Typical Meningioma
Figure 1: This right frontal meningioma demonstrates low T2 signal intensity and is inciting hyperostosis along the inner table of the right frontal calvarium and along the anterior falx. (Left) A hyperintense CSF cleft is also present on T2WI that characterizes this as an extra-axial mass. (Right) On contrast-enhanced T1WI, this lesion shows adjacent dural thickening and enhancement representing a "dural tail."
Figure 2: (Top Right) This meningioma is well circumscribed, obviously extra-axial, and mildly hyperintense on FLAIR. The mass demonstrates moderate enhancement and adjacent dural thickening and enhancement representing a "dural tail." (Bottom) There is also restricted diffusion on DWI, which may or may not be present in meningiomas but often aids in identification when present.
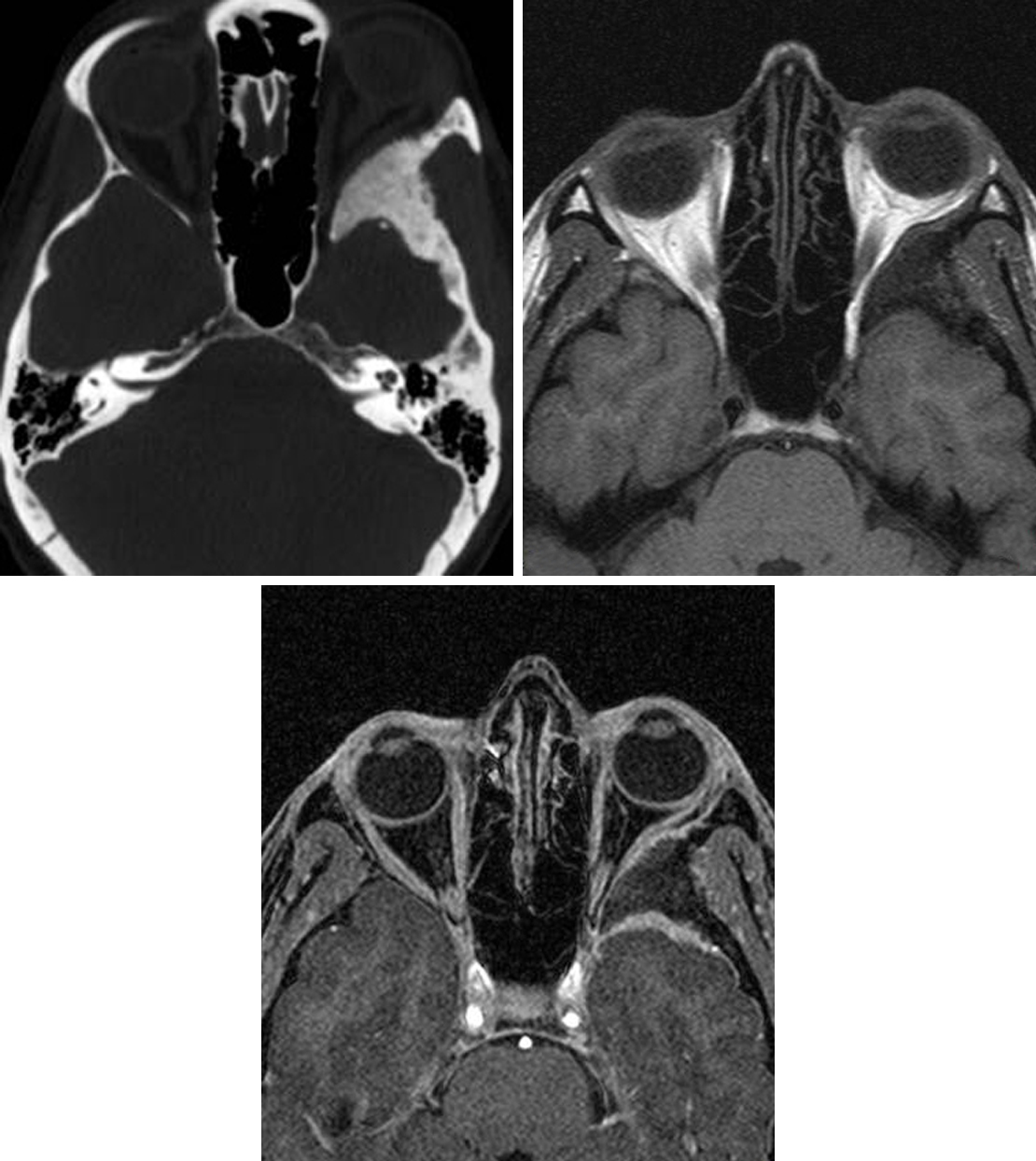
Figure 3: (Top Left) This intraosseous meningioma is visible predominantly as sclerosis and expansion of the left sphenoid wing on CT imaging. (Top Right) Mass effect on the left orbit and low signal sclerosis in the left sphenoid wing is also visible on T1WI. (Bottom) Only with contrast are the en plaque enhancing components obvious in the left middle cranial fossa and in the lateral extraconal space of the left orbit.
BASIC DESCRIPTION
- Benign slow-growing extra-axial tumor arising from arachnoid meningothelial (“cap”) cells
- Most common primary adult intracranial neoplasm
PATHOLOGY
- WHO grade I
- Overwhelming majority are supratentorial (~90%): parasagittal, convexity, sphenoid wing, olfactory groove
- Infratentorial (~10%): most commonly within the cerebellopontine angle (CPA) cistern
- Optic nerve sheath or intraventricular locations may be seen
- Uncommonly arise extracranially: sinonasal, parotid, intraosseous, or skin
- Single or multiple
- Associated with neurofibromatosis type 2 (NF-2)
- “Tumor-to-tumor” metastases to meningioma may be seen (“collision tumor”), most commonly from breast or lung
CLINICAL FEATURES
- Adults (40–60 years old) are most commonly affected; children in cases of NF-2
- Female gender predilection (male/female ratio, 1:2–3)
- Presenting symptoms depend on tumor size and location
- Majority of typical meningiomas are asymptomatic
- Mass effect on adjacent structures resulting in seizures, hemiparesis, visual field defects, cranial nerve defects
- Treatment: serial imaging if small, asymptomatic; surgical resection including dural tail if symptomatic
IMAGING
- General
- Well-marginated, smooth, extra-axial mass with broad dural attachment
- ±Bucking or hyperostosis of adjacent cortex
- Avid, homogeneous enhancement is typical
- Intraosseous extension and dural venous sinus involvement or compression may be present
- CT
- Well-marginated, isodense to hyperdense mass with broad dural attachment
- Variable patterns of calcification common (focal, diffuse, rim, etc)
- Hypodense peritumoral edema sometimes present
- ±Hyperostosis of adjacent bone
- MRI
- T1WI: isointense to hypointense mass; hyperintense areas of calcification
- T2WI: variable signal intensity; ±cystic areas and hyperintense “cerebrospinal fluid (CSF) cleft” separating tumor from adjacent brain
- FLAIR: hyperintense peritumoral edema can be present
- T2*GRE: hypointense signal “blooming” related to calcification
- DWI: variable reduction in diffusivity
- T1WI+C: avid, homogeneous enhancement; ±dural tail (nonspecific finding)
- MR venography: evaluate patency and involvement of dural venous sinuses
- MRS: elevated alanine at short echo times results in triplet peaks at 1.3–1.5 ppm
IMAGING RECOMMENDATIONS
- MRI without and with intravenous contrast; MRS might be helpful in differentiating from other tumor types if ambiguous
For more information, please see the corresponding chapter in Radiopaedia.
Contributor: Rachel Seltman, MD
References
Bosch MM, Wichmann WW, Boltshauser E, et al. Optic nerve sheath meningiomas in patients with neurofibromatosis type 2. Arch Ophthalmol 2006;124:379–385. doi.org/10.1001/archopht.124.3.379.
Buetow MP, Buetow PC, Smirniotopoulos JG. Typical, atypical, and misleading features in meningioma. Radiographics 1991;11:1087–1106. doi.org/10.1148/radiographics.11.6.1749851.
Lin BJ, Chou K-N, Kao H-W, et al. Correlation between magnetic resonance imaging grading and pathological grading in meningioma. J Neurosurg 2014;121:1201–1208. doi.org/10.3171/2014.7.JNS132359.
Osborn AG, Salzman KL, Jhaveri MD. Diagnostic Imaging (3rd ed). Elsevier, Philadelphia, PA; 2016.
Shibuya M. Pathology and molecular genetics of meningioma: recent advances. Neurol Med Chir (Tokyo) 2015;55:14–27. doi.org/10.2176/nmc.ra.2014-0233.
Takeguchi T, Miki H, Shimizu T, et al. The dural tail of intracranial meningiomas on fluid-attenuated inversion-recovery images. Neuroradiology 2004;46:130–135. doi.org/10.1007/s00234-003-1152-4.
Zhang H, Rödiger LA, Shen T, et al. Perfusion MR imaging for differentiation of benign and malignant meningiomas. Neuroradiology 2008;50:525–530. doi.org/10.1007/s00234-008-0373-y.
Zhang H, Rödiger LA, Shen T, et al. Preoperative subtyping of meningiomas by perfusion MR imaging. Neuroradiology 2008;50:835–840. doi.org/10.1007/s00234-008-0417-3.
Please login to post a comment.