Supraorbital Craniotomy
This is a preview. Check to see if you have access to the full video. Check access
Eyebrow Incision and Supraorbital Craniotomy: dAVF Disconnection
General Considerations
The supraorbital craniotomy is a lateral skull base approach suitable to access the parasellar, parachiasmatic and intrasylvian space. This approach attempts to minimize brain retraction, an important consideration for surgeons attempting to reach deep lesions, especially underneath the dominant hemisphere. When combined with removal of the orbital roof, intraorbital tumors become readily accessible via this approach.
When combined with an eyebrow incision, the supraorbital craniotomy is a minimally invasive keyhole approach. This concept of a keyhole approach has gained special popularity. Several authors have described various modifications of the conventional frontal and frontotemporal approaches, creating some confusion. Variations of the subfrontal route can be referred to as supraorbital, eyebrow supraorbital, frontolateral, supraciliary frontolateral keyhole, lateral supraorbital, and several other combinations.
When compared with the standard pterional lateral subfrontal exposure, the more anterior trajectory of the supraorbital subfrontal corridor affords a longer operative working distance, but potentially requires less brain manipulation and retraction. The use of dynamic retraction through the strategic use of suction apparatus and dissectors bestows the supraorbital subfrontal route flexible working angles for managing complex lesions, including anterior circulation aneurysms and large anterior skull base tumors.
Figure 1: This anatomical dissection demonstrates the most frequently used minimally invasive anterolateral approaches to the anterior cranial fossa and parasellar spaces. Substantial overlap among these exposures is apparent. The frontolateral approach is distinguished from the supraorbital route by its subtle rotation towards the sphenoid wing. Green: supraorbital approach; Orange: lateral supraorbital approach; Red: minipterional approach; Blue: pterional approach (Modified with permission, courtesy of AL Rhoton, Jr.)
We often underestimate the function of the basal frontal lobes during subfrontal operations. The orbitofrontal and mediobasal cortices are often misleadingly considered ‘silent’ and ‘noneloquent.’ However, their functions are apparent to the patients’ families and coworkers, especially when the patient is high functioning. Subfrontal injury frequently leads to disinhibition caused by damaging the orbitofrontal region, which is involved in cognitive processing and decision-making (see Wikipedia).
Mediobasal injury leads to anterograde and retrograde amnesia. These deficits are not apparent to the treating neurosurgeon, but readily detectable on a neuropsychological examination.
Extraneous frontal lobe injuries can be avoided with proper planning of the operative approach and patient positioning to use gravity retraction, enhanced bony removal, brain relaxation, wide arachnoid dissection and most importantly, strategic use of dynamic retraction and handling of the normal brain during manipulation of the pathology.
Indications for the Approach
A supraorbital craniotomy is used for large (<5cm) anterior skull base tumors such as olfactory groove, planum sphenoidale, and tuberculum sella meningiomas, as well as vascular lesions such as anteriorly and inferiorly pointing anterior communicating artery (A-Comm) and common ophthalmic aneurysms. Parasellar tumors such as craniopharyngiomas are also ideal candidates for this approach. However, more posteriorly situated lesions with significant cranial extensions are not suitable for this approach due to the limited vertical reach of this corridor.
Appropriately selected small lesions within the mid to medial anterior Sylvian fissure (such as small middle cerebral artery aneurysms) and the interpeduncular space (small tumors) are also reasonable contenders for this approach. The long working distance to these targets restricts the working angles needed to manipulate large tumors or complex aneurysms.
This is a slightly increased risk of cosmetic concerns associated with the eye-brow incision. Patients with sparse eye-brows should consider traditional pterional routes. Moreover, tumors along the sphenoid wing and extending into the middle fossa are best approached through the traditional corridors.
Preoperative Considerations
Preoperative tumor embolization may help minimize blood loss; however, I hardly ever use this method for meningiomas because the craniotomy allows tumor devascularization along the anterior skull base. Preoperative scans should be reviewed to assess the lateral extent of the frontal sinus and the potential to avoid its entry. If this sinus is entered, the mucosa must be removed and the cavity packed with muscle and bone wax. A pericranial flap harvested during the exposure can be preserved and used to cover the frontal sinus opening.
The basal cisterns may be difficult to reach early in the surgery without significant retraction of a tense frontal lobe. Therefore, a lumbar drain may be used for patients who have associated lesional edema and expected increased intracranial tension.
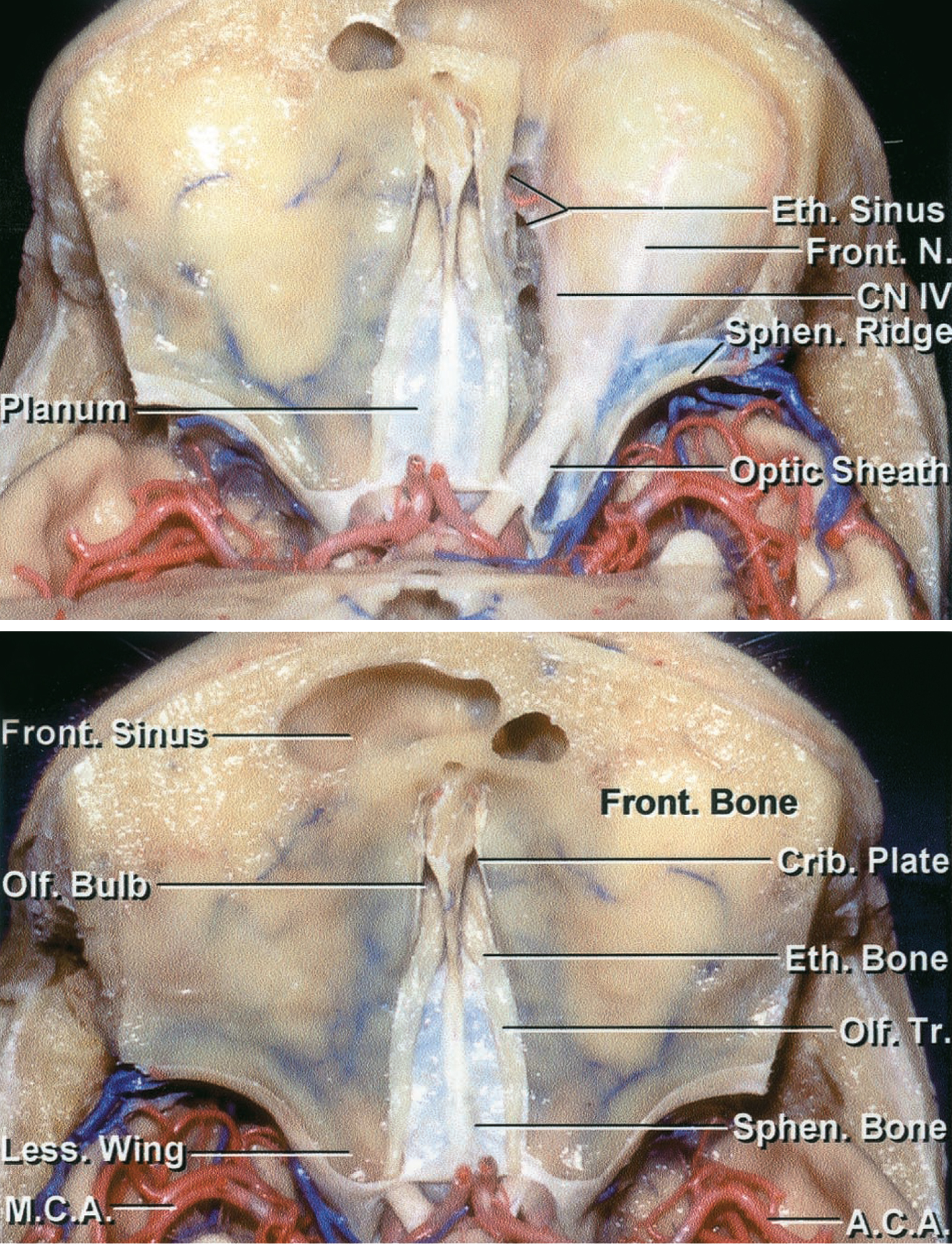
Operative Anatomy
Figure 2: Superior view of the anterior skull base. Notice the accessibility of the A-Comm complex and parasellar region, but also the long operative working distance through the supraorbital subfrontal trajectory. The frontal sinus may be encountered during a supraorbital osteotomy (Images courtesy of AL Rhoton, Jr).
Figure 3: The frontalis branches of the facial nerve are at risk during an eyebrow incision and mobilization of the fat pad at the area of the keyhole. These branches are reflected posteriorly and preserved along with the muscle during an eyebrow incision. These nerves are within the superior fascia of the fat pad; therefore, the pad should not be transected horizontally.
SUPRAORBITAL CRANIOTOMY
The patient is placed on the operating table in a supine position. The degree of head turn is determined by the characteristics of the lesion. Since this approach is mainly used for midline lesions, I frequently turn the patient’s head only 20 degrees.
The pins are placed directly across from each other along the superior temporal line, with the single pin directly above the pinna. The double-pin arm may be rotated to prevent its interference with the bicoronal incision. The patient should be well secured to the table in case the need arises to ‘airplane’ the table in one direction or another.
There are two alternative incision styles for a supraorbital craniotomy: bicoronal and eyebrow incision.
Figure 4: I prefer an eyebrow incision marked just above the eyebrow (top images). The locations of the supraorbital notch and nerve are also marked. Some surgeons prefer the use of a bicoronal (Soutar) incision (bottom images) extending to the level of the contralateral pupil because of potential cosmetic concerns related to the eyebrow incision. I have found the eyebrow incision cosmetically acceptable among patients with normal or thick eyebrows.
By following a low hairline, the Soutar incision may be shortened. The pericranium may be preserved and harvested in a separate layer. The temporalis muscle should initially be left intact. The outline of the craniotomy for both incisions is marked (bottom left). The patient’s head is turned and tilted back ~20 degrees. This maneuver allows the frontal lobes to fall back with gravity.
Figure 5: The location of the frontalis nerve is demonstrated. The nerve is located along the superficial fascia of the fat pad.
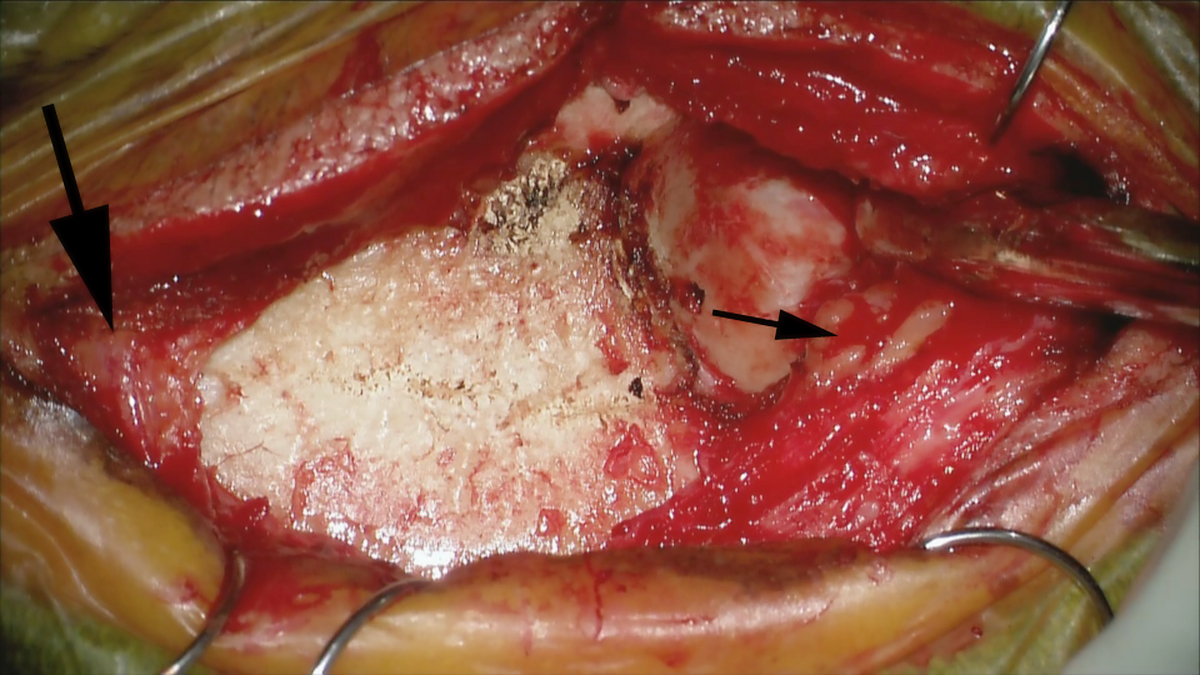
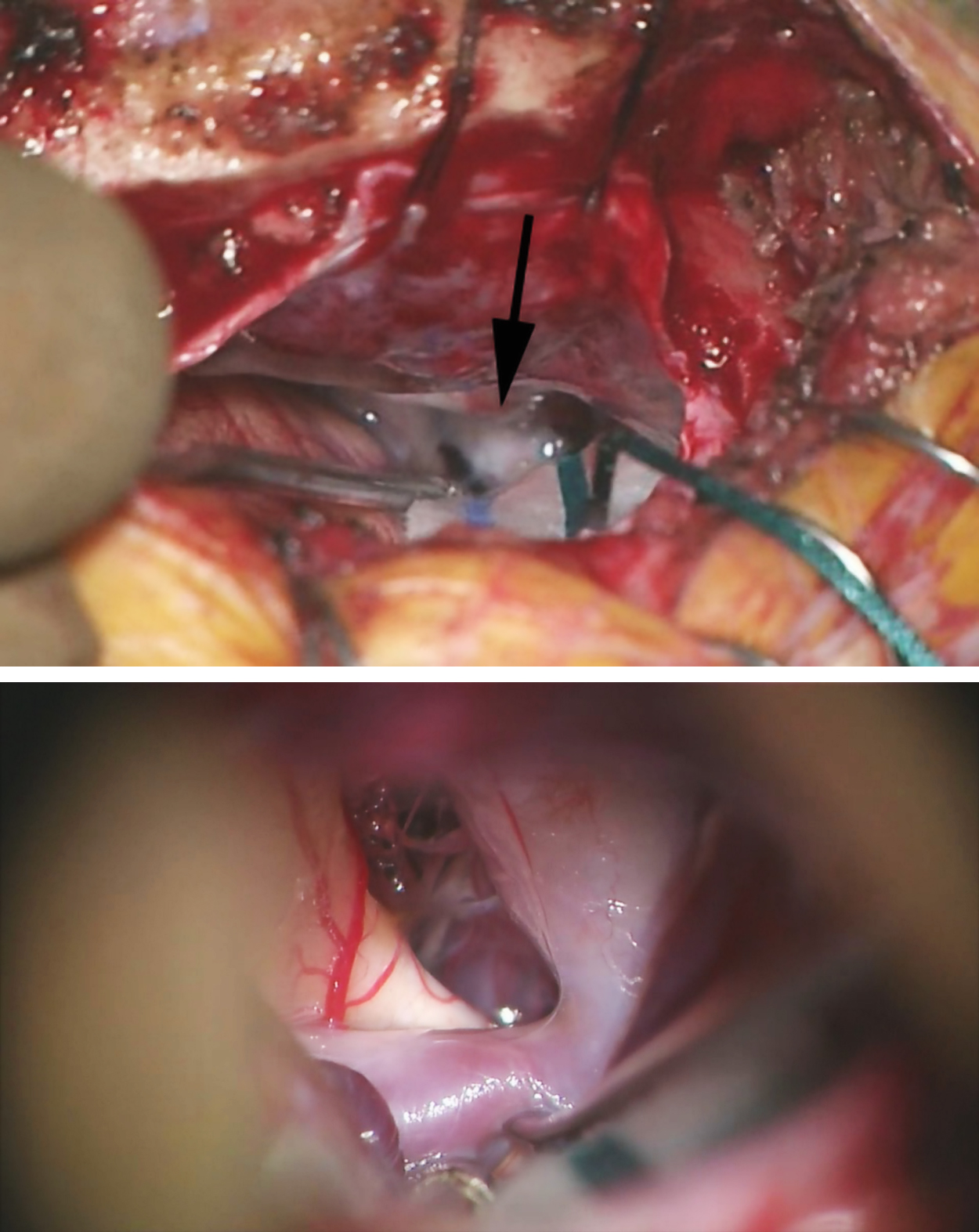
Figure 6: As the eyebrow incision is completed, the supraorbital nerve (large black arrow) is dissected within and released from the subcutaneous space; this nerve defines the medial edge of the incision and must be protected. For the Soutar incision, the scalp is turned forward and a gauze is placed over the globes to prevent pressure injuries.
The location of the frontalis nerve should be remembered to avoid its palsy. The temporalis muscle is left intact during the skin incision. After mobilization of the skin over the area of the keyhole, the soft tissue over the keyhole is transected along the posterior edge of and parallel to the frontal process of the zygoma and the nerve on the fat pad (small black arrow), and muscle is reflected posteriorly to protect the frontalis nerve. Note the tip of the Penfield dissector at the lower edge of the keyhole.
The supraorbital rim must be exposed to gain the appropriate exposure. The pericranium is elevated separately, reflected anteriorly, and kept moist. Fishhook retractors are crucial for maximizing bony exposure for an eyebrow scalp flap. The skin in this region is mobile and can allow for a sizable craniotomy.
A single burr hole is made under the temporalis muscle at the keyhole to expose the frontal dura. The location of this burr hole will determine how easily the craniotomy can be created flush with the orbital roof. A true McCarty keyhole burr hole will expose the frontal dura, and the orbit and can be used to complete a modified orbitozygomatic osteotomy, if necessary.
A dissector can be used to “feel” the roof of the orbit through the keyhole to guide the inferior cut of the craniotomy parallel to the roof. The “tallest” craniotomy should be made through the eyebrow incision. The height of the craniotomy is often the most limiting aspect of the supraorbital eyebrow incision during the intradural work. Navigation may be used to avoid violation of the frontal sinus with the craniotomy. However, bone removal and exposure should not be compromised at the expense of leaving the sinus intact.
Figure 7: For a Soutar incision, the temporalis muscle is elevated over the keyhole (left image) to protect the frontalis nerve and provide a cosmetic closure. A single burr hole is used for the craniotomy through the eyebrow incision (right image). A pericranial flap is harvested because the frontal sinus may be encountered.
Figure 8: After elevation of the bone flap, the overhanging portions of the frontal bone along the inferior edge of the craniotomy are drilled away with a side-cutting bit so that the inferior edge of the craniotomy is flush with the roof of the orbit. The orbital rim may also be removed to expand the inferior to superior operative trajectory for larger tumors with dominant superior extension.
The dura is opened in a U-shaped fashion based on the orbital rim. When the dura is secured with sutures, the frontal lobes will be mobilized away from the cranial base using appropriate methods of brain relaxation such as a lumbar drain and opening of the optico-carotid cisterns. The anterior sylvian fissure is split and optico-carotid arachnoid membranes are released.
Figure 9: Dural tack-up sutures are placed routinely to maintain hemostasis, and the dura is opened in a U-shape fashion. The dura is flapped down toward the face and kept moist to permit easier watertight closure at the end of the operation. You can see that the main limitation of the eyebrow incision is the restricted height of the craniotomy (top). There should be no frontal bone obstructing the view parallel to the orbital roof.
Figure 10: After the dural opening and gentle elevation of the frontal lobe, the optic nerve and the carotid artery (black arrow) are apparent at the depth of the operative field (top image). At higher magnification (bottom image), the carotid artery, A1 branch, and optic nerve are identified. These images demonstrate the panorama of skull base exposed through the eyebrow keyhole craniotomy.
Closure
Figure 11: Avoidance of fixed retractors prevents cortical injury along the basal frontal lobe. You can see the condition of the basal frontal lobe after clip ligation of a large A-Comm aneurysm. The dura is closed with a running suture in a watertight fashion, especially if the frontal sinus has been entered. The pericranial flap may be used for dural closure or coverage of the frontal sinus opening. Watertight dural closure is optional if the frontal sinus has not been entered.
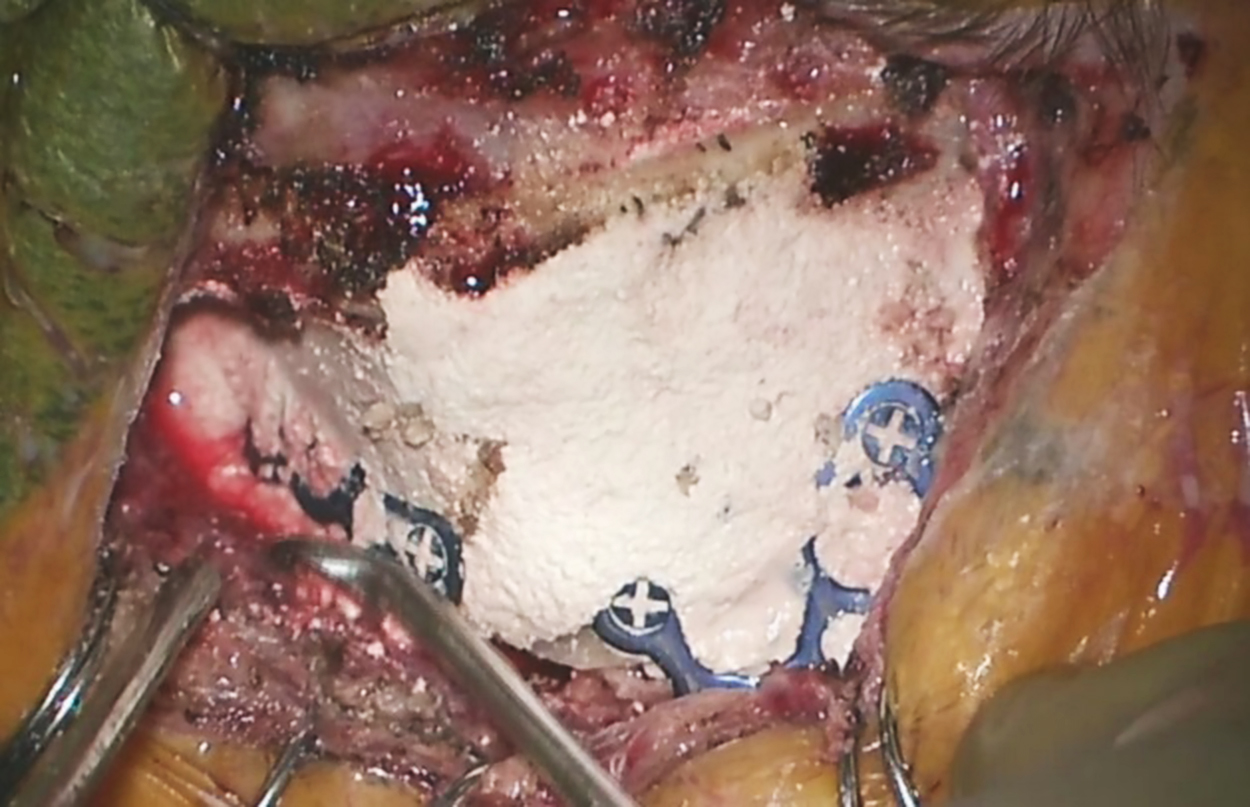
Figure 12: After the bone flap is replaced and fixed with bone plates, a cranioplasty (white material) is performed to fill in the depressions and gaps along the craniotomy edges and to maximize cosmesis. The fixation plates should not be used over the region of the frontal sinus because the screws of the plate can invade the sinus and lead to a cerebrospinal fluid leak.
A subgaleal drain is not implanted and the scalp is closed in the standard fashion. The skin edges are carefully approximated and not strangulated using absorbable sutures. The eyebrow incision must be carefully closed to ensure acceptable cosmetic results.
Orbital Rim Osteotomy or Fronto-Orbital Craniotomy
Figure 13: The osteotomy of the orbital rim can expand the operative corridor and the inferior-to-superior operative trajectory. I use this modified form of supraorbital craniotomy for parasellar lesions with superior extensions or superior intraorbital tumors. The bony cuts (just medial to the supraorbital notch and above the frontozygomatic suture) are demonstrated; the roof of the orbit can be fractured. Please see the following videos for further technical details.
Supraorbital Craniotomy and Orbital Rim Osteotomy for Resection of an Olfactory Groove Meningioma
Supraorbital Craniotomy and Orbital Rim Osteotomy for Intraorbital Tumors
Postoperative Considerations
The patient is observed in the intensive care unit for 1-2 days and then transferred to the wards. The lumbar drain can be used for 1-2 days after surgery to help divert cerebrospinal fluid (CSF) pressures if there is a concern for CSF leakage through the frontal sinus.
It is not uncommon for patients to suffer temporary frontalis palsy after surgery related to retraction of this nerve, but this weakness generally resolves in 4-6 weeks. Numbness in the distribution of the supraorbital nerve is undesirable, and should be avoided during the early steps of the operation by minimizing traction on the nerve.
Pearls and Pitfalls
- The patient’s head must be tilted back to take full advantage of gravity retraction during a supraorbital craniotomy.
- Removal of the supraorbital rim can significantly expand access to the anterior cranial base. This osteotomy will improve the inferior-to-superior operative trajectory.
- An eyebrow incision allows exposure of a variety of lesions in a minimally invasive way. The exposure should be not only minimally invasive, but also minimally disruptive.
- The inferior edge of the craniotomy should be flush with the roof of the orbit.
Contributor: Marcus A. Acioly, MD, PhD
References
Figueiredo EG, Deshmukh P, Nakaji P, Crusius MU, Crawford N, Spetzler RF, Preul MC. The minipterional craniotomy: technical description and anatomic assessment. Neurosurgery. 2007;61(5 Suppl 2):256-265.
Hernesniemi J, Ishii K, Niemelä M, Smrcka M, Kivipelto L, Fujiki M, Shen H. Lateral supraorbital approach as an alternative to the classical pterional approach. Acta Neurochir Suppl. 2005;94:17-21.
Jallo GI, Bognár L. Eyebrow surgery: the supraciliary craniotomy: technical note. Neurosurgery. 2006;59(1 Suppl 1):ONSE157-8.
Jane JA, Park TS, Pobereskin LH, Winn HR, Butler AB. The supraorbital approach: Technical note. Neurosurgery. 1982;11:537-542.
Rhoton AL Jr. The anterior and middle cranial base. Neurosurgery. 2002;51(Suppl 1):273-302.
Wiedemayer H, Sandalcioglu IE, Wiedemayer H, Stolke D. The supraorbital keyhole approach via an eyebrow incision for resection of tumors around the sella and the anterior skull base. Minim Invasive Neurosurg. 2004;47: 221-225.
Please login to post a comment.