Conducting and Presenting Research Free
Figure 1: Harvey Cushing studied physiological effects of increased intracranial tension (Cushing reflex) in the Hunterian laboratory on primates at the Johns Hopkins Hospital (circa 1904).
Research in Neurosurgery
Modern neurosurgery is a field that is still is in its infancy, and research plays an integral role to its vitality. Neurosurgeons and neurosurgery applicants have participated in a wide variety of research projects encompassing bench research in basic neuroscience, translational research and drug discovery/development, clinical trials and epidemiology, clinical/population/database research, bioengineering and device development, and quality improvement.
Taking time during medical school for research has become increasingly common for most competitive medical and surgical subspecialties, and neurosurgery is no different. The 2016 National Resident Matching Program (NRMP) Charting Outcomes indicate that applicants who successfully matched in neurosurgery in 2016 had an average of 4.8 research experiences, and close to half reported five or more.
Furthermore, matched applicants had an average of 13.4 abstracts, presentations, and publications, more than any other specialty. While taking a year or more to do research is by no means a requirement to match into a neurosurgical program, the applicant pool comprises many students with advanced degrees who have had more time during which to accumulate publications and research experience.
If you are graduating from a medical school with a neurosurgery program that owns limited research assets or decide late to pursue neurosurgery (e.g. at the end of the first clinical year), a research year is a reasonable way to improve your application and better familiarize yourself with the field.
Advantages and Disadvantages of the Extra Time for Research
A research year (or more) should be viewed as an opportunity to learn about the process of conducting basic or clinical research. It is not required, and many applicants who develop an early interest in neurosurgery are able to incorporate rich research experience within the traditional model of four years of medical school. However, 47% of successfully matched applicants graduate from one of the 40 US medical schools with the highest NIH funding, and 32.7% have a PhD or another advanced degree. Many applicants will find it advantageous to take extra time to develop their research portfolio.
Most programs look favorably upon applicants who have cultivated an interest in basic or clinical research that has resulted in peer-reviewed publications and presentations. This stems, in part, from the fact that a neurosurgical program’s reputation is often correlated with its research output and contributions that have improved neurosurgical practice. Every neurosurgery program is looking to hire residents with the interest and the drive to contribute to academic neurosurgery.
In addition to the USMLE scores and letters of recommendation, research output is one of the most important differentiators within the neurosurgery applicant pool. Given how competitive the application to neurosurgical residency has become, applicants with little to no research experience are frequently screened out early at many academically focused programs.
Spending extra time to embark on research projects is not without downsides. While research years are often extremely rewarding, returning to clinical rotations after spending a year or more away from medical school can be challenging for some. Additionally, extra time for research separates you from your entering class, as many students will graduate medical school in only four years. Additionally, students with financial constraints may find it difficult to justify an additional year of medical school loan interest accrual.
When Should a Research Year Take Place?
Applicants often wonder if their research year or years should occur between the second and third year or between the third and fourth year of medical school. Both options have advantages and disadvantages.
Taking time for research between the preclinical years and the first clinical year of medical school takes advantage of a natural transition between classroom-based basic science study and clinical work. In addition, it provides a dedicated time to complete a research project and related publications prior to applying through ERAS. “Accepted” or “published” manuscripts are weighed much more heavily than those that have been “submitted” or are currently in “preparation.” However, a disadvantage of pausing after the preclinical years is that returning to clinical work will be more difficult after a year or more not spent thinking about clinical medicine.
Performance on core clinical rotations is an important factor in the residency application, an applicant who has taken additional time for research must be prepared when returning to clinical service as most of his or her classmates would have recently taken Step 1 and are more able to readily apply this knowledge on clinical rotations. The good news is that the learning curve to perform well on clinical rotations is so steep that there is often little difference in final performance between applicants who proceeded straight into rotations and those who have taken several years for research after a few weeks of rotations.
Taking time between the first and second clinical years (MS3 and MS4) allows you to decide on a specialty after having been exposed to several core rotations. Furthermore, a year on the wards may provide a better perspective on what types of questions are clinically relevant, which may help shape your research interests. Additionally, some medical schools allow students to complete a subinternship prior to the research year if it is taken between MS3 and MS4, which may be a good way to gain further exposure to neurosurgery and your home institution’s department.
If the research year is spent at your home institution, you will have the added benefit of attending departmental conferences and didactic sessions during your year of research. Unfortunately, research performed between MS3 and MS4 may not be complete by the time the ERAS application becomes available.
Despite all the factors above, there does not seem to be a significant difference in match rate between applicants in either of the above categories. Each applicant should decide for himself or herself which option works best.
The timing of USMLE examinations should be planned meticulously. Your USMLE score is the easiest way for programs to filter hundreds of applicants. Do not let yourself be tricked into thinking that a research year is an opportunity to take more time to study for Step 1 or 2. If you are planning to do research between MS2 and MS3, it is important to take Step 1 and then change gears to fully commit to your research endeavors. Perhaps you might gain an extra month of studying at most, but we do not recommend taking more than one month out of your planned research time to study for Step 1. Taking a research year with little to show for it because time was spent studying for boards or participating in other endeavors may negatively impact an application as opposed to helping it.
Similarly, if you plan to do research between MS3 and MS4, it is beneficial to take both components of the Step 2 exam before starting your research while your clinical knowledge and bedside technique are still fresh. This will also help free up time for subinternships and interview travel during MS4. Many students who took a year of research between MS3 and MS4 regret not taking Step 2 prior to their research efforts. Conversely, it is important to recognize that your Step 2 score will be reported in your application if your score report is released prior to submission of the ERAS application.
What Kind of Research Should I Do?
When deciding to take a research year and applying for a research fellowship, one has to decide what kind of research to pursue. Answering this question depends on an applicant’s interests, the availability of projects, labs, and mentors, the applicant’s skills and motivation, and the time available to commit to a project. In the following paragraphs, we introduce the main categories of research available to most neurosurgical applicants and elaborate on their nuances as they pertain to the application process.
Success in research can depend as much on the selection of an appropriate mentor and laboratory as on the individual student factors. Important details to consider when selecting a research mentor include
- The mentor’s history of working with other students and those students’ experiences and results from this mentorship
- The mentor’s availability for formal meetings, informal communication, and research support
- The research opportunities the mentor brings to the table and his or her record of publication
- The mentor’s national prominence
You should begin your search for a research mentor by finding a scientist in your area of interest who has a history of working well with students and a strong publication record. The latter can be discerned through PubMed or Google Scholar searches. Total citation number will provide some insight into how much impact each faculty member has had on the field, but the most prolific researchers are not necessarily the best mentors or recommendation letter writers!
While research within neurosurgery will be most directly relevant in your applications, it is not necessary to conduct all of your research with a neurosurgeon mentor. For reasons we will elaborate on in the section on clinical research below, it is of great benefit to identify one or more academic neurosurgeon mentors within your home institution’s department of neurosurgery.
Basic Science
Basic science, in the context of biomedical research, can be defined as the pursuit of fundamental knowledge about biological systems in the laboratory setting, with or without direct relevance to a clinical problem. Basic science research, especially “wet”, or bench-based laboratory research is extremely time-intensive and can be very difficult to complete within a one-year timeframe, especially if the project requires work with animals or model organisms. Yet, if successful, basic science projects resulting in publications (ideally first-author publications in leading journals) can be a strong boost to a successful application. As a result, such projects should be thought of as high risk, high reward.
Ideally, your project should be clinically relevant, as most neurosurgeons are not basic scientists and therefore are more likely to relate more readily to a clinically-focused research topic during interviews. However, if you are passionate and can speak articulately about your basic science topic of interest, you should not feel discouraged from pursuing that topic.
If you choose to pursue basic science research, it is vital to find a research mentor who thoroughly understands your time constraints and is able to facilitate a project that has a well-defined endpoint that is readily achievable and agreeable to you and existing lab members.
Realize that a bias exists in many lab settings against medical student researchers, who are seen as “dropping in” for a year expecting an easy path to first-author publications in top journals. Unfortunately, many of these stereotypes are corroborated by entitled medical students (many of whom are applying to competitive specialties that demand research experience, such as neurosurgery) who arrive in labs with an attitude and expect to produce work on par with PhD students and postdoctoral fellows, for whom time in lab is not time “off,” as many medical students refer to their research years.
Do not galvanize these stereotypes by expecting 40 hours per week for a year to result in a Nature, Science, or Cell paper. In many high-powered labs, 18-hour workdays, including weekends and holidays, are the norm, and the publication cycle itself can take a year or more. As with all endeavors in neurosurgical training, put your head down, work hard and be efficient, and you can maximize the chances that your efforts will result in a publication.
Despite the challenges posed by your time constraints, your goal should be to publish at least one publication, preferably as a first author. In order to accomplish this task, all data collection should be completed within the designated research year, especially if your project takes place at a different institution. Since basic science work is highly unpredictable, it is likely that unforeseen challenges will arise that prolong experiments, data collection, and analysis.
In fact, experienced scientists often double the amount of time they originally allot for an experiment, as things inevitably require troubleshooting and consultation with collaborators. Maintain a steady, open line of communication with your mentor and labmates, and read the existing literature – it is likely that someone, somewhere has attempted what you are attempting, and it makes little sense to reinvent the wheel when help is available.
You should aim to submit a publication by the end of the research year. Since the peer review process can take months to years (with a current median time between submissions and acceptance hovering around 100 days), it is completely unrealistic to expect that an original basic science manuscript based on the work you start will be published by the time you return to clinical rotations. Stating such an expectation to a research mentor is the fastest way to be written off as entitled.
The reality is that you should consider yourself fortunate to have been given the opportunity to take part in basic science research alongside full-time professionals, who often fight with reviewers and editors for months before the fruits of their labor are recognized with publications. You may have to return to the lab after getting out of the hospital on your clerkships in order to carry out additional experiments requested by reviewers, and you will likely have to reformat your paper once or twice to resubmit to a different journal after rejection. You might get lucky and build a story so compelling that your paper gets accepted right away – great! However, this is extraordinarily rare in today’s research climate. So, again, don’t complain, get to work, and face the publication process with the right attitude.
A note about authorship: while billing itself as the ultimate meritocracy, the basic science world is not without competition and politics. As a result, determining the order of authorship for a publication is a process fraught with emotions and egos. We strongly recommend that you avoid this potential minefield by discussing authorship expectations with your research mentor at the beginning of your time in his or her laboratory and before beginning your research.
In summary, although applicants with a strong record of basic science research are highly desirable to program directors, this type of work is difficult to complete during a one-year interval unless you have deep prior experience working in the laboratory environment.
Clinical Research
Defined loosely, clinical research involves using patient data to reach a conclusion about the way we practice medicine. This can range from a case report detailing an unusual finding in a single patient, to a retrospective analysis of risks or outcomes in a group of patients at a single hospital or across the United States, to a prospective clinical trial to evaluate a new drug.
There may be a smaller barrier to get involved with clinical research than basic science work, but that is not to say that complicated clinical research projects do not require highly specialized skills. For example, a small case series of patients at a single institution might require only a few hours of data collection in the electronic medical record. However, an national-level analysis of predictors of outcomes after a procedure requires intimate familiarity with statistics, statistical programming packages such as SAS, R, Stata, or SPSS, not to mention the thousands of dollars that high-profile national patient databases often cost. These are skills that can be learned, however, perhaps more quickly than basic science techniques, which makes clinical research attractive to applicants.
Additionally, while not every neurosurgery department in the United States is set up to support a full cadre of basic science laboratories, the majority of departments engage in some level of clinical research that is often resident-led. Getting involved in clinical research can be a great way to meet residents and faculty at your home department. Many students find themselves engaged in several projects (often at once) with several different residents and faculty members during medical school. Many students find it easier to generate clinical research publications (including first-author publications) than basic science papers, and, as a result, many will have several to list on their ERAS applications.
Even if you decide to perform basic science research, it may also be beneficial to work on a few clinical studies to maximize the number of publications you can generate and to ensure that even if the basic science experiments fail, there is something to show for your extra research time. This method of risk diversification is advised. Many students find that both types of work can be performed simultaneously, and we highly recommend pursuing at least some clinical work in neurosurgery, regardless of your “main” research focus.
Other Research: Biomedical Engineering, Public Health, Global Neurosurgery…
Naturally, basic science and clinical research are not the only ways by which you can contribute to innovations in neurosurgery and neuroscience. Applicants in neurosurgery come from a variety of backgrounds and undergraduate experiences, and many continue their previous work while in medical school.
If you have a unique set of skills and interests outside of the “wet” lab, do not feel pressured to start a basic science research project in medical school! Your continual demonstration of passion in a field of interest, even if outside the traditional set of choices for medical students, will mean more for your application than changing course and venturing into new, unfamiliar research territory.
For example, if you are an engineer and can continue developing your skills by working on brain-computer interfaces or surgical instruments, you should continue this work and pursue tangible achievements (e.g. a patent, a new medical device, etc.). Pursuing a Masters of Public Health (MPH) degree by working on epidemiological problems in neurosurgery is an acceptable pathway into neurosurgery, as long as you are passionate and can speak knowledgeably about the impact of your work.
If you would rather spend months in a developing country working with local surgeons to develop surgical capacity, go for it – these are all legitimate options that your predecessors who have successfully matched into neurosurgery have pursued.
Types of Publications and Presentations
As of 2016, the ERAS allows applicants to list publications in nine categories: Peer Reviewed Journal Articles/Abstracts, Peer Reviewed Journal Articles/Abstracts (Other than Published), Peer Reviewed Book Chapter, Scientific Monograph, Other Articles, Poster Presentation, Oral Presentation, Peer Reviewed Online Publication, and Non-Peer Reviewed Online Publication. It goes without saying that all publications are not created equal, and applicants must be very careful to correctly categorize their work.
More applicants than you would believe have been devastated to find out during Match week that an embellishment around one of their publications cost them a residency position. As with all aspects of the application, it is imperative to be completely truthful about the number and type of publications you have. For example:
- The existence of the “Peer Reviewed Journal Articles/Abstracts (Other than Published)” category is not a license to list half-complete manuscripts, papers you have submitted, or manuscripts stuck in the review process. It is our position that this section is for accepted manuscripts only, as manuscripts with a status other than “accepted” are completely unverifiable and will raise eyebrows.
- Only list oral presentations that you gave, not presentations you were a part of generating the data for but didn’t actually present.
- Only list posters that you stood in front of and presented at a conference.
- Be certain that you understand the peer review process at the journal to which you have submitted your manuscripts, and categorize them accordingly.
PhD Perspective
If you are an MD/PhD student applying into neurosurgery, you are in good company – in 2016, 9.5% of applicants who successfully matched into neurosurgery owned a PhD degree, versus 4.1% of matched applicants in any specialty. Your additional work confers a number of advantages over traditional MD-only applicants, but there are also some disadvantages.
The most obvious way that an MD/PhD applicant stands out is through his or her research. The PhD degree is, by nature, a research-intensive program, and you will likely complete your degree with several publications, including first-author publications, not to mention an invaluable set of skills that you can transfer to any research setting. The analytical, problem solving-oriented mindset required to succeed in a PhD program will be beneficial in your practice of medicine. The additional emotional maturity that comes with the constant existential struggle that is the modern scientific research process (and with age) will serve you well in your neurosurgical career.
However, MD/PhD programs can make an application to neurosurgery residency more difficult in several ways. First, you will be out of the medical school curriculum for several years, which can make returning to clinical rotations difficult. Many MD/PhD students elect to complete a continuity clerkship to maintain their clinical skills while in lab, while others rely on the fact that (as discussed above) there is little difference between new clinical students after a few weeks of rotations, as the first clerkship or two are difficult for everyone, regardless of time away from medicine.
Unless your thesis lab is in the department of neurosurgery, you may be disconnected from your home institution’s department during your lab years. Therefore, it is adivible to make an effort to remain involved (by conducting clinical research, attending resident mixers, etc.). Conversely, some MD/PhD students feel that they do not need to work on clinical research in their home department due to what they feel is significant basic science achievement.
While a number of high-profile papers may ultimately “rescue” you from the need to produce clinical papers, it is still our opinion that pursuing some clinical research is beneficial, as it will introduce you to techniques you will use throughout residency as well as keep you connected to your department. Finally, expect that many of your interviews will be focused on your PhD work, which you may be expected to talk about in great detail – do not assume that your interviewers without PhDs will be unfamiliar with your work or cannot ask pointed questions about it! It goes without saying that you should be completely prepared to engage your interviewers in conversation about any of your papers or research experiences.
One of the most challenging interview topics involves your plan for balancing clinical and research obligations in your future career. You may find yourself defending the decision to pursue both degrees in one room, convincing an interviewer that you are still committed to learning to operate well in the next, and outlining your three specific aims for your K award proposal in the third. While no one can expect you to have all the answers regarding how you plan to balance running a lab (if you want one) with your neurosurgical practice and your family and hobbies at this stage in your career, you should already be thinking about these things and be able to articulate your thoughts on the matter when asked.
Programs and Funding
There are a number of programs that support a basic science research year. Three of the most well-known programs include the Howard Hughes Medical Institute (HHMI) Medical Research Fellowship, the NIH Medical Research Scholars Program, and the Doris Duke Clinical Research Fellowship. All provide funding for one year of full-time research in a structured laboratory environment.
The NIH program requires that you do research at the NIH with an NIH researcher, which involves moving to Bethesda, MD for the year. The HHMI and Doris Duke programs allow for the medical fellow to perform research with any mentor, but there is a preference for well-known and well-funded labs.
Other options popular with neurosurgery applicants:
- CSNS/CNS Medical Student Summer Fellowship in Socioeconomic Research
- American Association of Neurological Surgeons
- AANS Medical Student Summer Research Fellowship
- Campagana Scholarship in Neurological Surgery
- YNC MISSION Fellowship
- American Brain Tumor Association Medical Student Summer Fellowship
This is a very brief list. We suggest asking other students, research counselors at your school, and searching the internet for more opportunities. Almost every university provides grants to students interested in research, and some will even have grants specific to the neurosciences or neurosurgery. If your school does not provide these opportunities, do not hesitate to apply to another institution for the opportunity. We suggest getting a head start and respecting their deadlines so that you can work accordingly.
When applying to named fellowships, make sure to have a “plan B” in case you do not receive one of these competitive fellowship positions. If given the choice to accept a named fellowship or to conduct research at your home institution for a year without any form of official support, it is usually preferable to participate in the former option. Other reasonable options for applicants interested in clinical research include obtaining a Masters of Public Health or a Masters of Clinical Research degree, which may come with institutional support.
As always, seek constant advice from your mentors in developing a plan for your research time. Be flexible, humble, and resilient if things do not go as first envisioned. Above all, prepare for hard work and an invaluable learning experience!
Presenting Your Research
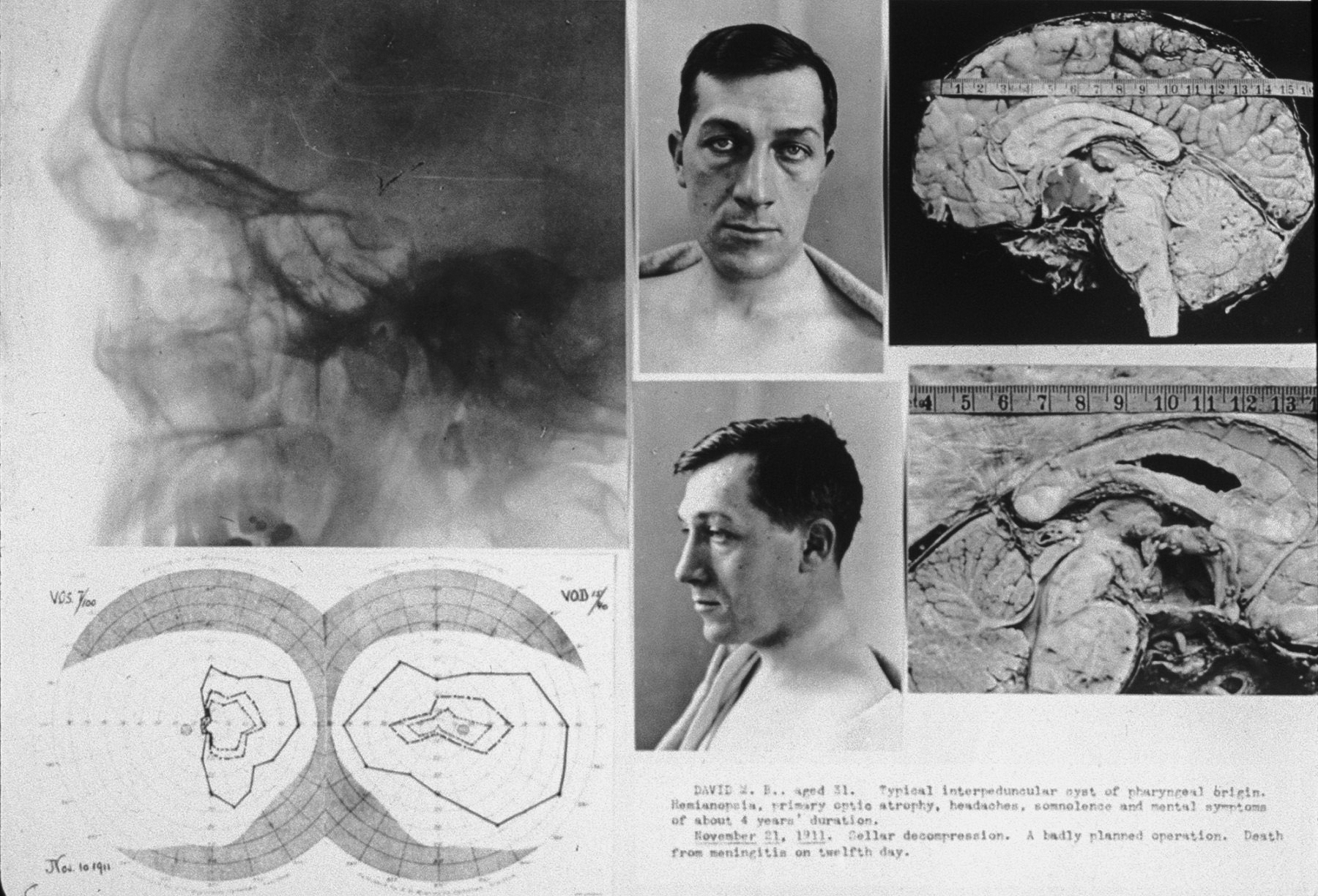
Figure 2: Photos of a patient of Harvey Cushing who died from meningitis after surgery for a suprasellar craniopharyngioma on November 12, 1911. This image is in fact the lantern slide that Cushing used in his lectures to present his clinical research. The operative note by Cushing noted: “Typical interpeduncular cyst of pharyngeal origin. Sellar decompression. A badly planned operation. Death from meningitis on twelfth day.” The autopsy brain specimens on the right demonstrate the extent of tumor decompression through the transsphenoidal route.
Organizing the Presentation and Creating the PowerPoint File
A discussion on the nuances of technique regarding the creation and delivery of effective presentations is beyond the scope of this chapter, but a few important points follow.
You should find out what the time limit for your presentation is at each program. Some programs only want you to speak for five minutes and others expect a 15-minute presentation. It is best to find out what their expectations are and strictly adhere to the time limits. This cannot be stressed enough. If in doubt, err on the side of a shorter, faster presentation.
If you are planning to give a talk about your own research, structure your presentation like you would a research article. Start with a background and rationale for the project. Then discuss the specific aims of your study before going on to your methods, results, and conclusions. The PowerPoint slides should be highly illustrative with helpful graphics and minimal wording so that you are not tempted to read from the slides. Be sure to place your work into the context of the existing literature, but do not overstate its importance. Many applicants have been blacklisted for overinflating the significance of their own work.
If you are giving a talk about an interesting case you witnessed during your rotation, it may help to discuss the structure of the presentation with some of the residents involved with the case. Most presentations start with the evaluation of the patient, the decision-making process, the intervention, and the outcome. You can then choose a particular part of the case to discuss further by means of references from the literature. Try to avoid giving general overviews, since most residents and faculty will find it neither helpful nor informative.
At the end of your presentation, add an acknowledgement slide. Acknowledge the mentors who have helped you with your research, residents/faculty who have helped with your presentation, your funding sources, and the institution for hosting you and giving you the opportunity to present. However, do not go overboard with your acknowledgments.
One infamous interview trail story features a cocky sub-I who spent more than five minutes on his acknowledgements slide alone, thanking his medical school classmates, his parents, and the residents at the program he was presenting to, who he claimed were “like brothers” to him. Needless to say, this tacky behavior was a quick way for this applicant to end up on that program’s blacklist.
Tips on Practicing
Practicing the presentation is key. Time yourself to ensure you stay within the limit. For some students, it helps to write out what you want to say and practice it. You may want to create short bullet points that will guide you rather than complete sentences that you will be tempted to read from. Try to memorize the key points that you want to make for each slide and engage the audience with eye contact while presenting. If you get nervous during presentations and you know this about yourself, then the best way to get around this is to practice numerous times. No matter how nervous you get, by practicing you will know exactly what points need to be made about each slide before moving on.
After practicing on your own, it may be helpful to get feedback from one or two residents at the program. Ask if they would be willing to listen to your presentation and give feedback during their downtime. Their constructive criticism can help you avoid major pitfalls and give you a heads up to faculty with expertise in the field. We also recommend identifying the faculty who are most likely to be interested in the topic of your presentation and invite them to participate and comment sporadically if they are attending the talk. This maneuver shows your knowledge about the program and your collaborative spirit.
Delivering Your Presentation
In the days prior to your presentation, find out what the dress code is for presenters. Usually, it is best to wear formal business attire. It is important to respect how Grand Rounds are held at each institution. If there are other sub-Is, agree on the attire beforehand, such as all wearing your white coat or business suits. Do your best to appear professional, both in terms of attire and grooming.
On the morning of your presentation, arrive early. Bring your presentation on a USB drive or external hard drive and email yourself a copy, just in case. Arriving early will allow you to set up your presentation and get accustomed to the computer and podium. This will also give you some time to address any technical difficulties. Do not assume that residents will give you the morning off from rounds to prepare your presentation. There is generally a culture at each institution, so do your best to learn that and do what previous rotating students have done. Do not exert your own agenda and personal preference!
As mentioned previously, it is important to practice so that, when it comes to the actual presentation, you are able to make eye contact and captivate members of the audience. In fact, if you can get into the actual room you will be presenting, this is the ideal place to practice. Make sure you speak loudly and clearly, as these rooms are often without a microphone and it can be difficult to hear for those in the back of the room.
Be prepared for questions at the end of your presentation, if there is time. It may not be possible to predict what your audience will ask. If you know the answer, take some time and form the sentences in your head before responding so you appear more confident. Another trick is to have appendix slides that contain additional information that can answer likely questions. These slides show attention to detail and forethought regarding questions for your presentation.
A good way to practice answering questions is to repeat the question after it is asked. This can also be helpful to the audience as they often do not hear the question. “Thank you, the question was…” Of course, you should use your best judgment here. If you are presenting in a very small conference room where everyone clearly could hear the question, then skip this tactic.
If you do not know the answer, it’s not the end of the world. The audience expects you to be an expert on your topic, especially if you are presenting your own work, but the best research always generates more questions than it answers. Acknowledge your limitations and do not let them fluster you. Remain calm and it will reflect well even if you do not have a great response. For example, “that’s a great question, I never thought about it that way… or that never crossed my mind… I’m not entirely sure, but I would be happy to look it up and get back to you.” As long as you are gracious, your audience will be receptive to that. Again, find out ahead of time which faculty member has the expertise and ask them to assist you in the discussion of the response to the question. Also, if you tell someone that you will get back to them, definitely do so.
Please login to post a comment.