Transcallosal Interforniceal Approach
This is a preview. Check to see if you have access to the full video. Check access
Resection of a Large Hemorrhagic Colloid Cyst via the Transcallosal Interforniceal Approach
Indications for the Approach and Preoperative Considerations
The interforniceal approach is a variation of the transcallosal route and involves working between the columns of fornix (within the interforniceal raphe) to reach the third ventricle. I do not use this approach unless the interforniceal raphe is expanded in the presence of a cavum septum pellucidum or tumor. The associated risks of disconnecting and dissecting the normally fused forniceal bodies away from each other are significant. In my opinion, because other routes are not available, these risks are not justified.
Figure 1: Magnetic resonance images demonstrate a large hemorrhagic colloid cyst. The presence of cavum septum pellucidum creates a potential space within the interforniceal raphe, facilitating the use of the interforniceal route.
Operative Anatomy
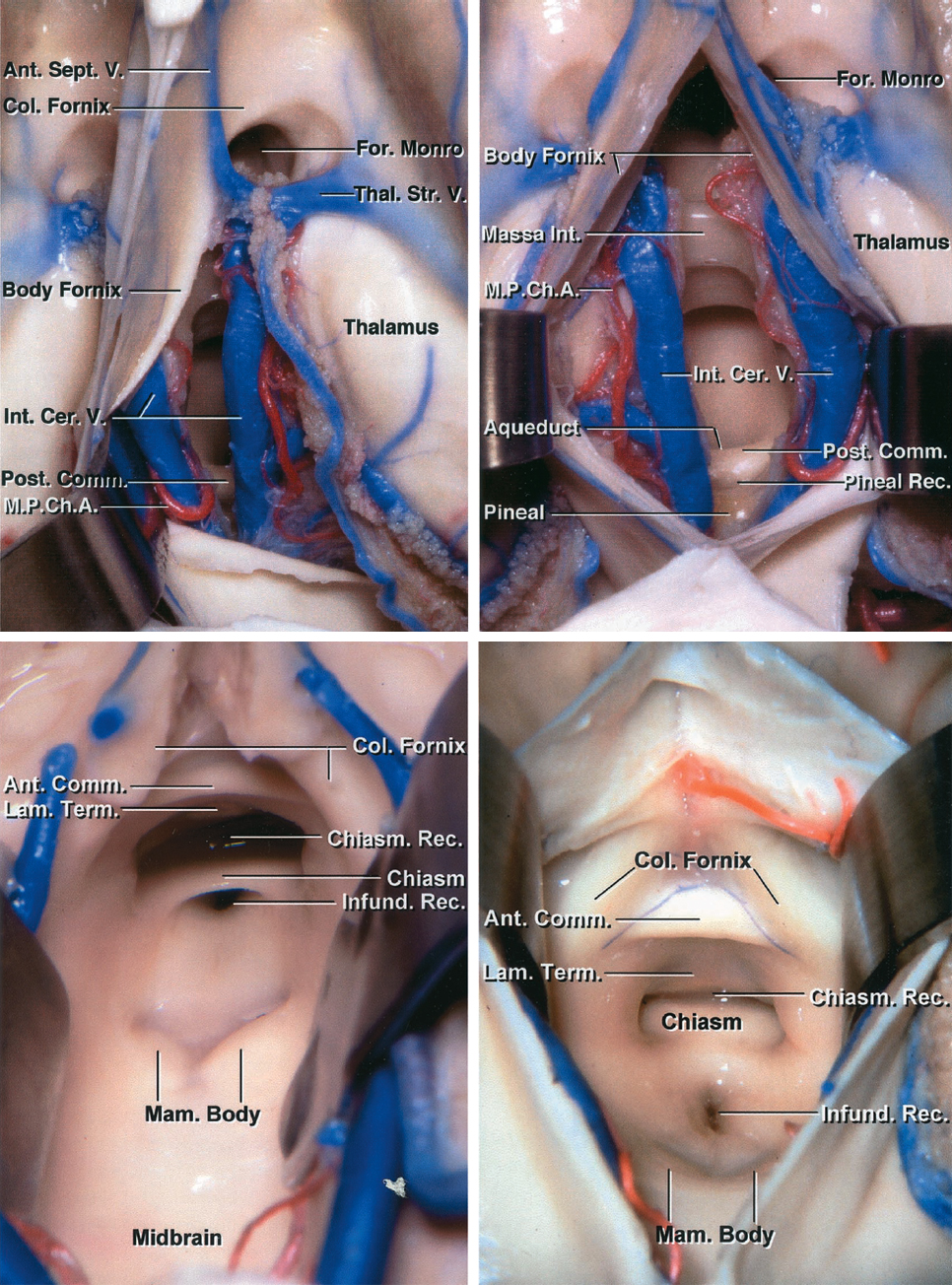
The interforniceal approach minimizes the expanse of the operative blind spots as a midline lesion is exposed via a midline route.
Click here to view the interactive module and related content for this image.
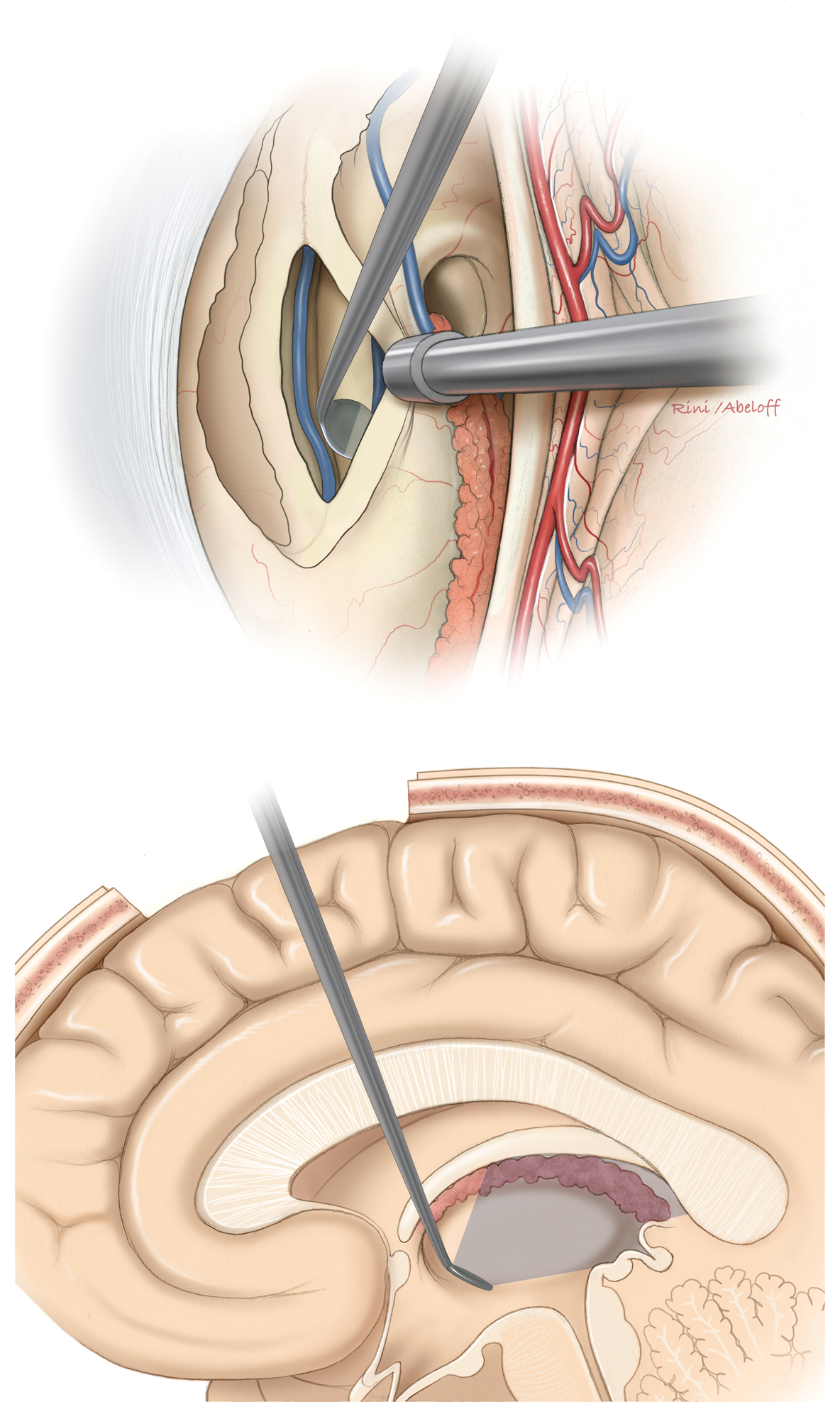
Figure 2: Transchoroidal and interforniceal dissections are demonstrated (upper row).Note the more encompassing exposure of the interforniceal approach with wide disclosure of the internal cerebral veins and the floor of the third ventricle. The lower images further identify relevant anatomical structures on the floor. This wide exposure is possible at the expense of potential injury to both forniceal bodies. The highly vulnerable internal cerebral veins should not be retracted aggressively.
TRANSCALLOSAL INTERFORNICEAL APPROACH
The interforniceal approach can be performed with the patient’s head in the neutral or lateral position (the sagittal suture parallel to the floor). For the initial stages of the operation including the exposure and transcallosal entry, please refer to the chapters on Interhemispheric Craniotomy and Lateral Ventricular Tumors.
INTRADURAL PROCEDURE
The trajectory of the transcallosal dissection should target the interforniceal raphe. The following illustrations demonstrate the operative trajectory with the patient's head in the supine position. I typically place the head in the lateral position to utilize gravity retraction.
Figure 3: Upon entering the right lateral ventricle, first, septum pellucidum is coagulated/reduced to the level of the dorsal surface of the fornices. Next, I dissect the columns of fornix along their raphe; the tumor is usually immediately encountered. Often, the tumor creates a natural separation plane between the forniceal bodies. The junction of the septum pellucidum and fornices provides the landmark for the raphe.
Figure 4: The interforniceal and transforaminal pathway(s) may be all utilized for resection of large tumors.
Figure 5: The unilateral versus bilventricular corridors can be accessed based on the size and the location of the bulk of the tumor. Manipulation of the tumor via unilateral or bilateral foramina of Monroe is possible.
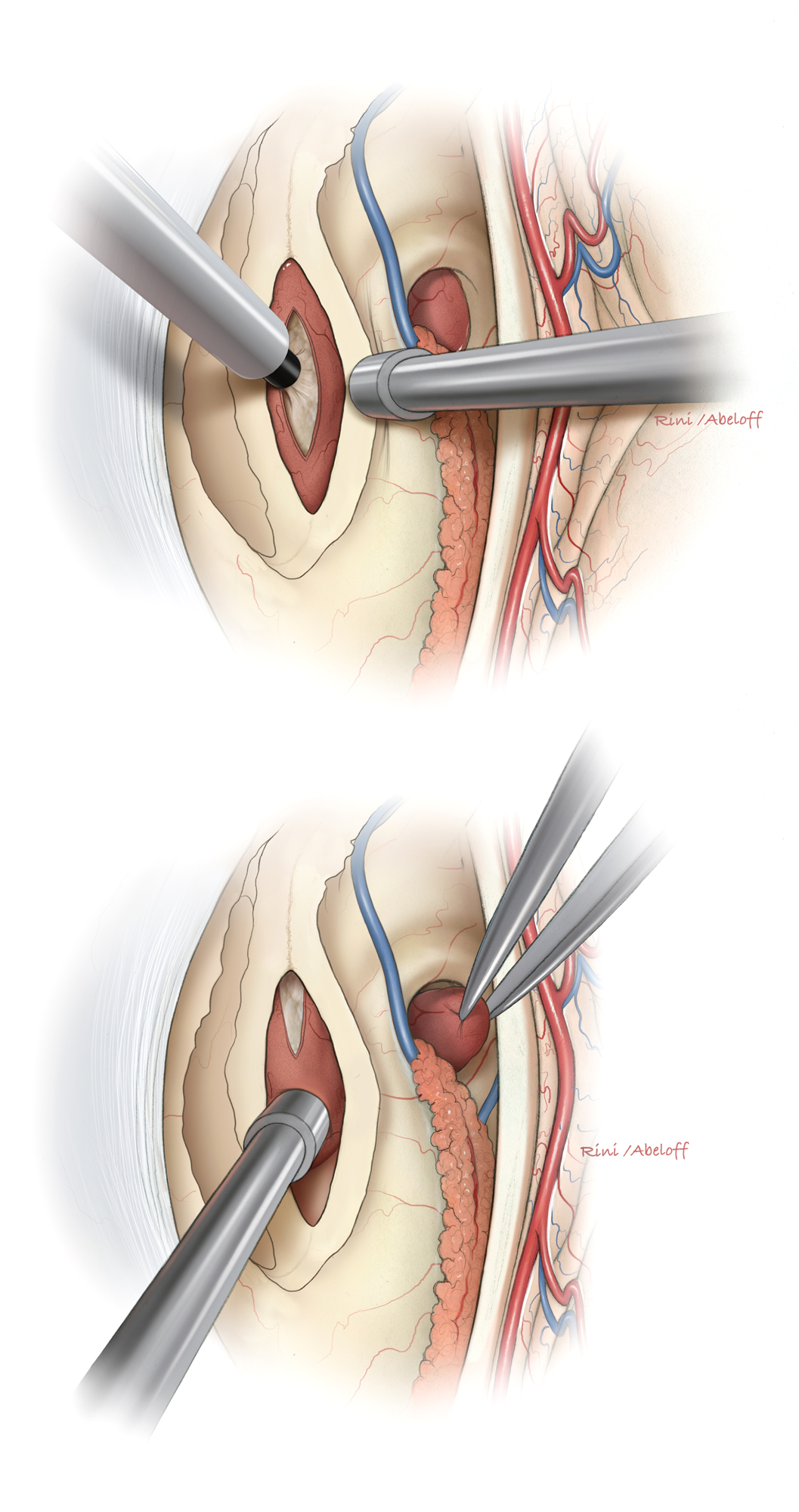
Figure 6: The forniceal bodies are gently mobilized over the capsule of the tumor (top). The exposure of the raphe starts at the level of the foramen of Monroe and extends 2 cm posteriorly. Next, the capsule is entered for internal decompression of the tumor bulk (bottom).
Figure 7: The ultrasonic aspirator is needed to remove the tumor without placing the vital surrounding structures including the walls of the third ventricle under undue traction (top). The enlarged foramen of Monroe may be accessed for removing the anterior pole of the tumor (bottom).
Figure 8: The tumor is cautiously separated from the internal cerebral veins (top). An angled micromirror (dental mirror) can expand the viewing angles and reveal/inspect the posterosuperior space within the third ventricle (the operative blind spot)(bottom).
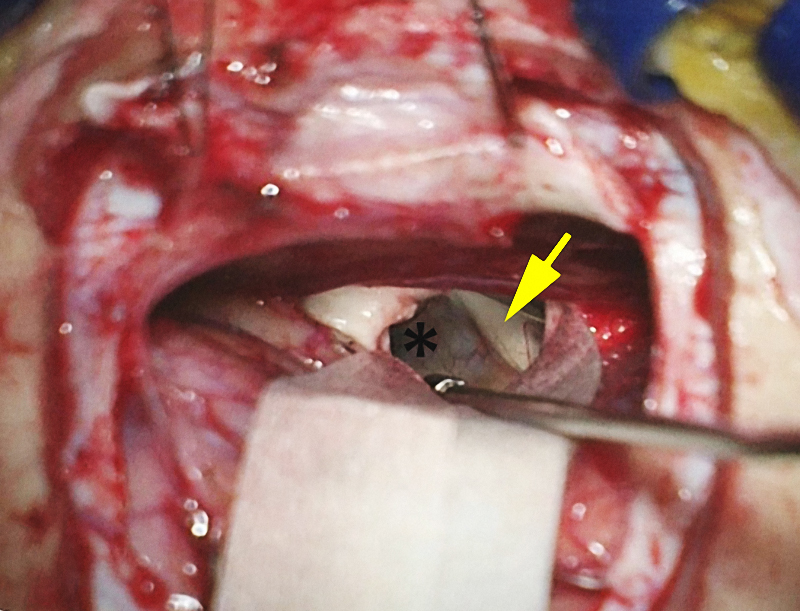
Figure 9: A small right frontal craniotomy and interhemispheric approach were completed for the tumor depicted in Figure 1. The patient’s head is in the lateral position with the right side “down.” The lateral position may lead to novice operator’s disorientation in regard to the anatomic landmarks that demarcate the operative corridor.
Figure 10: A small 1.5-2.0cm callosotomy immediately discloses the grayish capsule of the tumor through the generous cavum septum pellucidum and expanded interforniceal raphe. The left fornix is marked with an arrow. This natural separation of the forniceal columns is important for safe use of the interforniceal corridor.
Once I land in the right lateral ventricle, I enter the cavum and find the raphe. If the septal leaves are fused, I attempt to find a small potential space between them. If this is not feasible, I reduce the septum to the level of the forniceal bodies using bipolar electrocoagulation and then expand the raphe using sharp microinstruments.
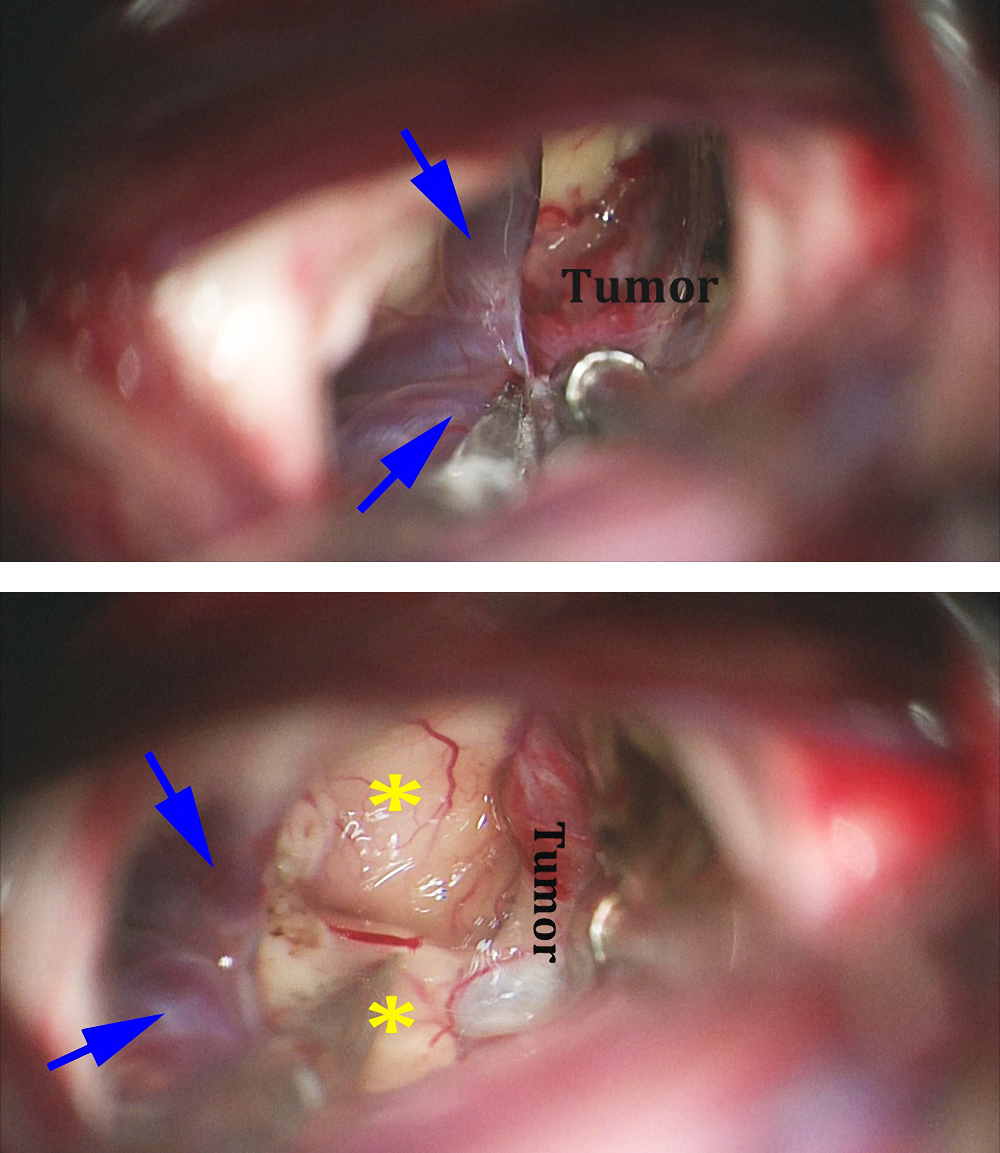
Figure 11: A higher magnified view of the operative corridor (compared with the one in Figure 4) through the cavum discloses the left fornix (yellow arrow) and the capsule of the tumor through the interforniceal raphe (at the tip of bipolar forceps).
Figure 12: The internal cerebral veins (blue arrows) are separated using microscissors so that the posterior capsule of the tumor can be exposed (top image). This maneuver allows identification of the posterior third ventricular wall (*) and the posterior capsule of the cyst (lower photo).
Finally, the capsule is delivered en bloc. Minimal manipulation of the fornices is key to success.
If aggressive separation of the fused forniceal bodies is attempted, this separation should occur within the 1.5–2.0cm distance posterior to the foramen of Monro to minimize deleterious effects on memory. The hippocampal commissures are posterior to this limit and should be identified and protected.
Postoperative Considerations
Short-term memory difficulties are not unusual after the above approach. These deficits are likely to disappear within 3-6 months postoperatively. Postoperative neuropsychological therapy is advised.
Pearls and Pitfalls
- There are limited indications for the use of the interforniceal approach. I use this trajectory if the interforniceal raphe is expanded in the presence of a cavum septum pellucidum or by the tumor.
Please login to post a comment.