Temporal/Subtemporal Craniotomy Free
This is a preview. Check to see if you have access to the full video. Check access
Techniques for Performance of Temporal Craniotomy
Please note the relevant information for patients undergoing craniotomy is presented in another chapter. Please click here for patient-related content.
General Considerations
Temporal craniotomy is a simple approach that has vast applicability to intra-axial and extra-axial pathologies. The subtemporal approach provides a wide operative corridor to the floor of the middle fossa and upper petroclival territories and their associated cisterns. More specifically, this corridor reaches the anterior upper brainstem through the anterior petrosectomy.
The lateral neocortical temporal lobe and more specifically the dominant superior and posterior parts of the middle temporal gyri affect important functions such as language. The exact function of the anterior middle temporal gyrus is unknown, but it may be involved in processes such as contemplating distance, recognition of known faces, and accessing word meaning while reading (see Wikipedia).
The inferior temporal gyrus is involved with visual processing, associated with the representation of complex object features, such as global shape. It may also process face perception and the recognition of numbers (see Wikipedia).
Indications for the Procedure
Temporal craniotomy is beneficial for resection of mid to posterior intraparenchymal and convexity temporal lobe tumors. This route also affords access to mid hippocampal lesions through the transsulcal approach and reaches lateral thalamic tumors and basal cisterns through the transcortical transventricular transchoroidal pathway. The exposure of the Sylvian fissure is limited.
A subtemporal craniotomy is more versatile and exposes various neoplastic and tumorous intradural and extradural pathologies of the middle fossa floor, anterior basal cisterns, and upper clivus. Middle fossa meningiomas, small acoustic tumors and trigeminal schwannomas, low-lying basilar caput/upper basilar artery aneurysms, and upper petroclival meningiomas (through the anterior petrosal approach) are some examples of lesions readily reached via this route.
In addition, this approach allows repair of the superior semicircular canal dehiscence. The subtemporal approach can be used in combination with the extended pterional route for access to complex vascular abnormalities of the interpeduncular cisterns and fibrous multicompartment menigniomas filling the medial incisural and parachiasmatic space.
Preoperative Considerations
The location of the vein of Labbe and its drainage site into the transverse sinus should be estimated preoperatively based on magnetic resonance (MR) venogram for cases that require posterior subtemporal exposure. This drainage site is about 1cm superior to a line parallel to the superior border of the zygomatic arch and 2 to 5 cm (mean 2.9 cm) posterior to the opening of the external auditory meatus.
The displacement of other arterial and venous structures along the medial tentorium should be defined. The potential need for a combined approach to tumors with both supratentorial and infratentorial extensions should be planned preoperatively.
Mannitol (1g/Kg) should be administered during skin incision if a “tight” brain is expected. If cortical stimulation for functional mapping is contemplated, cold lactated Ringer’s solution should be available. In expectation of a subtemporal approach, I generally place a lumbar drain for most patients, regardless of their tumor size, in order to minimize the risk of temporal lobe retraction injury during intradural or extradural elevation of the lobe. Since the basal cisterns are not reached until after elevation of the lobe, alternative routes for early cerebrospinal fluid (CSF) drainage is beneficial.
The surgeon is positioned at the head of the operating room table with the surgical technician at either the right or left, depending on the handedness of the surgeon. The anesthesiologist may be situated at the foot of the table, allowing more working room for the assistant and microscope if necessary.
Operative Anatomy
Depending on the skin incision, the superficial temporal artery may or may not be involved in execution of the approach. The artery typically runs one finger-breadth anterior to the tragus and bifurcates into its frontal and parietal branches approximately 5 cm superior to the zygoma. The temporal branch of the facial nerve is located more anteriorly over the zygoma and superficial to the two layers of the anterior superficial temporal fascia.
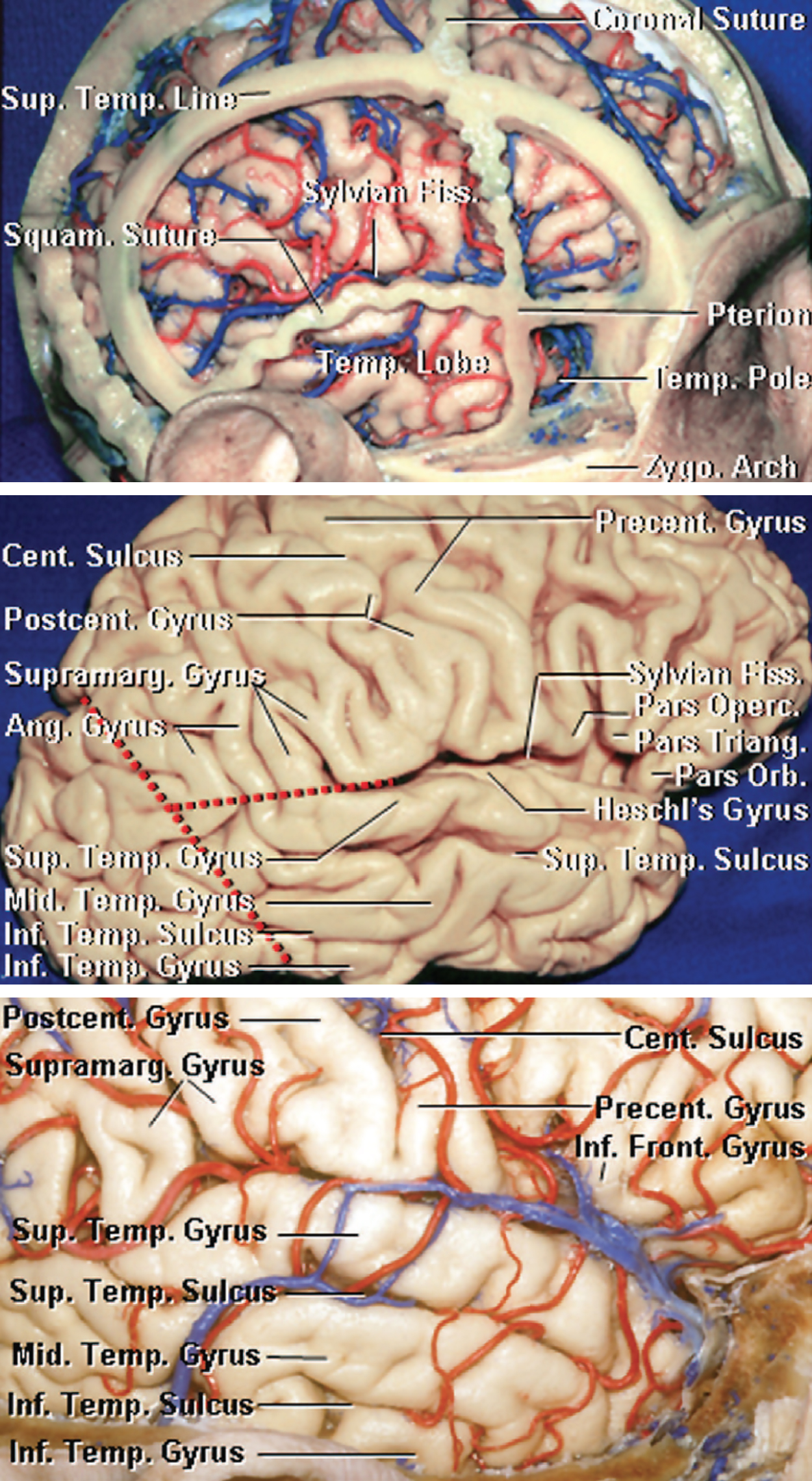
The root of the zygoma is an essential landmark to define the level of the middle fossa floor. This landmark should be used for planning the initial burr hole and subsequent craniotomy. Preservation of the vein of Labbe is essential. Its anatomic relationships are illustrated in the following images.
Click here to view the interactive module and related content for this image.
Figure 1: Relationship of the cranial sutures to the temporal lobe and Sylvian fissure (Top image). Note the squamosal suture overlying the Sylvian fissure, in addition to delineating the superior limit of the temporal lobe. Also, the importance of performing the craniectomy to the level of the zygomatic arch is illustrated in this dissection. Cortical topography of the temporal lobe is illustrated in the other images (Images courtesy of AL Rhoton, Jr).
Figure 2: Venous anatomy of Sylvian and posterior temporal regions. The vein of Labbe runs a variable course toward the transverse sinus, but must always be preserved, especially during combined approaches to the posterior temporal region. Locating this vessel is critical for preventing its injury and temporal lobe venous infarction. Middle temporal vein should not be confused with the vein of Labbe (Image courtesy of AL Rhoton, Jr).
TEMPORAL/SUBTEMPORAL CRANIOTOMY
Appropriate head position is paramount for surgery on deep skull base lesions. The patient’s head position should direct the surgeon to the region of interest through a path that allows adequate exposure of the lesion, minimizes brain retraction, and affords flexible working angles. Furthermore, the patient’s head position should enable a comfortable ergonomic body posture for the surgeon during the operation.
Figure 3: The patient is frequently placed in the supine position (if the patient’s neck is supple) or rarely in the lateral position, if the neck is relatively rigid. The patient’s neck should be rotated as much as possible while utilizing a large shoulder roll underneath the ipsilateral shoulder to minimize neck torsion. Nonphysiologic neck rotation leads to compromised jugular venous return and postoperative neck pain.
Older and heavy-set patients should be placed in a lateral position. If the patient has a history of significant cervical spondylosis, this dictates the need for a lateral position. The head is then tilted ~20 degrees toward the floor for gravity retraction to mobilize the temporal lobe away from the middle fossa.
The exact location and size of the lesion will determine the corresponding skin incision. In general, smaller lesions that are within the superior or middle temporal gyri are amenable to linear incisions, whereas large subtemporal lesions benefit from a horseshoe-shaped incision. For lesions that require access to the anterior temporal pole, a small reverse question mark incision would be appropriate.
Figure 4: Alternative incision styles and pin placement for temporal and subtemporal craniotomies. An incision that extends to the level of the zygoma should spare the main trunk of the superficial temporal artery. Manual palpation of the artery guides planning of the scalp flap. I prefer a linear incision when possible since this type of incision heals more readily. Horizontal disconnection of the temporalis muscle attachments from the superior temporal line through the linear incision often maximizes retraction of the scalp flaps and provides adequate bony exposure.
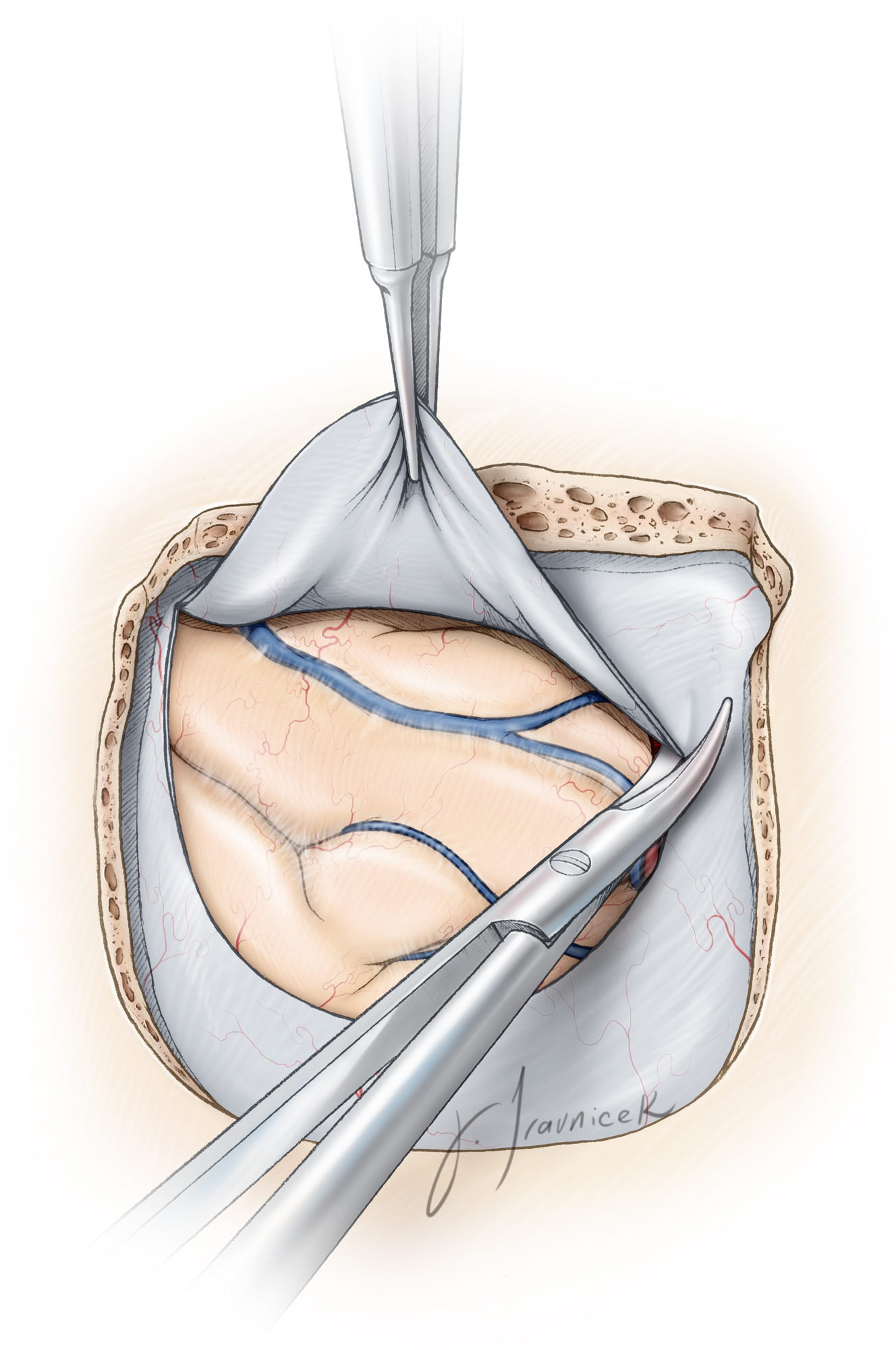
After placing a generous single burr hole just above he root of the zygoma, I use a #3 Penfield dissector to mobilize the dura away from the inner table of the calvarium in preparation for the craniotomy. If an extradural approach to the middle fossa is planned, it is essential to avoid early injury to the dura in order to protect the lobe during extradural subtemporal dissection and petrosectomy.
If the dura is adherent to the inner skull bone, I place numerous burr holes. The lumbar drain is used to remove ~30 to 40cc of CSF gradually (in 10–20cc aliquots) to relax the brain. This drainage facilitates dissection of the dura from the calvarium and reduces the risk of a dural tear. A craniotome is then used to complete the craniotomy.
Figure 5: Note the location of the initial burr hole near the sigmoid sinus for linear (top) and horseshoe (bottom) incisions. In the case of a subtemporal operative corridor, the craniotomy should be created as close to the middle fossa floor as possible. This task may be accomplished by identifying one important landmark: the upper edge of the root of zygoma marks the level of the middle fossa floor. It is also important to remember that the floor of the middle fossa is oblique and slopes slightly superiorly from the anterior to posterior direction. Therefore, the inferior edge of the craniotomy should be only slightly above the level of the zygoma.
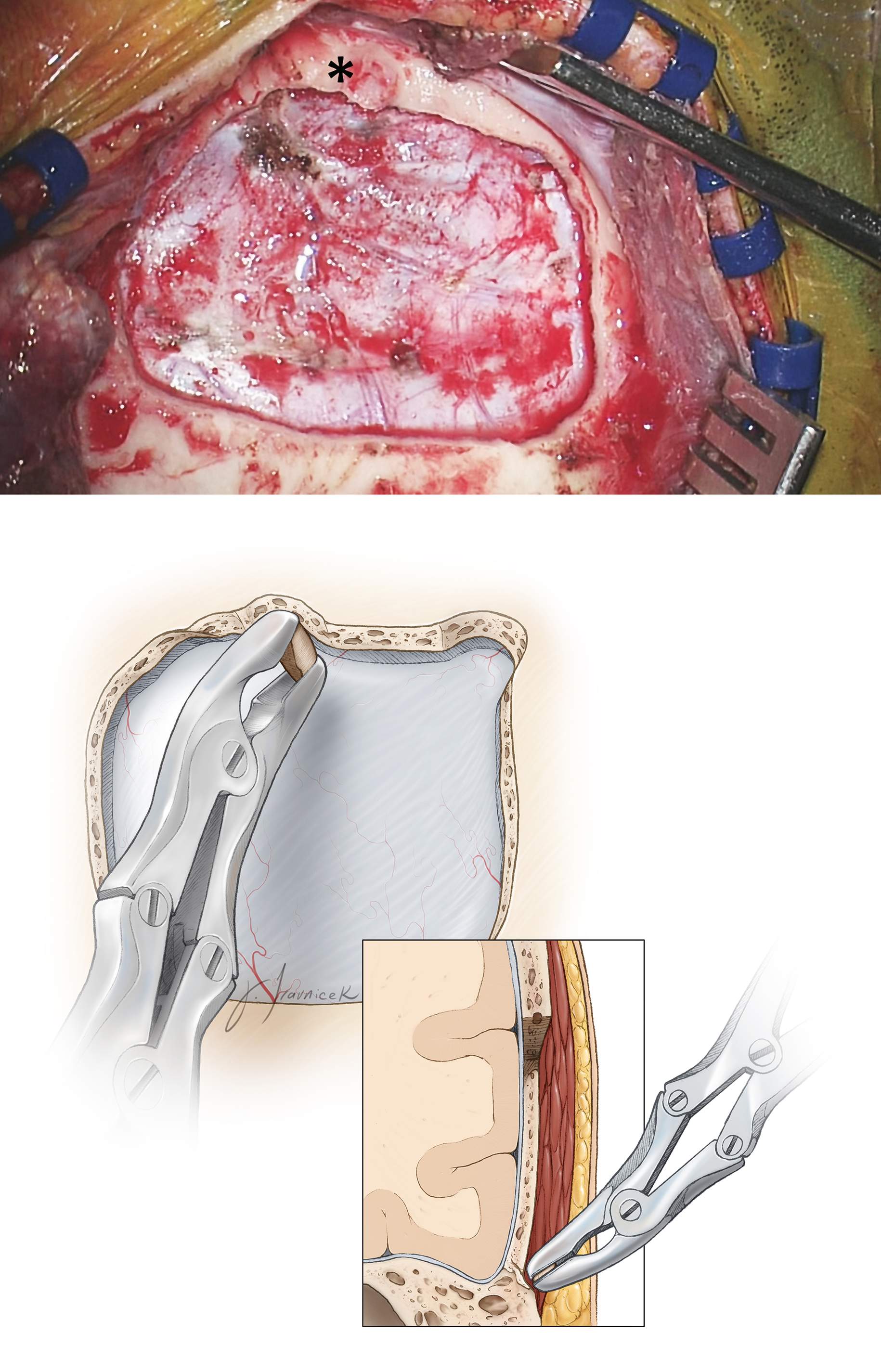
Figure 6: The craniotomy in relation to the root of zygoma (*) is evident (top). Most often, the inferior edge of the craniotomy leaves a strip of overhanging bone, obscuring a clear operative path toward the middle fossa floor. Subsequently, a Leksell rongeur may be used to remove this overhanging bone until the edge of the craniotomy is at the level of the floor (bottom). A handheld drill further assists with this task.
Figure 7: Removal of the overhanging bone over the inferior craniotomy will allow an unobstructed view of the middle fossa floor, minimizing the need for temporal lobe retraction. The location of the root zygoma (*) is marked. The temporal bone and mastoid air cells are thoroughly waxed to prevent development of a postoperative CSF fistula (arrows). Dural Tack up sutures are placed.
Alternatively, an extradural dissection along the middle fossa may be resumed for skull base lesions. Importantly, the location of the vein of Labbe should be estimated preoperatively. The dural opening and extradural temporal lobe elevation should be adjusted for protection of this vital venous structure. Additional CSF may be released through the lumbar drain to further relax the lobe.
Please refer to the Anterior Pterosectomy chapter for further steps regarding extradural middle fossa dissection and petrosal osteotomy.
Extradural Middle Fossa Dissection and Anterior Petrosal Approach
Extended Subtemporal Transtentorial Approach to the Ventrolateral Upper Brainstem
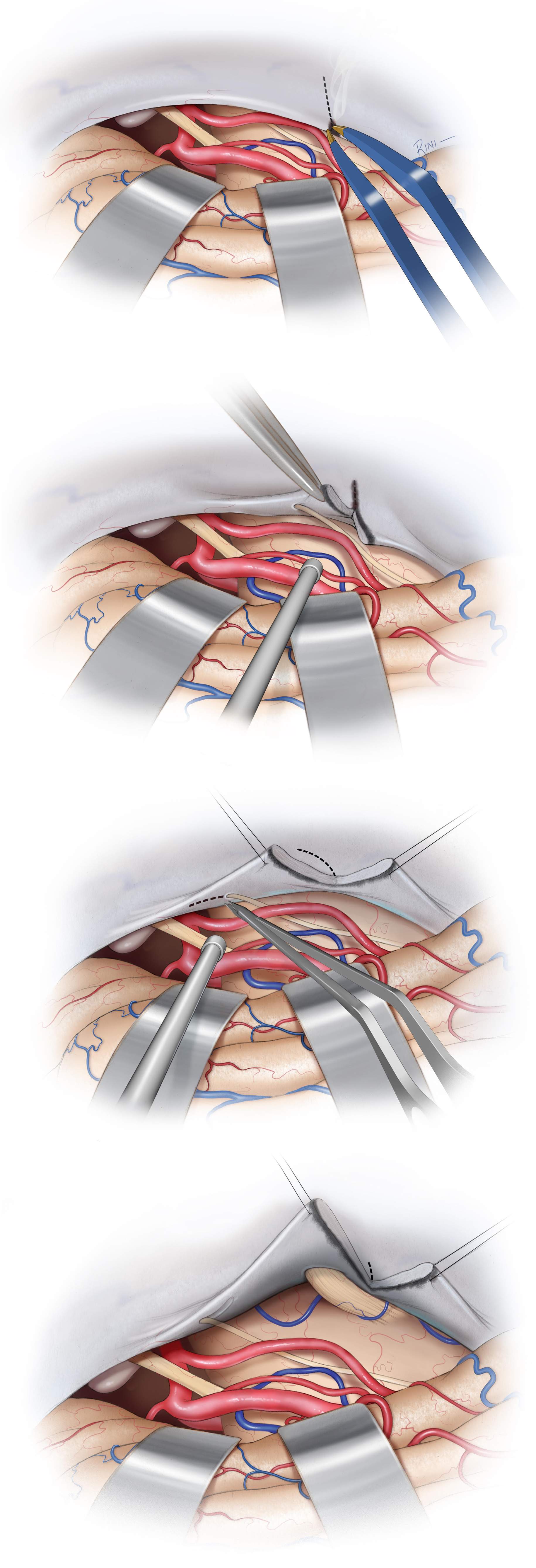
This expansion of the subtemporal approach towards the ventrolateral brainstem is especially worthwhile and should be employed when neccessay to replace more radical skull base approaches such as an anterior petrosectomy. The following two key steps allow anterolateral reflection of the medial tentorial flap:
- dissection of the trochlear nerve from its dural canal up to its entrance in the cavernous sinus and
- extension of the tentorial incision up to the Meckel's cave.
Two retraction sutures are placed along the tentorium to mobilize it effectively. With fine microscissors, the medial border of the dural canal of the trochlear nerve is opened. The nerve is not adherent within the canal and a microdissector is used to gently mobilize it from the rest of the canal and towards the brainstem. The tentorial incision is continued and oriented toward the superior petrosal sinus at the area just over the entrance of the trigeminal nerve into the Meckel's cave. The mean distance from the trochlear nerve’s entrance in its dural tunnel to its entrance into the cavernous sinus is about 8 mm (range, 3.4-14.9 mm; standard deviation, 3.9 mm).
With this technique, the trochlear nerve is free of the tentorial flap, creating a supra- and infratrochlear working window. If the tentorial incision is extended to the most lateral aspect of the Meckel's cave, the root of the trigeminal nerve and the anterior inferior cerebellar artery (AICA) origin can be seen.
Figure 9: This above modified technique of tentorial incision and reflection maximizes the subtemporal transtentorial exposure and operative maneuverability by increasing the rostrocaudal and anterolateral exposure without permanent postoperative trochlear nerve deficit. The following steps are described: 1) retraction or reflection of the tentorial edge to identify where the CN IVth enters its dural canal, 2) coagulation of the tentorial edge and its incision starts between both retraction sutures (top row) Again, the dural entry point of the nerve is carefully protected (second row), 3) dissection of the trochlear nerve free of its dural canal for a short distance, and 4) incision of the tentorium is continued and oriented toward the superior petrosal sinus and dissection of the trochlear nerve’s dural canal continues forward (third row). Depending on the degree of anterolateral retraction needed for optimal exposure, the tentorial incision can stop at the edge of the petrosal sinus, extended across the petrosal sinus, or into the roof of Meckel's cave (last row). Anterolateral reflection of the anterior triangular tentorial flap, with the trochlear nerve fully dissected out of its tunnel at the tentorial edge, results in supra- and infratrochlear working windows.
Closure
In the presence of air cells, I prefer a watertight dural closure primarily or secondarily using a piece of dural allograft. Adipose tissue with its globular texture is one of the best barriers against CSF leakage. In the case of subtemporal skull base exposures that require removal of the tumor-infiltrated dura and bone, strips of adipose tissue are placed across the dural opening to seal the dural defect. Before placement of the adipose grafts, all air cells must be meticulously waxed.
Alternatively, a vascularized muscle flap prepared from the posterior aspect of the temporalis muscle may be rotated to fill the defect within the bone or dura. This latter method is used during repeat operations for patients who have previously undergone radiation treatment.
Any additional mastoid and temporal air cell are rewaxed. Finally, the bone flap is replaced and the scalp is closed in anatomic layers.
Postoperative Considerations
Postoperatively, the patient is admitted to the ICU for neurologic and blood pressure monitoring and pain control. Frequent and careful neurologic exams are paramount because temporal lobe hematomas can occur due to lobar retraction injury or venous drainage compromise, leading to rapid brainstem compression.
The patient is usually transferred to the regular ward on the first or second postoperative day. Lumbar drainage may be continued if there is a high suspicion of CSF leakage. Due to manipulation of the temporal lobe, the use of prophylactic antiepileptic medications for at least one week after surgery is highly recommended.
Pearls and Pitfalls
- During positioning, tilting the patient’s head toward the floor is a key maneuver to maximize the use of gravity retraction and obtain appropriate subtemporal exposure.
- The upper edge of the zygoma is a good landmark for locating the level of the middle fossa floor.
- Removal of the overhanging inferior edge of the craniotomy is important for preparing an obstructed operative trajectory toward the middle fossa floor.
- The location of the vein of Labbe should be estimated preoperatively. Dural opening and extradural temporal lobe elevation should be adjusted for protection of this vital venous structure.
References
Apuzzo. M, Brain Surgery: Complication Avoidance and Management, Volume 1. Churchill Livingstone, 1983.
Campero A, Tróccoli G, Martins C, Fernandez-Miranda JC, Yasuda A, Rhoton AL Jr. Microsurgical approaches to the medial temporal region: An anatomical study. Neurosurgery. 2006;59(Suppl 2)S279-308.
Rhoton AL Jr. The cerebral veins. Neurosurgery. 2002;51(Suppl 4)S159-205.
Please login to post a comment.