Histoplasmosis
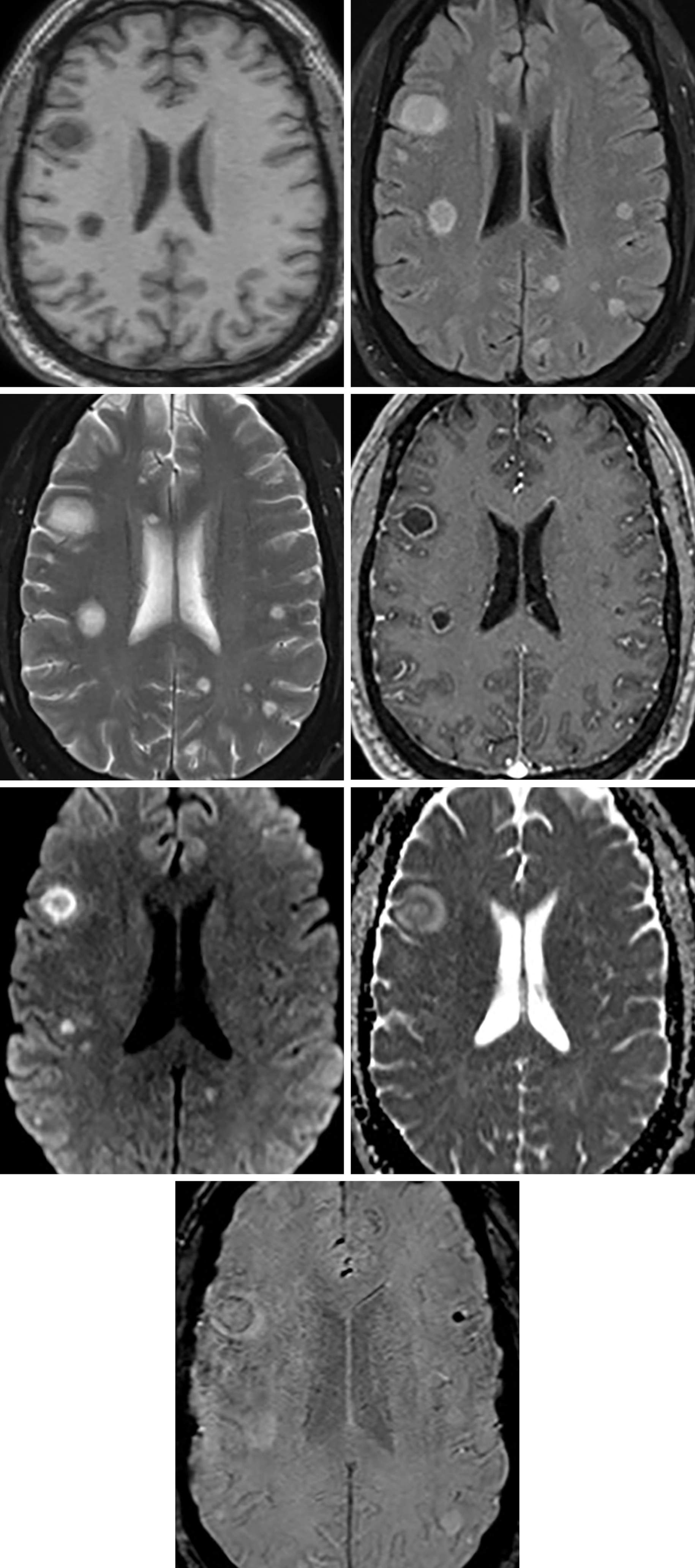
Figure 1: Multiple lesions scattered throughout the parenchyma demonstrating T1 hypointensity (top left) and T2/FLAIR hyperintensity (top right and second row left) with a rim of edema and a thin rim of enhancement (second row right). (Third Row) As is typical with fungal infection, the periphery demonstrates restricted diffusion but not the center of the necrosis. (Bottom) SWI also demonstrates mild dark susceptibility artifact in the periphery of these lesions, likely representing a combination of heavy metal deposition and microhemorrhage.
Description
- Caused by the dimorphic fungus Histoplasma capsulatum
- Exists as a mold in the environment and a yeast at body temperatures
- Endemic to the US Midwest
- Disseminated disease is uncommon and occurs primarily when immune suppression is present
- Represents the first manifestation of AIDS in 50% to 75% of patients
- 5% to 10% of patients with dissemination develop CNS involvement
Pathology
- Grows as a mold in the soil and causes infection when microconidia or hyphal elements are inhaled and convert into yeast in the lungs or when organisms in old foci reactivate during immunosuppression
Clinical Features
- Symptoms
- Usually very nonspecific
- Age and gender
- No predilection
- Median survival
- Variable
- Associations
- If available, look at previous chest imaging for calcified pulmonary nodules or mediastinal lymph nodes
Imaging
- General
- Meningitis, scattered parenchymal lesions, abscesses, and rarely histoplasmomas
- Histoplasmomas: expansile lesion in the thalamus, hypothalamus, or chiasmatic region that is small and round and demonstrates peripheral enhancement
- Modality specific
- CT
- Enhancing mass lesions, atrophy, and hydrocephalus
- MRI
- T1WI
- Hypointense lesions with surrounding hypointense edema
- T2WI
- Hyperintense lesions with surrounding hyperintense edema
- If an abscess, the rim might be hypointense
- DWI
- Variable but typically no restriction
- Contrast
- Diffuse leptomeningeal enhancement
- Ring enhancement typical of an abscess
- T1WI
- CT
- Imaging recommendations
- Standard protocol MRI (including DWI) with intravenous contrast
- Mimic
- Much like other fungal infections, can mimic any of the ring-enhancing lesions and can present as nonspecific meningitis; clinical history with travel to an area of endemicity can help narrow the differential diagnosis
Contributor: Sean Dodson, MD
References
Desai SP, Bazan C 3rd, Hummell W, et al. Disseminated CNS histoplasmosis. AJNR Am J Neuroradiol 1991;12:290–292.
Jain KK, Mittal SK, Kumar S, et al. Imaging features of central nervous system fungal infections. Neurol India 2007;55:241–250. doi.org/10.4103/0028-3886.35685
Saccente M. Central nervous system histoplasmosis. Curr Treat Options Neurol 2008;10:161–167.
Starkey J, Moritani T, Kirby P. MRI of CNS fungal infections: review of aspergillosis to histoplasmosis and everything in between. Clin Neuroradiol 2014; 24:217–230. doi.org/10.1007/s00062-014-0305-7
Tabbal SD, Harik SI. Cerebral histoplasmosis. N Engl J Med 1999;340:1176. doi.org/10.1056/NEJM199904153401506
Wheat LJ, Musial CE, Jenny-Avital E. Diagnosis and management of central nervous system histoplasmosis. Clin Infect Dis 2005;40:844–852. doi.org/10.1086/427880
Zalduondo FM, Provenzale JM, Hulette C,. Meningitis, vasculitis, and cerebritis caused by CNS histoplasmosis: radiologic-pathologic correlation. AJR Am J Roentgenol 1996;166:194–196. doi.org/10.2214/ajr.166.1.8571874
Please login to post a comment.