Atypical and Malignant Meningiomas
Figure 1: This AM demonstrates some characteristics of lower-grade meningioma, including calcification on CT imaging (top left), but on bone algorithm CT imaging, permeative bony infiltration can be seen (top right). This is a finding suggestive of a higher-grade tumor. Most lower-grade meningiomas tend to exhibit underlying hyperostosis. Axial FLAIR imaging (bottom left) demonstrates vasogenic edema associated with the medial left parietal mass, presumably due to irritative parenchymal invasion or venous stasis, given the invasion of this AM into the superior sagittal sinus, as seen on sagittal T1-weighted postcontrast imaging (bottom right).
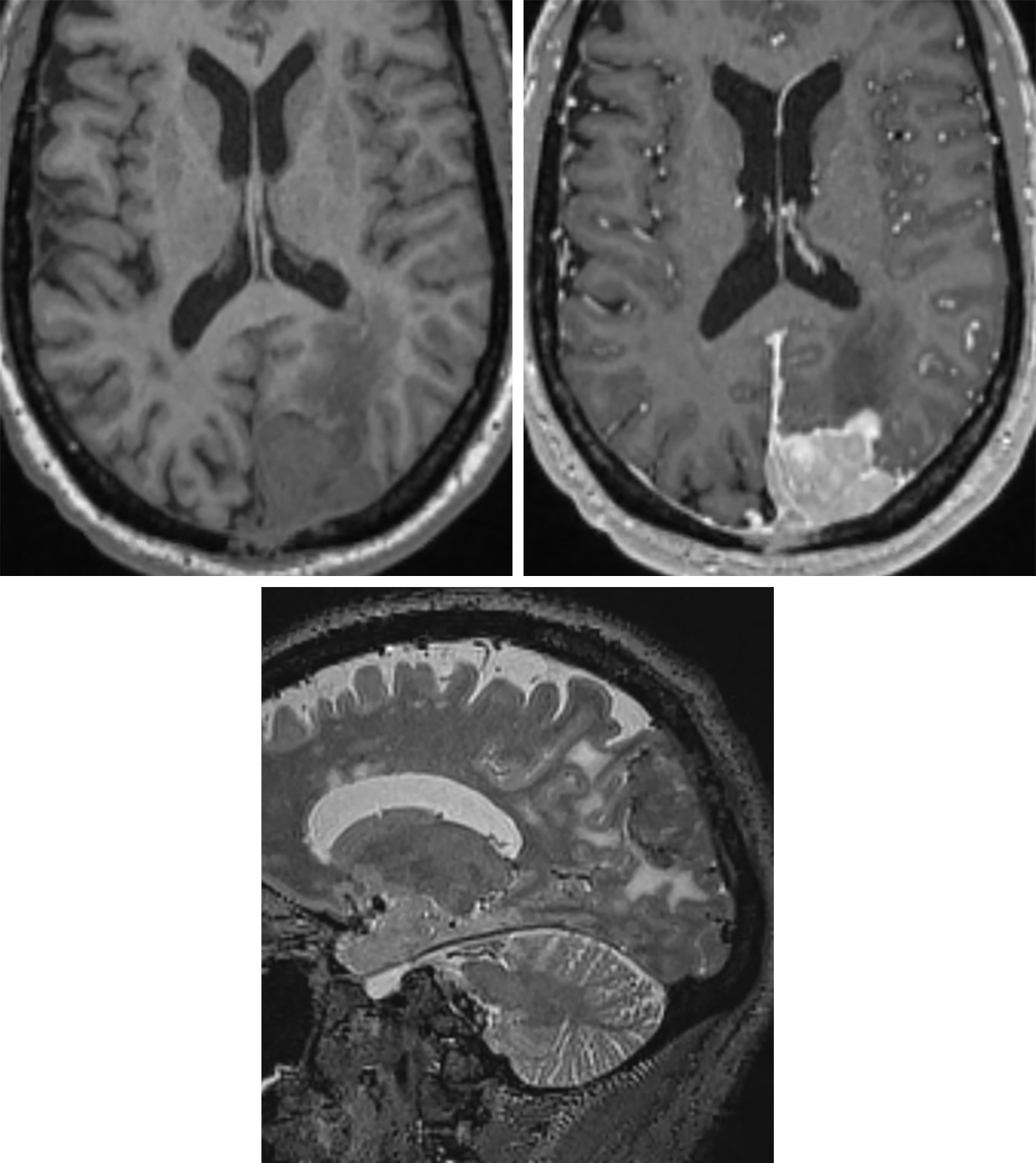
Figure 2: (Top Right) Thought more difficult to see on T1-weighted axial imaging, this left parieto-occipital convexity MM demonstrates bright enhancement on postcontrast T1-weighted imaging. The irregular contour is more typical of MM than of benign meningioma. (Bottom) Sagittal T2-weighted imaging also demonstrates hyperintense surrounding edema, a feature that is often seen in benign meningioma but should also raise suspicion for a higher-grade lesion.
Figure 3: (Top Left) This MM demonstrates extensive involvement of the skull base and surrounding structures, particularly on postcontrast T1-weighted imaging, where there is encasement of the brightly enhancing carotid arteries and extension through the sella, suprasellar cistern, left middle cranial fossa, and left orbit. (Top Right) Sagittal postcontrast imaging also illustrates how extensive the tumor is, with involvement of the left occipital condyle and extension into the posterior fossa. Significant mass effect on the inferior left frontal lobe can also be seen. (Middle Left) Axial FLAIR imaging shows this mass mildly infiltrating the left cerebellar hemisphere, in addition to skull base, masticator space, and orbital involvement. DWI and ADC (middle right and bottom) show mild restriction, a characteristic common to both benign and malignant meningiomas.
BASIC DESCRIPTION
- Anaplastic, aggressive extra-axial tumors arising from malignant degeneration of typical meningiomas (TMs)
PATHOLOGY
- WHO grade II (atypical meningioma [AM]) and grade III (malignant meningioma [MM])
- Most likely arise from dedifferentiation of TMs
- Increased mitoses, nucleus-to-cytoplasm ratio, necrosis, and nuclear atypia compared to TMs
- Sarcomatous degeneration, rapid growth, and invasion of brain parenchyma in MMs
- AMs account for <3% of all meningiomas
- MMs are uncommon
CLINICAL FEATURES
- Adults are most commonly afflicted (usually at a younger age than with TMs)
- Slight female gender predilection
- Treatment: surgical resection including adjacent bone; presurgical embolization; radiation
- Higher recurrence rates (MM > AM >> TM)
IMAGING
- General
- Dura-based, extra-axial mass with necrosis, invasion of adjacent brain, and extensive peritumoral brain edema
- May arise at any location within the neuraxis
- AMs: cerebellopontine angle (CPA) cistern, tentorium most common
- MM: parasagittal or cerebral convexity
- Skull base and spine less commonly affected than with TMs
- Invasion and destruction of adjacent bone
- CT
- Ill-defined, hyperdense mass extending intracranially and extracranially
- Minimal calcification compared to TMs
- Extensive hypodense peritumoral edema
- Avid enhancement on contrast-enhanced CT imaging
- MRI
- T1WI: variable signal intensity, often poorly defined tumor margins
- T2WI: variable signal intensity
- FLAIR: often marked hyperintense peritumoral edema
- DWI: reduced diffusivity (bright DWI, dark ADC)
- T1WI+C: avid enhancement with enhancing margins invading adjacent structures
- MR venography (MRV): evaluate patency and involvement of dural venous sinuses
- MRS: elevated alanine at short echo times (TEs) (1.3–1.5 ppm)
IMAGING RECOMMENDATIONS
- MRI without and with intravenous contrast; MRV for dural sinus patency
For more information, please see the corresponding chapter in Radiopaedia.
Contributor: Rachel Seltman, MD
References
Cao X, Hao S, Wu Z, et al. Survival rates, prognostic factors and treatment of anaplastic meningiomas. J Clin Neurosci 2015;22:828–823. doi.org/10.1016/j.jocn.2014.11.022.
Moradi A, Semnani V, Djam H, et al. Pathodiagnostic parameters for meningioma grading. J Clin Neurosci 2008;15:1370–1375. doi.org/10.1016/j.jocn.2007.12.005.
Nagar VA, Ye JR, Ng WH, et al. Diffusion-weighted MR imaging: diagnosing atypical or malignant meningiomas and detecting tumor dedifferentiation. AJNR Am J Neuroradiol 2008;29:1147–1152. doi.org/10.3174/ajnr.A0996.
Osborn AG, Salzman KL, Jhaveri MD. Diagnostic Imaging (3rd ed). Elsevier, Philadelphia, PA; 2016.
Please login to post a comment.