General Principles Free
Figure 1: Harvey Cushing demonstrates creation of a trephine craniotomy at the upper edge of frontal bone work. Note the use of tourniquet to control scalp bleeding.
This Cranial Approaches volume provides a road map regarding the indications, rationale, and technical nuances for execution of common supratentorial and infratentorial operative corridors. Although the skull base osteotomies will be discussed in the Skull Base Surgery volume within the Skull Base Exposures section, these osteotomies are also included in this volume.
My personal philosophy for reaching appropriate exposure is based on the following principles:
- The ideal approach protects normal cerebrovascular structures and allows efficient and thorough handling of the lesion. The technical complexity of the approach is secondary in importance.
- The operator should avoid a routine and overzealous use of a limited number of approaches. Instead, one should tailor the approach to the underlying target.
- The most important priorities for selection of the operative corridor are:
a. Strict protection of normal anatomy and
b. maximal and efficient exposure of the lesion without operative blind spots. - The operation is not about how to get there, rather it is about what to do when you are there. This means that the surgeon must minimize the complexity of the approach and instead choose the most efficient and unobstructed route to reach the lesion. Once there, the surgeon spends most of the time and effort on protecting normal anatomy while dealing with the pathology.
- The normal structures, pathology, and ultimately the surgeon’s experience affect the trajectory of the approach.
- Extensive skull base osteotomies such as petrosal approaches have important but a limited use in cranial surgery. Careful patient selection and their judicious use are strongly advised.
The advantages and drawbacks of every approach should be clearly defined. The familiarity of the surgeon with a particular approach should not be the sole confounding factor to determine the choice of approach; rather the surgeon should accumulate experience with every operative corridor and its modifications.
After the 1) bony approach is determined, the next step is the selection of the 2) intradural trajectories or routes to expose the lesion. The surgeon should remain inventive and original by exploring techniques and methods to protect the normal anatomy. The following algorithm defines my strategy for design of pertinent intradural trajectories:
The dissection via the intradural trajectory to reach the lesion must minimize extraneous brain injuries and transgression through proper planning of the operative approach and patient positioning. Gravity retraction, enhanced bony removal, brain relaxation, wide arachnoid dissection, and most importantly, strategic use of dynamic retraction and handling of the normal brain during manipulation of the surgical target are key factors in successful operative planning.
For example, the supraorbital craniotomy is a lateral skull base approach suitable to access the parasellar, parachiasmatic, and intrasylvian spaces. This approach allows minimal brain retraction, an important consideration for reaching deep lesions, especially pathologies underneath the dominant hemisphere. When modified through the removal of the orbital roof, intraorbital and large parachiasmatic tumors become readily accessible via this approach.
When combined with an eyebrow incision, the supraorbital craniotomy is a minimally invasive keyhole approach. When compared with the standard pterional lateral subfrontal exposure, the more anterior trajectory of the supraorbital subfrontal corridor affords a longer operative working distance, but potentially is associated with less brain manipulation and retraction. The use of dynamic retraction through the strategic use of suction apparatus and dissectors gives the supraorbital subfrontal route flexible working angles and adequate operative space for managing complex lesions, including anterior circulation aneurysms and large anterior skull base tumors.
We often underestimate the function of the basal frontal lobes during subfrontal operations. The orbitofrontal and mediobasal cortices are often misleadingly considered ‘silent’ and noneloquent. However, their functions are apparent to the patients’ families and coworkers, especially when the patient is high functioning. Subfrontal injury frequently leads to loss of inhibition caused by damaging the orbitofrontal region, which is involved in cognitive processing and decision-making. For more information, please see Wikipedia.
Supratentorial Approaches and Routes
The pterional craniotomy and its modifications are the workhorses of the supratentorial approaches. An extended form of pterional craniotomy through aggressive resection of the sphenoid wing and orbital roof is a skull base approach and mimics orbitozygomatic osteotomy.
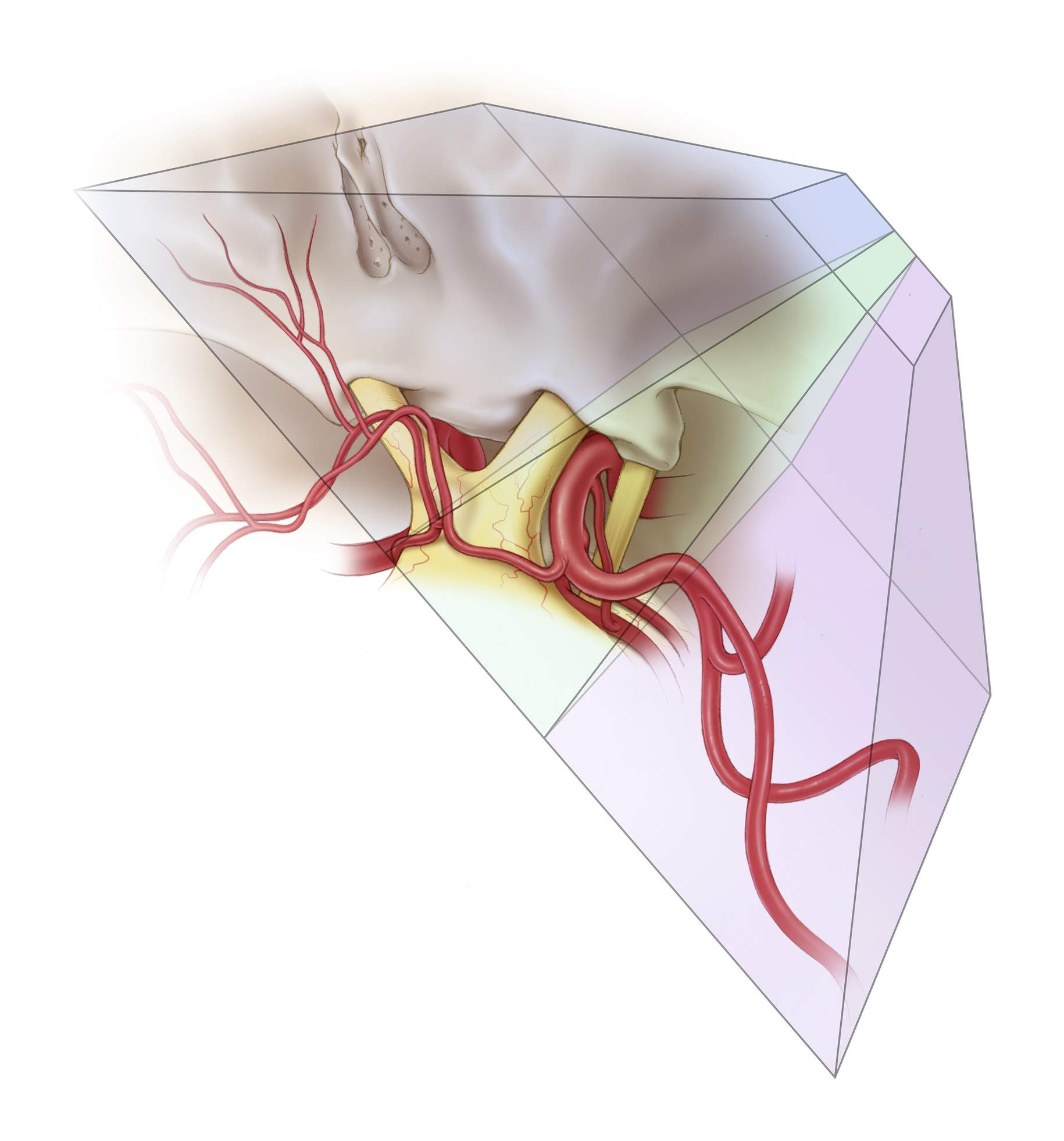
Figure 2: I often visualize the ideal exposure to handle the lesion and then work backwards to compromise and find safe approaches and trajectories to the lesion. Before the intradural work, I also routinely conceptualize the final appearance of the operative field after resection and accelerate my maneuvers to achieve the final result. As demonstrated with this illustration, I conceive the three-dimensional anatomy of vital structures (ie optic nerve, etc) at the depth of the dissection and then plan my approach for the adjacent abnormality.
Figure 3: I define the operative trajectories based on specific arachnoidal dissection planes and gentle mobilization of the neighboring brain. In this illustration, the three trajectories for the subfrontal approach are defined. Based on the desired trajectory, the operative maneuvers are designed.
Figure 4: Roadmaps help me conceptualize the operative trajectory. The images above demonstrate the dissection routes for reaching middle cerebral and anterior communicating artery aneurysms.
Infratentorial Approaches
Figure 5: The operative corridors and trajectories for accessing the cerebellopontine angle are illustrated. The surgical corridors for reaching lesions above the cranial nerve (CN) VII/VIII complex (supralateral cerebellar route: blue arrow) and below the CN VII/VIII complex (infralateral cerebellar or infrafloccular route: green arrow) are shown.
Figure 6: The trajectory of operative dissection for the telovelar approach in relation to the tonsils, vermis, and medial aspect of the cerebellar hemispheres is indicated in this illustration.
Figure 7: The areas of exposure (green) for the pterional, orbitozygomatic, and subtemporal cranial approaches are illustrated.
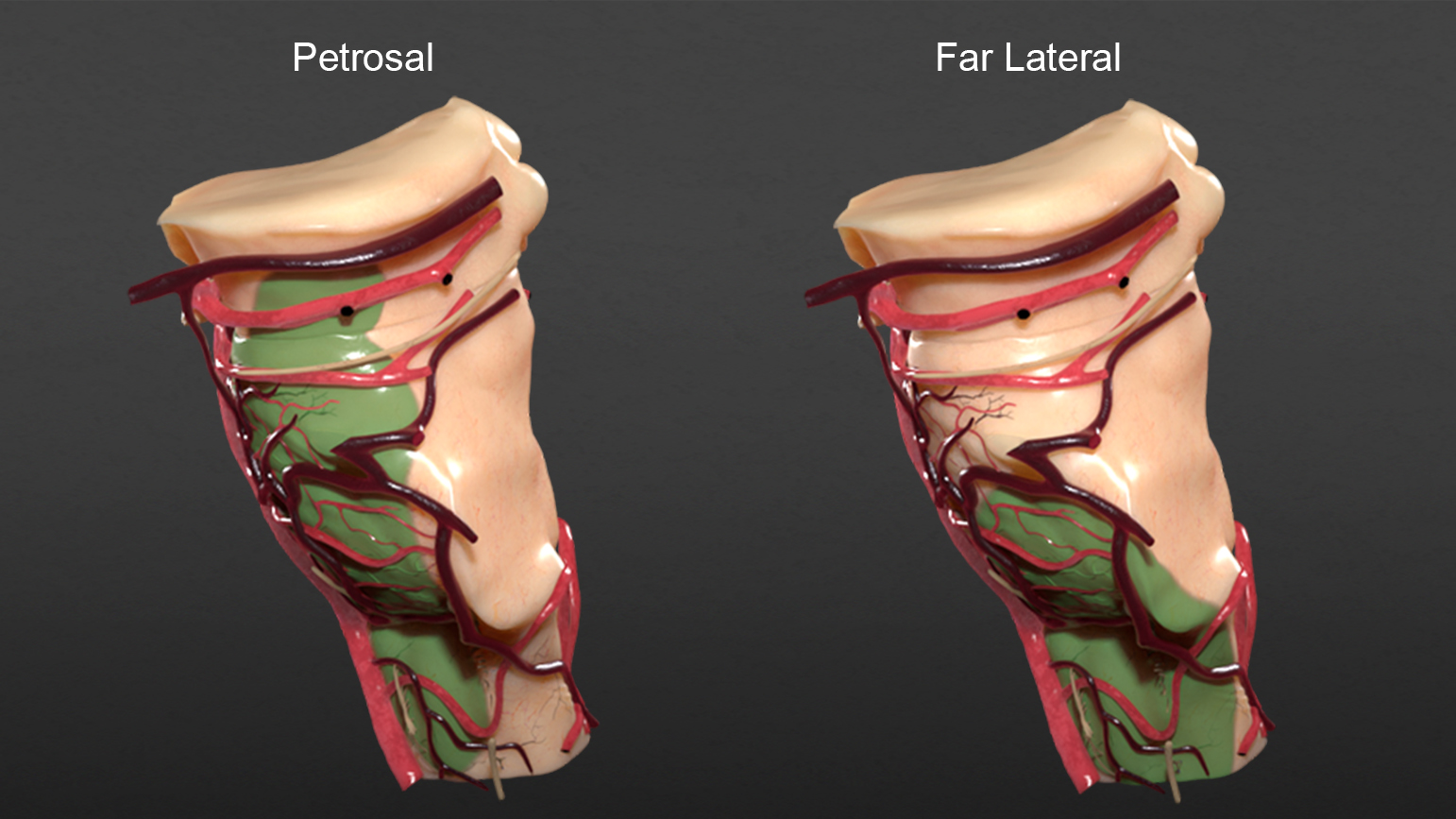
Figure 8: The areas of exposure (green) for the petrosal and far lateral cranial approaches are illustrated.
Figure 9: The areas of exposure (green) for the retrosigmoid and suboccipital cranial approaches are illustrated.
Figure 10: The areas of exposure (green) for midline and lateral supracerebellar infratentorial cranial approaches are illustrated.
Figure 11: A comparison of the different approaches and their associated areas of exposure are detailed in these illustrations.
Ultimately, it is the surgeon’s experience that affects the limitations of the approach and the operative trajectory. We are all comfortable with a certain volume of lesional exposure when we proceed with microsurgical dissection.
The use of dynamic retraction limits the exposure of the entire lesion at one time but reveals just enough of the necessary portion of the lesion at each step of dissection. One has to feel comfortable with such segmented or step-wise exposure. In return, dynamic retraction obviates the need for extensive cranial openings and brain retraction or transgression that are often associated with higher degree of postoperative morbidity.
As I have gained experience in my career, I have been able to accomplish more with less exposure. My confidence has grown to the point where I realize that I can manage disastrous intraoperative events with just enough space. The definition of just enough is difficult to determine, but it is related to one’s operative experience and skill.
Another turning point in my career was the development of a tailored concept in accordance with each patient needs. Minimally invasive keyhole and tailored approaches are also discussed where appropriate, since I believe the operator should be intimately familiar with all modifications of the exposures, as well as their advantages and limitations.
Finally, the operative working angles are more important than the operative working space. The use of flexible operative working angles obviates the need for expanded operative spaces that lead to aggressive handling of the overlying normal structures. These principles are portrayed through the use of the endoscopic transnasal approaches.
I want to thank you for your interest in exploring my operative philosophy for cranial approaches.
Please login to post a comment.






















Comments: