Peritorcular Meningioma
This is a preview. Check to see if you have access to the full video. Check access
Resection of a Peritorcular Meningioma
Torcular meningiomas arise from the wall of the torcular Herophili, the site of confluence of the superior sagittal, straight, occipital, and both transverse sinuses. On the other hand, peritorcular meningiomas originate from the neighboring dural structures and secondarily grow into the torcular region, sparing the patency of he torcula.
Meningiomas associated with the torcular herophili present considerable surgical challenges because of their relationships to structures involved in the principal venous drainage systems of the bilateral hemispheres. Hyperostosis in the region of the internal occipital protuberance and en plaque extension of tumor along the venous sinuses is not unlikely.
These tumors are fortunately very rare and account for less than 1% of all intracranial meningiomas. With careful patient selection and detailed preoperative assessment, surgical risks can be minimized.
Meticulous surgical technique is mandatory when working in the vicinity of the dural venous sinuses and central venous structures, given the requirement for patency of venous outflow and the risk of life-threatening intraoperative bleeding. The surgeon, of course, wants to achieve complete resection, but in these cases, complete resection is accompanied by the risk of neurologic devastation from disruption of the dominant venous drainage. Fortunately, adequate tumor control can be achieved after surgery with modern radiosurgical intervention for small residual tumors.
Diagnosis
Peritorcular meningiomas tend to present similarly to falcotentorial meningiomas, but they often also cause obstruction of the posterior superior sagittal sinus, adding an additional etiology for raised intracranial pressure.
Occipital lobe (visual field defects and seizures) or cerebellar (ataxia) dysfunction may result from direct compression by the tumor or from regional venous hypertension.
Evaluation
The patient’s functional status, age, comorbidities, and life expectancy are important considerations when determining the time of intervention. Because the natural history of meningiomas is variable, it is important to establish the lesion’s growth rate in asymptomatic or minimally symptomatic cases to determine the appropriateness of intervention.
Given the potential for significant blood loss during tumor resection or sinus reconstruction, the possible need for blood transfusion should be discussed with the patient, and the patient’s beliefs about the use of blood products should be addressed. If sinus reconstruction is contemplated, the safety of antiplatelet agents and heparin therapy should be evaluated in light of the patient’s medical history.
Proximity to the visual cortex and operative risk from retraction injury necessitates preoperative visual acuity and visual field assessment. The patient and family should be made aware of the risk of transient or permanent hemianopia if unilateral approaches are used, and of the risk of cortical blindness with bilateral occipital approaches.
Preoperative MR imaging is used during frameless stereotaxy. T2-weighted sequences can provide information about anatomic relationships to the pineal gland, internal cerebral veins, thalamus, splenium of the corpus callosum, and occipital lobes.
Assessment of the venous anatomy in relation to the tumor is further supplemented with a MR venogram. If resection or reconstruction of the straight sinus, transverse sinus, or torcula is contemplated in very rare cases, a preoperative cerebral angiography to assess the dural sinuses, venous collaterals, and arterial supply to the tumor is warranted.
The vascular supply for these lesions is variable and may include the meningohypophyseal trunk, meningeal branches of the external carotid artery, meningeal branches of the ascending pharyngeal artery, branches of the medial and lateral posterior choroidal artery, the posterior cerebral artery, and the meningeal branches of the vertebral artery.
Figure 1: A large peritorcular meningioma is noted. This patient could not undergo MR imaging because of the presence of a ferromagnetic foreign body. CT angiogram demonstrated occlusion of posterior sagittal and transverse sinuses as well as the torcula (top row of images). Anteroposterior and lateral angiogram images (bottom row of images) revealed tumor arterial supply from the petrosquamosal divisions of the middle meningeal arteries bilaterally. There was complete occlusion of the superior sagittal sinus at the level of the parietal lobe with venous outflow from the superior sagittal sinus into bilateral dural and scalp veins as well as into the parietal cortical veins. There was some patency of the straight sinus into the torcula which drained via a right paramedian emissary vein. There was prominence of the precentral cerebellar and supravermian veins, raising the possibility of retrograde flow from the straight sinus and vein of Galen into the supravermian veins. Note the hypertrophied osseous collateral venous channels within the posterior fossa (blue arrow); these were protected during the craniotomy. The vein of Trolard was also very prominent (black arrow).
Classification
Torcular meningiomas may be classified according to their involvement with the dural venous sinus walls and the extent of sinus occlusion. Although no formal classification system is widely used, close attention is given to the extent of sinus wall involvement and the degree of sinus occlusion (partial <50%; partial >50%; or complete).
Tumors in which collateral venous drainage has developed from complete sinus occlusion and in which no sinus venous hypertension exists can be considered for complete tumor/sinus excision without reconstruction. However, partially occluded sinuses must be preserved, either by proceeding with a conservative strategy of subtotal resection followed by watchful waiting or stereotactic radiosurgery, or alternatively by sinus wall resection and reconstruction (not recommended).
The tumors that are superior to the vein of Galen arise within the pericallosal cistern and acquire a thick arachnoid covering as they invaginate into the quadrigeminal cistern, which permits complete removal of these tumors from the adjacent vein of Galen. However, tumors that lie below the vein of Galen may not benefit from the same separation planes.
Indications for Procedure
Surgical resection is indicated for patients who have enlarging tumors causing progressive neurologic deficit and who are medically fit for surgery. If the patient is older than 65, calcified tumors that are not growing should be observed with serial imaging because these are less likely to grow and cause symptoms of mass effect.
If the patient has significant medical comorbidities and is high risk for a major surgical procedure, symptomatic hydrocephalus related to venous outflow obstruction by a torcular meningioma may be alleviated by ventriculoperitoneal shunting without addressing the tumor directly.
Preoperative Considerations
All patients in whom an attempt at complete torcular meningioma resection is entertained with or without a consideration for sinus reconstruction should undergo preoperative cerebral angiography to define the patency of major dural venous sinuses and collateral venous drainage systems. Angiography allows the most accurate assessment of the degree of occlusion of the straight sinus, torcula, and transverse sinus.
In some patients with substantial dural sinus stenosis or occlusion, significant transosseous and scalp drainage may be the only source of collateral venous drainage. Therefore, the scalp flap and craniotomy should be tailored to preserve these only-primary venous collaterals. For example, if the straight sinus is occluded, important collateral venous drainage through tentorial channels parallel to the straight sinus may exist. It is important to preoperatively identify this collateral drainage system so that the tentorium can be divided laterally to these vital indispensable collaterals during the occipital transtentorial approach to these tumors.
Operative Anatomy
The torcula represents the junction of the superior sagittal sinus with the transverse sinuses and straight sinus. Typically, the dominant transverse sinus is on the right. Variations in sinus anatomy occur in which the superior sagittal sinus may be duplicated or split into one separate supply vessel into each of the transverse sinuses. The location of the torcula is directly deep to the external occipital protuberance.
Figure 2: The relationship of the torcula to the occipital protuberance on the sagittal plane is shown (left image). To expose the torcula, I drill perpendicular to the oblique surface of the skull at this location. The junction of the dural sinuses (superior sagittal, transverse, and straight sinuses) is also demonstrated via mobilization of the right hemisphere (right image). The straight sinus often has numerous venous lakes at its periphery; these lakes can be a serious source of bleeding during surgery and should be packed with thrombin-soaked gelfoam and not coagulated. (Images courtesy of AL Rhoton, Jr.)
Click here to view the interactive module and related content for this image.
Figure 3: The relevant neurovascular anatomy of the incisura is noted. The relationship of the tumor to the deep venous system is critical for preservation of the diencephalic veins. The arachnoid planes are life-saving when protecting function and avoiding venous infarction. (Images courtesy of AL Rhoton, Jr.)
Click here to view the interactive module and related content for this image.
Figure 4: The deep venous system from a superior view (left image) and inferior view (right image) is shown in detail. Venous injury is one of the primary sources of morbidity during meningioma resection in the region. (Images courtesy of AL Rhoton, Jr.)
RESECTION OF TORCULAR MENINGIOMA
The patient is placed in the three-quarters prone position to avoid raised venous pressure from the chest and abdominal compression and to reduce the risk of air embolism. The head is slightly elevated about 15 degrees in relation to the floor. The head is turned approximately 60 degrees toward the floor. The torcular quadrant where most of the tumor is situated is placed at the summit of the operative field.
Figure 5: Patient positioning is illustrated. The skin is taped so that the shoulder is mobilized anteroinferiorly. This maneuver is important to prevent obstruction of the operative field. The skin incision, generous number of burr holes and relationship of the tumor to the surrounding structures are also demonstrated.
I have a low threshold for using precordial Doppler ultrasonography and transesophageal echocardiography for resection of tumors associated with the major dural venous sinuses. A central line is also placed to deal with venous air embolism. Importantly, a low level of suspicion for venous air embolism during the procedure is warranted.
I use a lumbar drain to decompress the dual sac early in surgery. This maneuver allows effective mobilization of the adherent dura from the inner surface of the skull, especially in the area of the dural venous sinuses (the craniotomy often encompasses the posterior superior sagittal/transverse sinuses, as well as the torcula.)
I do not recommend the use of visual evoked potentials because these potentials are unreliable, altered depending on the anesthetic used, and difficult to record.
Frameless stereotaxy may be used to identify the extent of the tumor along the transverse and superior sagittal sinuses in order to plan the skin incision and craniotomy. A U-shaped flap is usually used, with the base along the patient’s neck and a horizontal limb centered on the midline above the superior aspect of the tumor.
Unilateral tumors extending along the tentorium may require a “hockey-stick” incision that crosses the midline. The extent of peritorcular exposure depends on the peritorcular quadrants containing the tumor and on the tumor's geometry. A unilateral occipital craniotomy may be adequate for single quadrant tumors when the sacrifice of a torcular component is not a consideration. The tumors that extend through the tentorium can be removed via an occipital craniotomy and transtentorial approach.
Exposure of the torcula can be accomplished by making multiple burr holes on the transverse sinus and two burr holes, one on each side of the superior sagittal sinus beyond the superior extent of the tumor. The dural sinuses are carefully reflected off the bone flap before elevating the flap.
Bone wax and ample gelfoam powder soaked in thrombin solution should be readily available during the placement of burr holes and elevation of the bone flap; meticulous hemostasis must be maintained. If the tumor invades into the bone so that safe elevation of the bone flap in a single piece might be impossible or unsafe, thinning of the adjacent bone with a round burr drill and Kerrison rongeurs is advised to safely access the tumor.
I recommend a wide craniotomy supra- and infratentorially (based on the extent of the tumor) on each side of the superior sagittal sinus. This exposure allows for occipital and parietal lobe mobilization without untoward retraction on the corresponding cortices and by the dural edge. Adequate exposure is also desired for controlling venous bleeding.
The dural leaflets are incised in a cruciate fashion and subsequently elevated toward the superior sagittal sinus and transverse sinus above the tentorium, and based over the transverse sinus infratentorially. All parasagittal veins are meticulously preserved. The dural incisions must be about 1 to 2 cm away from the edge of the tumor, exposing a strip of the brain at the periphery of the craniotomy. Posterior falcine and tentorial divisions are performed early in surgery to disrupt the blood supply to the tumor.
Upon elevation of the bone flap, there is usually a high risk of sudden venous bleeding. The surgical team must be ready to control this bleeding episode and minimize the risk of venous air embolism. The patient’s head may be only slightly elevated during the process of bone flap elevation.
I typically cover the entire surface of the dura with a wet sponge immediately after elevation of the bone. Next, I systematically control the different bleeding sites by mobilizing the sponge along its different corners in a stepwise fashion. As mentioned previously, the risk of massive sudden blood loss is significant in these cases, and the surgeon and anesthesiologist should work closely together under these circumstances and be prepared.
Figure 6: Dural opening is tailored to the tumor's size, tumor's extent within the supra- versus infratentorial compartments, and involvement of the major venous sinuses. A generous exposure of the surrounding normal brain is mandatory to minimize the risk of untoward forces on the normal cerebrovascular structures and working within operative blind spots. The major parasagittal bridging veins must be protected to avoid venous infarction.
INTRADURAL PROCEDURE
After dural opening, some tumor debulking may be necessary to accomplish the division of the falx and the affected section of the tentorium. Before tumor decompression starts, I devascularize the tumor along its base as much as is safely possible. Cerebrospinal fluid drainage via the lumbar drain is quite effective for allowing early tumor mobilization and exposure of the tumor base.
Hemostasis is secured at one location before the surgeon diverts his or her attention to a different dissection location.
The tumor is debulked with preservation of the functional posterior superior sagittal sinus draining veins. In some cases, the large posterior draining veins may wrap around and between the lobules of the tumor like vines on a trellis. Meticulous sharp dissection is required, and if the veins are adherent to the tumor surface or dive into the tumor lobule, resection may have to be near gross total or subtotal in that region.
Figure 7: After devascularization of the tumor from its base on the falx and tentorium, I work above and below the tentorium to maximize tumor removal. Retractor blades act as "protectors" on the occipital lobes. Any adherent tumor on the calcarine cortices is left behind to avoid the risk of blindness. As expected, the patterns of dural opening and maneuvers for tumor resection are highly dependent on the extent of the tumor bulk.
The initial steps involve disconnection of the tumor from its attachments and tumor debulking. Occluded dural sinuses are handled at the later stages of the operation. The tumor is enucleated centrally to allow direct visualization of the tumor-brain interface and thereby permitting sharp dissection of the arachnoid planes. The underlying brain is protected with soft cotton patties during dissection.
Even barely patent posterior superior sagittal sinus should not be occluded or resected given the associated risk of cerebral edema and venous infarction. Although revascularization of the venous sinuses can be accomplished with autologous tissue such as the internal saphenous vein or external jugular vein, this maneuver is high risk and not advised. Resection of the barely patent transverse sinus with reconstruction is also controversial for similar reasons.
I have opted for an adaptive nonaggressive approach to resection of dural sinuses given the control that can be achieved with microsurgical resection combined with postoperative radiosurgery.
After tumor devascularization, and its extensive debulking and dissection from the neurovascular structures, including the occipital lobes, the affected falx, and tentorium, are divided, and the occluded dural sinuses are ligated, isolated, and removed. Invariably, some tumor is left behind within the adjacent patent dural sinuses and will be the source of future recurrence. As mentioned previously, any cortical draining vein anterior to the tumor and leading to the patent section of the superior sagittal sinus should be preserved. If the tumor has invaded the visual cortex, a rim of the tumor should be left behind because any manipulation of the adherent tumor capsule in the region will lead to blindness.
Figure 8: The completely occluded sections of the major dural venous sinuses can be ligated and an en bloc removal accomplished. Note the clip ligation of the vein of Galen. Such an aggressive resection requires preoperative confirmation of total occlusion of the involved venous structures including the straight sinus.
I do not believe temporary clamping of the dural venous sinuses and measurement of their intraluminal pressure proximal to the blockage can provide reliable information about the safety of their permanent occlusion.
The occipital sinus is dispensable unless it has become a hypertrophied collateral of an obstructed transverse sinus. In this role, it carries substantial venous flow from the superior sagittal or straight sinus into the jugular bulb.
Management of Tumors Associated with the Dural Venous Sinus
The safety of tumor resection near the dural sinus is determined by the degree of the involvement of the tumor with the sinus. I previously discussed the nuances for removal of the occluded transverse sinus as long as the origin of the vein of Labbé (laterally) and the patent torcula (medially) are protected. Obviously, one must preserve the dominant venous drainage system of the hemispheres.
If the tumor abuts the sinus wall, one usually can peel the tumor away from the wall of the dural sinus. If a small portion of the sinus is partially filled with tumor, the extrasinusal portion of the tumor is truncated and the intrasinusal component dealt with separately. I usually am able to gently dislodge the tumor fragment out of the sinus lumen and repair the defect in the sinus wall using 6-0 sutures. The walls of the sinus may be temporarily collapsed via gentle pressure for proximal and distal control during suturing.
If a substantial portion of the sinus is involved with the tumor or both walls of the sinus are affected but the sinus lumen remains functional, removal of the sinus and its reconstruction is not warranted because of safety concerns.
Case Example
A 42 year-old female presented with visual dysfunction and was found to suffer from a large peritorcular meningioma. Please see the preoperative images in Figure 1.
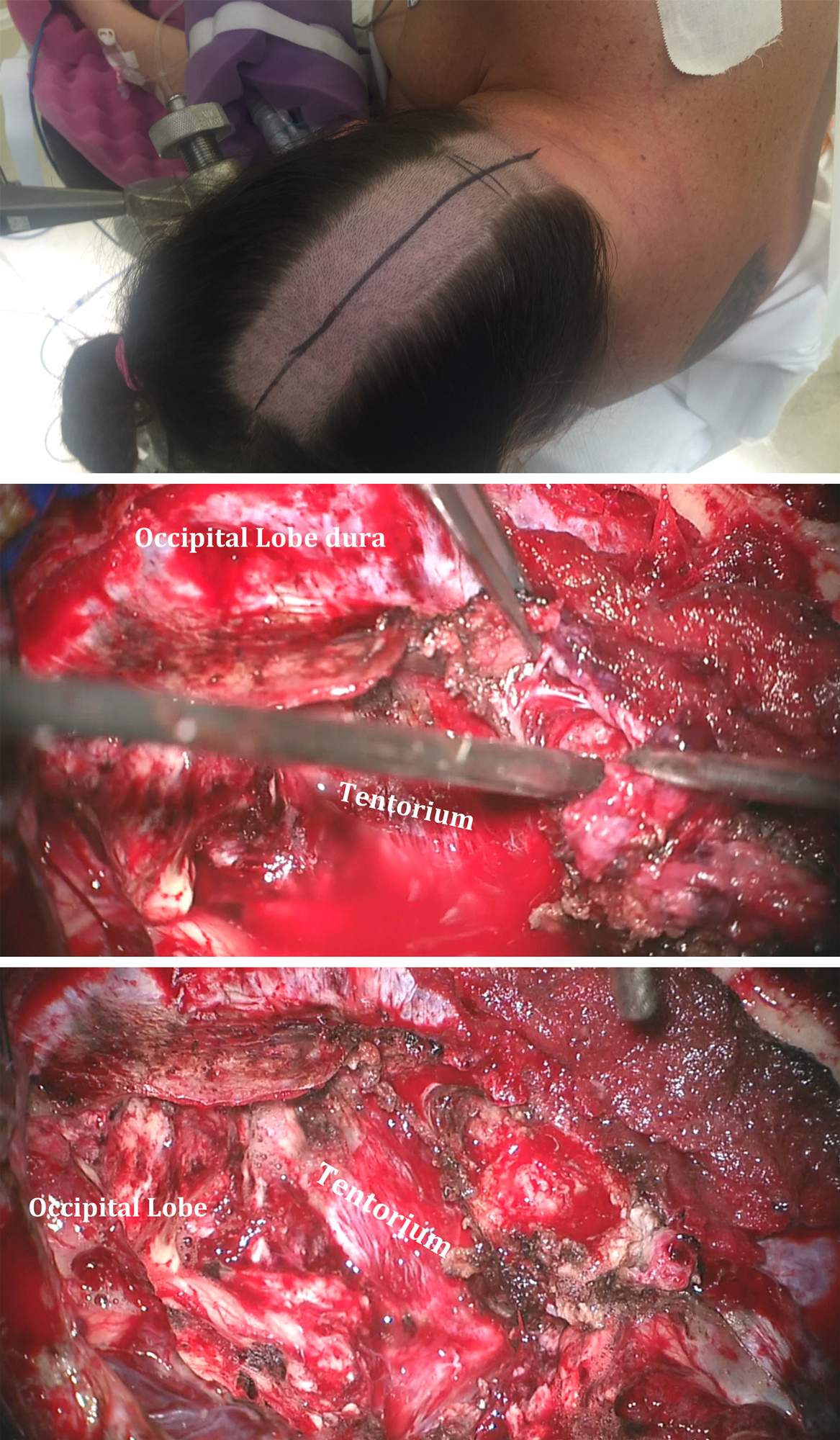
Figure 9: Note the head positioning in the top image. A lumbar drain was used in this case. After removal of the majority of the tumor, the easily deliverable part of the tumor within the right transverse sinus was extracted (middle image). The occluded dural venous sinuses were not ligated and removed in this case because I did not want to interrupt the osseous collateral venous drainage of the posterior fossa. The final result of resection is demonstrated in the bottom image.
Closure and Postoperative Care
Dural closure is completed using an autologous section of pericranium. Skin closure is performed with running nylon sutures. Staples on the posterior scalp catch on bed sheets and are uncomfortable for the patient to lie on.
The risk of pseudomeningocele formation is significant because of the large potential space created after resection of these typically giant tumors. The lumbar drain is left in place at the end of the procedure and for 48 hours after surgery, drained at 8 cc/hour.
Pearls and Pitfalls
- Aggressive surgery with sinus reconstruction is not advised.
- Appropriate measures for controlling intraoperative bleeding and dealing with sudden blood loss are important for torcular meningioma surgery.
Contributors: Roberto Jose Diaz, MD, PhD, FRCSC, Simon Buttrick, MD, Ricardo J. Komotar, MD
References
Asari S, Maeshiro T, Tomita S, Kawauchi M, Yabuno N, Kinugasa K, et al. Meningiomas arising from the falcotentorial junction. Clinical features, neuroimaging studies, and surgical treatment. J Neurosurg. 1995; 82:726-738.
Ausman JI, Malik GM, Dujovny M, Mann R. Three-quarter prone approach to the pineal-tentorial region. Surg Neurol. 1988; 29:298-306.
Bassiouni H, Asgari S, Konig HJ, Stolke D. Meningiomas of the falcotentorial junction: selection of the surgical approach according to the tumor type. Surg Neurol. 2008;69:339-349; discussion 349.
DiMeco F, Li KW, Casali C, Ciceri E, Giombini S, Filippini G, et al. Meningiomas invading the superior sagittal sinus: surgical experience in 108 cases. Neurosurgery. 2004;55:1263-1272; discussion 1272-1264.
Goto T, Ohata K, Morino M, Takami T, Tsuyuguchi N, Nishio A, et al. Falcotentorial meningioma: surgical outcome in 14 patients. J Neurosurg. 2006;104:47-53.
Hasegawa M, Yamashita J, Yamashima T. Anatomical variations of the straight sinus on magnetic resonance imaging in the infratentorial supracerebellar approach to pineal region tumors. Surg Neurol. 1991;36:354-359.
Kobayashi S, Sugita K, Tanaka Y, Kyoshima K. Infratentorial approach to the pineal region in the prone position: Concorde position. Technical note. J Neurosurg. 1983; 58:141-143.
Mantovani A, Di Maio S, Ferreira MJ, Sekhar LN. Management of meningiomas invading the major dural venous sinuses: operative technique, results, and potential benefit for higher grade tumors. World Neurosurg. 2014;82:455-467.
Mathiesen T, Pettersson-Segerlind J, Kihlstrom L, Ulfarsson E. Meningiomas engaging major venous sinuses. World Neurosurg. 2014;81:116-124.
Nadkarni TD, Menon RK, Desai KI, Goel A. Spontaneous cerebrospinal fluid rhinorrhea following excision of a massive torcular meningioma. J Clin Neurosci. 2006;13:118-121.
Odake G. Meningioma of the falcotentorial region: report of two cases and literature review of occlusion of the galenic system. Neurosurgery. 1992;30:788-793; discussion 793-784.
Okami N, Kawamata T, Hori T, Takakura K. Surgical treatment of falcotentorial meningioma. J Clin Neurosci. 2001;8(Suppl 1):15-18, 2001
Quinones-Hinojosa A, Chang EF, McDermott MW. Falcotentorial meningiomas. clinical, neuroimaging, and surgical features in six patients. Neurosurg Focus. 2003;14:e11.
Raco A, Agrillo A, Ruggeri A, Gagliardi FM, Cantore G. Surgical options in the management of falcotentorial meningiomas. report of 13 cases. Surg Neurol. 2004;61.157-164; discussion 164.
Sekhar LN, Goel A. Combined supratentorial and infratentorial approach to large pineal-region meningioma. Surg Neurol. 1992;37:197-201.
Sindou M. Meningiomas invading the sagittal or transverse sinuses, resection with venous reconstruction. J Clin Neurosci. 2001;8(Suppl 1);8-11.
Sindou M. Meningiomas involving major dural sinuses: should we attempt at radical removal and venous repair? World Neurosurg. 2014; 81.46-47.
Sindou M, Hallacq P. Venous reconstruction in surgery of meningiomas invading the sagittal and transverse sinuses. Skull Base Surg. 1998; 8:57-64.
Suzuki M, Sobata E, Hatanaka M, Suzuki S, Iwabuchi T, Makiguchi K. Total removal of a falcotentorial junction meningioma by biparietooccipital craniotomy in the sea lion position: a case report. Neurosurgery. 1984; 15:710-714.
Please login to post a comment.