Bacterial Abscess
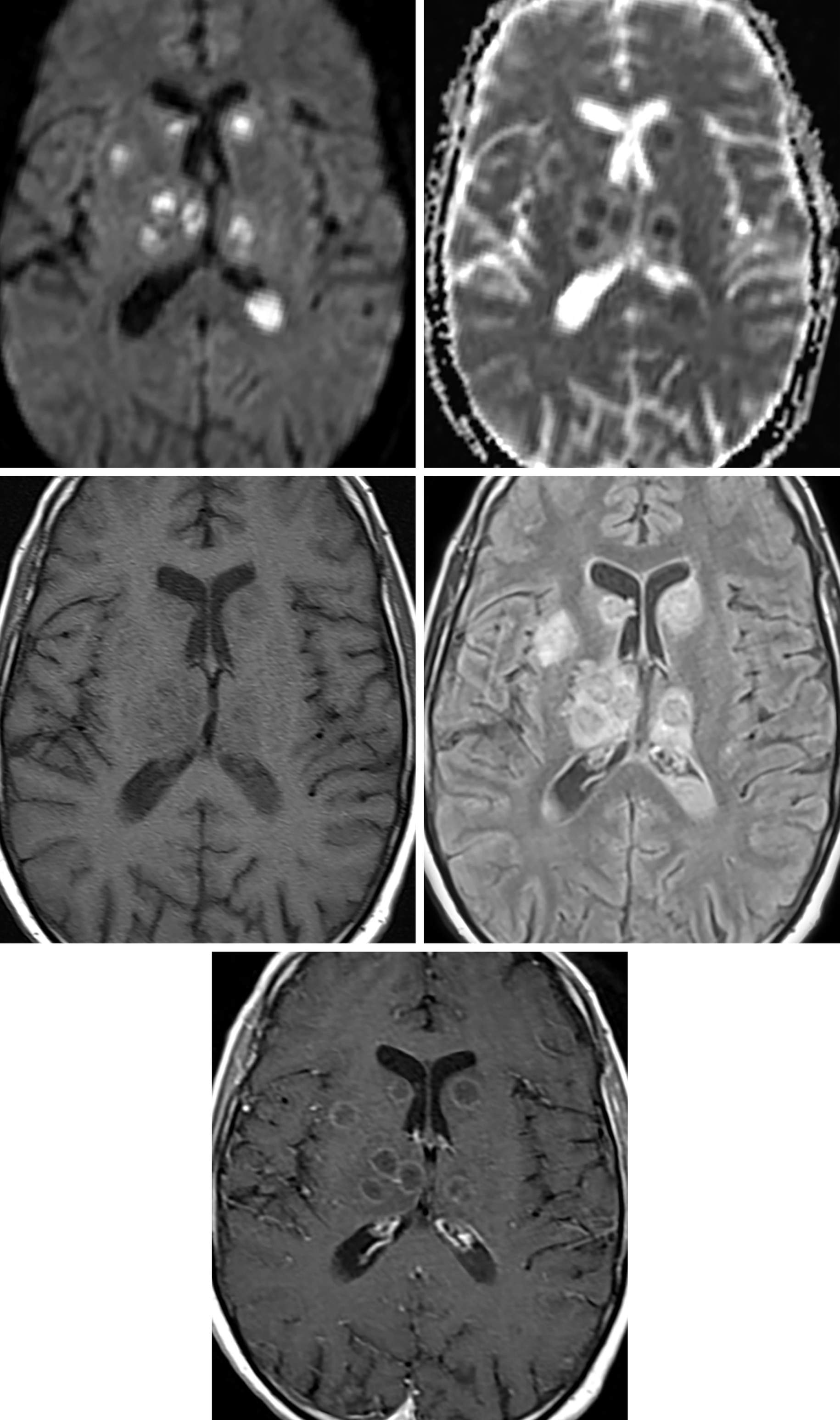
Figure 1: MRI demonstrates multiple FLAIR-hyperintense lesions with primarily central reduced diffusivity with spread into the posterior horns of the lateral ventricles (best demonstrated on the DWI and FLAIR sequences). The central location is fairly classic and suggests a systemic cause of the infection.
Description
- Focal infection that begins as an area of cerebritis and develops into a collection of encapsulated pus
- Mechanisms
- Direct inoculation and hematogenous spread
Pathology
- Britt and Enzmann classification
- Early cerebritis (1st–4th day)
- Ill-defined focal infection
- Late cerebritis (5th–10th day)
- Undergoes central necrosis and vascular proliferation
- Early capsule (10th–14th day)
- Develops a well-defined capsule
- Late capsule (2 weeks to months)
- Thickened capsule with shrinkage of the central cavity
Clinical Features
- Signs and symptoms
- Only 40% to 50% of patients are febrile
- Headache, seizures, altered mental status, focal deficits, nausea, and vomiting
- Demographics
- 2 times more common in men
- Most common in third and fourth decades of life
- Prognosis
- Mortality rates are highly variable but typically up to 30%
- Based on virulence of the organism, size, and location of the infection
Treatment
- If <2.5 cm, antibiotics only
- If >2.5 cm, surgical evacuation and antibiotics
- Steroids for edema and mass effect
Imaging
- General
- Highly variable depending on stage of development
- Most commonly supratentorial
- Location can provide a clue for the site of origin (whether hematogenous or a primary direct spread infection site)
- CT
- Initially appears as an ill-defined, hypodense lesion with mass effect, vasogenic edema, and patchy enhancement
- Develops a capsule and central necrosis
- Capsule initially demonstrates irregular rim enhancement and over time becomes thickened with continuous peripheral enhancement
- Inner rim of enhancement tends to be quite smooth, helping to differentiate from the irregular enhancement in the necrotic center of high-grade tumors
- MRI
- Variable depending on the stage
- DWI is often the most helpful sequence
- Resolving abscess: T2WI hypointense rim resolves, central ADC increases, enhancement is the last to resolve
- T1WI
- Initially will be an ill-defined, heterogeneous hypointense to isointense mass
- As it walls off, will develop definable rim that is often isointense to hyperintense and central hyperintense signal
- The cavity will eventually shrink, and the capsule will thicken
- T2WI
- Hyperintense mass that develops a hypointense rim and demonstrates significant surrounding edema until it begins to resolve
- DWI
- Restricted diffusion (bright on DWI, dark on ADC) throughout the necrotic core, often (although not always) strikingly homogeneous
- This is in contrast to restricted diffusion seen in hypercellular viable tumors, in which the necrotic center (unless hemorrhagic) only rarely demonstrates restricted diffusion
- SWI
- “Dual-rim” sign
- Hypointense along the periphery of the capsule and hyperintense along the inner portion of the capsule
- “Dual-rim” sign
- Contrast
- Early patchy peripheral enhancement that becomes intense, continuous, and thickened with time
- Inner rim of enhancement tends to be quite smooth, helping to differentiate from the irregular enhancement in the necrotic center of high-grade tumors
- MRS
- Central necrotic area can show presence of amino acids (0.9 ppm), lactate (1.3 ppm), acetate (1.9 ppm), succinate (2.4 ppm); metabolites usually not present in tumor
- PWI
- Abscess capsule shows lower relative cerebral blood volume (rCBV) values than rims of enhancing tumors
- Imaging recommendations
- Standard protocol MRI with intravenous contrast to include DWI; MRS and PWI can be helpful
- Mimic
- Bacterial abscess can mimic most ring-enhancing lesions but classically can be differentiated by central diffusion restriction and potential secondary causative etiologies, such as mastoiditis or sinusitis
For more information, please see the corresponding chapter in Radiopaedia.
Contributor: Sean Dodson, MD
References
Bajpai A, Prasad KN, Mishra P, et al. Multimodal approach for diagnosis of bacterial etiology in brain abscess. Magn Reson Imaging 2014;32:491–496. doi.org/10.1016/j.mri.2014.02.015
Chaudhary V, Bano S. MR spectroscopy in the diagnosis of bacterial etiology in brain abscesses. Magn Reson Imaging 2014;32:1434. doi.org/10.1016/j.mri.2014.08.001
Rabelo NN, Silveira Filho LJ, da Silva BNB, et al. Differential diagnosis between neoplastic and non-neoplastic brain lesions in radiology. Arq Bras Neurocir 2016;35:45–61. doi.org/10.1055/s-0035-1570362
Please login to post a comment.