OR such as an uncontrolled intraoperative aneurysm rupture. The emotional reactions of the surgeon are the most memorable takeaways from these situations. Learning to be prepared for these occurrences and to effectively communicate can prevent or minimize the risks associated with these events. A skilled communicator is aware of the immense valance of his or her words.
The attending surgeon serves as the leader and “the captain of the ship” in the OR, guides the team, and sets the tone for interactions and emotions in the OR environment. The team expects exemplary professional behavior from the attending as a role model, and it is this leadership that maintains the OR as an efficient and safe place. The attending surgeon must possess effective communication skills, demonstrate respect for all team members, and maintain a sense of confidence. Historically and unfortunately, some iconic attending surgeons have not consistently demonstrated these qualities.
The culture of the OR has been dominated recently by mandates to maximize patient safety. This change has provided residents more responsibility to request help or guidance, which can create an internal conflict within a trainee who seeks the embedded character traits of independence, confidence, and determination. These traits are widely viewed as desirable in trainees and were the major facets of the previous surgical culture.
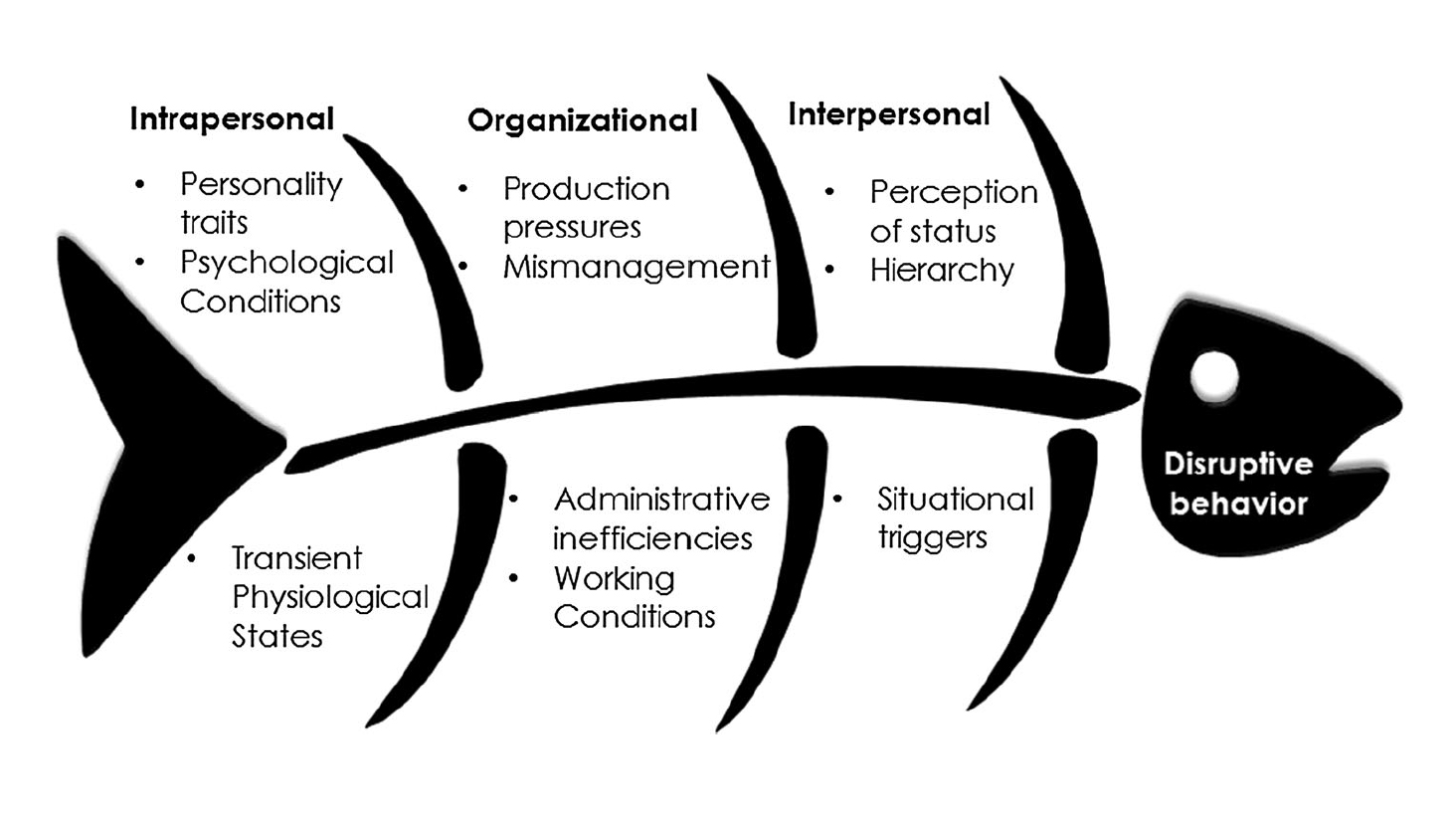
Surgeons have historically been considered inflexible and uncompromising and have acknowledged themselves to be at the peak of the hierarchical ladder of medicine. The OR environment has historically embellished this climate and identified the “disruptive physician” as the attending surgeon. The common causes of disruptive behavior are listed in Figure 1.
Figure 1: Ishikawa diagram analyzing the antecedent factors guiding disruptive behavior. Image credit to Villafranca et al (2017).
To discuss the operating room climate and appropriate etiquette, I am including this chapter, divided into resident’s and attending surgeon’s responsibilities. Ultimately, each resident and attending surgeon should continue to advance his or her self-awareness/mindfulness and recognize when he or she will be most vulnerable to demonstrating disruptive behavior. This self-awareness and emotional intelligence is critical for guiding the surgeon in stressful times. For example, I am most vulnerable late in the day when I am not rested (post-call), preoccupied with a recent poor patient outcome, and find myself involved in a very challenging case filled with unexpected technical difficulties while an inexperienced surgical team is assisting me. I recognize these situations and my shortcomings, control my emotions, and proactively remain nonjudgmental.
Figure 2: Disruptive behaviors on the part of the surgeon have a widespread impact on trainees and staff, as described in the Negative Consequences box. Coping strategies are described in the Management Strategies box.
RESIDENT’S RESPONSIBILITIES
The resident surgeon is responsible for the paramount task of learning to become the leader in the OR. This role is not naturally attained by any trainee but instead requires the resident to rise to the challenge in times of tension and command the respect of the team. This respect must be earned (a privilege, not a right!), and therefore this role takes time, coaching, and experience to attain.
As the impressionable resident observes the well-established attending surgeon in the OR, it is important that he or she is mindful that not all the behaviors demonstrated by the surgeon are desired in the OR setting. Every surgeon has his or her own strengths and weaknesses as a leader.
It is also challenging for a resident to emulate the positive qualities of an attending, given that the OR is an intimidating place and requires the junior resident to lead and maintain composure even when he or she lacks confidence. This fact highlights the importance of establishing leadership traits as a medical student.
Developing confidence in the OR requires a multifaceted approach in which the resident establishes self-confidence through diverse experiences and technical skills. Persuasion and leadership are developed via understanding, goals, leverages, and influences (“UGLI”).
- Understanding (clarity of context and challenge)
- “You cannot change what you do not understand.” Take the time and get to know the OR team and the dynamic working relationships. Analyze the challenges and opportunities.
- Goals (shared outcomes and urgency)
- “Define success. Identify and communicate outcomes.” Describe what you characterize as the success of the team as a whole. Use metrics to define progress.
- Leverage (momentum and champions)
- “Do not do it alone. Other people have some skin in this game” All of us find individuals in the OR who immediately appreciate our friendship, celebrate our successes and share our goals. Appropriately use their support to persuade skeptics and convert the blockers.
- Influence (commitment, not compliance)
- “Do not just hope to persuade and change behaviors. What are your evidence-based influence strategies?” Define actions that inspire others to follow you and believe in your vision, not based on your status, but based on your influential values. Begin to see where key stakeholders will have energy around new initiatives.
Achieving confidence in oneself and the team is a diverse concept, but it can be attained through coaching and practicing to form a habit. An easy step in reaching confidence is meticulous preparation. Preparation allows the resident to inform the team of the goals and critical steps of the procedure at the start of the case. The preoperative discussion with the team also serves to empower residents in their role in the OR and establishes the approachability of the surgeon.
The operative plan also facilitates clear communication among the other team members, including circulating nurses, anesthesiologists, surgical technologists, and medical students. With thorough preparation, the resident is able to communicate clearly, anticipate each step of the procedure, and lead the team to achieve the ultimate goals of the operation.
A list of management strategies for dealing with disruptive behavior is shown in Figure 2. These techniques are not a collection of remedies for the root of the problem but, rather, offer only temporary relief for each episode.
The most common strategy for dealing with disruptive surgeons is debriefing with colleagues. This activity provides a productive way to dissipate the emotions generated from working in a hostile OR setting.
The externalization of a disruptive surgeon’s behavior permits depersonalization of the episode and thereby permits the trainee to dissociate the surgeon’s anger during the situation from the trainee’s performance.
An additional simple strategy for coping with a disruptive surgeon is future avoidance of the situation. This strategy is often used by residents and OR staff in response to a known “repeat offender.” Although not always appropriate and certainly not a definitive answer, avoidance can be used as long as it does not compromise patient care.
ATTENDING SURGEON’S RESPONSIBILITIES
This leader in the OR concept can be likened to being the “captain of the ship,” given that there is one person who is ultimately responsible for the outcome of the voyage. This concept was exemplified historically in the surgical profession when, in a Pennsylvania court in 1949, McConnell v Williams found an obstetrician responsible for an intern giving an inappropriate dose of eye drops resulting in blindness of a newborn. The attending obstetrician was in no way involved or even aware of the intern’s actions; however, he was found ultimately responsible for the incident. Therefore, just as a captain is responsible for the actions of his or her crew, so is the attending physician responsible for the actions of all members of the OR staff and trainees.
As mentioned previously, the attending surgeon must serve as a role model for the residents and OR staff. As a result, residents who have trained in different programs present different defense mechanisms when faced with similar stressful situations.
A disruptive attending surgeon can have an immense impact on the patient, medical students, resident physicians, and OR staff. Examples of disruptive behaviors include profanity, insensitive attitudes, derogatory comments, and hyperactivity. For a more complete list of these behaviors, see Table 1.
| Organization | Definition | Generalized Examples | Excluded Behaviors |
| Council on Ethical and Judicial Affairs, American Medical Association | Verbal or physical conduct that does, or may, negatively affect patient care | Foul language | Good-faith criticism |
| Threatening language | |||
| Aggressiveness | |||
| Hyperactivity | |||
| Intrusiveness | |||
| Irritability | |||
| Being argumentative | |||
| Canadian Medical Protective Association | Can interfere with communication between team members or with patients, potentially affecting patient care and patient satisfaction | Derogatory comments | Good-faith advocacy for a patient |
| Dismissive comments | Complaining to an outside agency | ||
| Insensitive, uncaring, callous attitudes | Testifying against a colleague | ||
| Inappropriate language | Professionally written alerts | ||
| Profanity | |||
| Bullying | |||
| Threats | |||
| Demeaning conduct | |||
| Angry outbursts | |||
| Demeaning conduct | |||
| Condescending conduct | |||
| Aggressive conduct | |||
| Boundary issues | |||
| Joint Commission on Accreditation of Hospital Organizations (JCAHO) | Conduct that intimidates others to the extent that quality and safety and compromised | Verbal outbursts | None provided |
| Physical threats | |||
| Refusing to perform assigned tasks | |||
| Reluctance to answer questions | |||
| Quietly exhibiting uncooperative attitudes | |||
| Condescending language |
Credit to Villafranca et al (2017) for the content of this table.
The prevalence of disruptive behavior in the physician community is debated and most likely significantly underestimated, in part because of the lack of a standard definition for disruptive behavior by the medical profession.
Disruptive behaviors result in a shift of attention away from the patient and to the surgeon. Although the surgeon is potentially the internal motivator for seeking attention while exhibiting disruptive behavior, the end result is generally a loss of respect for the surgeon.
Disruptive behavior by the attending surgeon can dissuade a trainee from pursuing a career as a surgeon. It can also result in attrition among trainees and staff because of the grim outlook of working under such hostile conditions for a prolonged time. The loss of talent will adversely affect the work environment further, leading to a vicious cycle.
Disruptive behavior can also result in increased procedural errors. When members of the team feel threatened, they are less likely to be proactive about events that could precipitate a “never” event due to the fear of repercussions from the attending surgeon. Team members may also be distracted from patient care activities given their preoccupation with defusing and pacifying the disruptive experience.
Management of disruptive behavior raises the obvious question of whether a “repeat offender” is capable of learning a more appropriate method of functioning in the OR. As depicted in Figure 3, it is important for remediation to occur with a follow-through on disciplinary action if change does not take place. These behaviors should not be taken lightly given their negative consequences.
The appropriate behaviors for a surgeon can follow the guidelines established for civility within the greater population. Examples of these behaviors include respect, self-awareness, and kind speech. A more extensive list can be seen in Table 2. A survey-based list with major and minor themes is shown in Table 3.
| John Hopkins Rules of Civility that are applicable to the operating room | The Ontario Medical Association's fundamentals of civility |
| Acknowledge others: their presence, worth, and effort | Respect others and yourself |
| Respect others' opinions, time, and space (physical and emotional) | Communicate effectively |
| Speak kindly | Be aware |
| Do not blame | Be responsible |
| Keep it down | Take good care of yourself |
| Respectfully assert yourself |
Credit to Villafranca et al (2017) for the content of this table.
| Major Theme | Subtheme | Observed Behaviors |
| Calmness | Calmed patient | Allayed fears; calming talk; put at ease; reassuring; relaxed; relieved anxiety; soothing; supportive; took time; treated kindly; used humor to relieve anxiety |
| Remained calm professionally | Appropriate handling of a difficult situation; calm under fire; kept cool; maintained composure; stayed calm | |
| Teamwork | Cooperative team member | Deferred to expertise; visibly cooperative; worked together |
| Communicative | Aware of actions and apologetic; complimentary; considerate of others' responsibilities; explaining; good communication in adversity; good coordination; friendly greeting; kept informed and let others know of potential problems; reassuring | |
| Collegial | Didn't yell at one another when under duress; good camaraderie; good rapport; humor as team stress reducer; offered help; pleasant; relaxed environment; showed mutual respect; spoke well of others | |
| Cooperative in patient care | Acknowledging limitations; collectively explained and reassured; supported other provider(s) in front of patient; team worked together in reassuring patient | |
| Teaching | Role | Focused on learning and good teaching; constructive advice; "pimping," teasing, and questioning in a friendly way; willing, took time and made opportunity to teach; considerate within supervision; role-modeling of self-control; asking probing questions; developed a shared understanding |
| Inclusive | Invited; shared sense of belonging, supportive of medical student involvement; welcomed medical student | |
| Supportive | Encouraging; supportive of resident | |
| Patient Communication | Explained to patient | Explained plan; gave appropriate information; listened to patient while in process of explaining |
| Prioritized patient | Patient given sense of dignity or control; prioritized concerns | |
| Comfort | Comforted patient | Compassionate; ensured comfort; extra effort to make patient feel better; proactive in comforting and reassuring; warm interaction |
| Respect | To team | Thanked all; took time to explain situation to team |
| To patient | Being supportive; considerate; empathy; kind to patient; sincerely demonstrated humanity; sympathy and compassion | |
| Courteous | Asked nicely; courteous; resident apologized to nurse |
Credit to Currey et al (2011) for the content of this table.
CONCLUSIONS
For a surgeon, the process of becoming the “captain of the ship” in the OR is a challenging but rewarding task. When all goes well, the end result is an efficient team with the patients' best interest in mind. It allows each team member to provide input within the realm of his or her role, and it encourages each member to promote the team’s success. It is through the demonstration of respect, effective communication, and thorough preparation that a resident can attain the role of the “captain of the ship.”
PEARLS AND PITFALLS
- Each resident and attending surgeon should continue to advance his or her self-awareness/mindfulness and recognize when he or she will be most vulnerable to demonstrating disruptive behavior.
Contributor: Benjamin K. Hendricks, MD
References
Achor T, Ahn J. Becoming the “captain of the ship” in the OR. J Orthop Trauma 2014;28:S18–S19. doi.org/10.1097/BOT.0000000000000180.
Cochran A, Elder WB. Effects of disruptive surgeon behavior in the operating room. Am J Surg 2015;209:65–70. doi.org/10.1016/j.amjsurg.2014.09.017.
Curry SE, Cortland CI, Graham MJ. Role-modeling in the operating room: medical student observations of exemplary behavior. Med Educ 2011;45:946–957. doi.org/10.1111/j.1365-2923.2011.04014.x.
Hickson GB, Pichert JW, Webb LE, Gabbe SG. A complementary approach to promoting professionalism: identifying, measuring, and addressing unprofessional behaviors. Acad Med 2007;82:1040–1048. doi.org/10.1097/ACM.0b013e31815761ee.
Murphy EK. “Captain of the ship” doctrine continues to take on water. AORN J 2001;74:525–528. doi.org/10.1016/s0001-2092(06)61686-4.
Villafranca A, Hamlin C, Enns S, Jacobsohn E. Disruptive behavior in the perioperative setting: a contemporary review. Can J Anesth 2017;64:128–140. doi.org/10.1007/s12630-016-0784-x.
Please login to post a comment.