Balloon Compression
This is a preview. Check to see if you have access to the full video. Check access
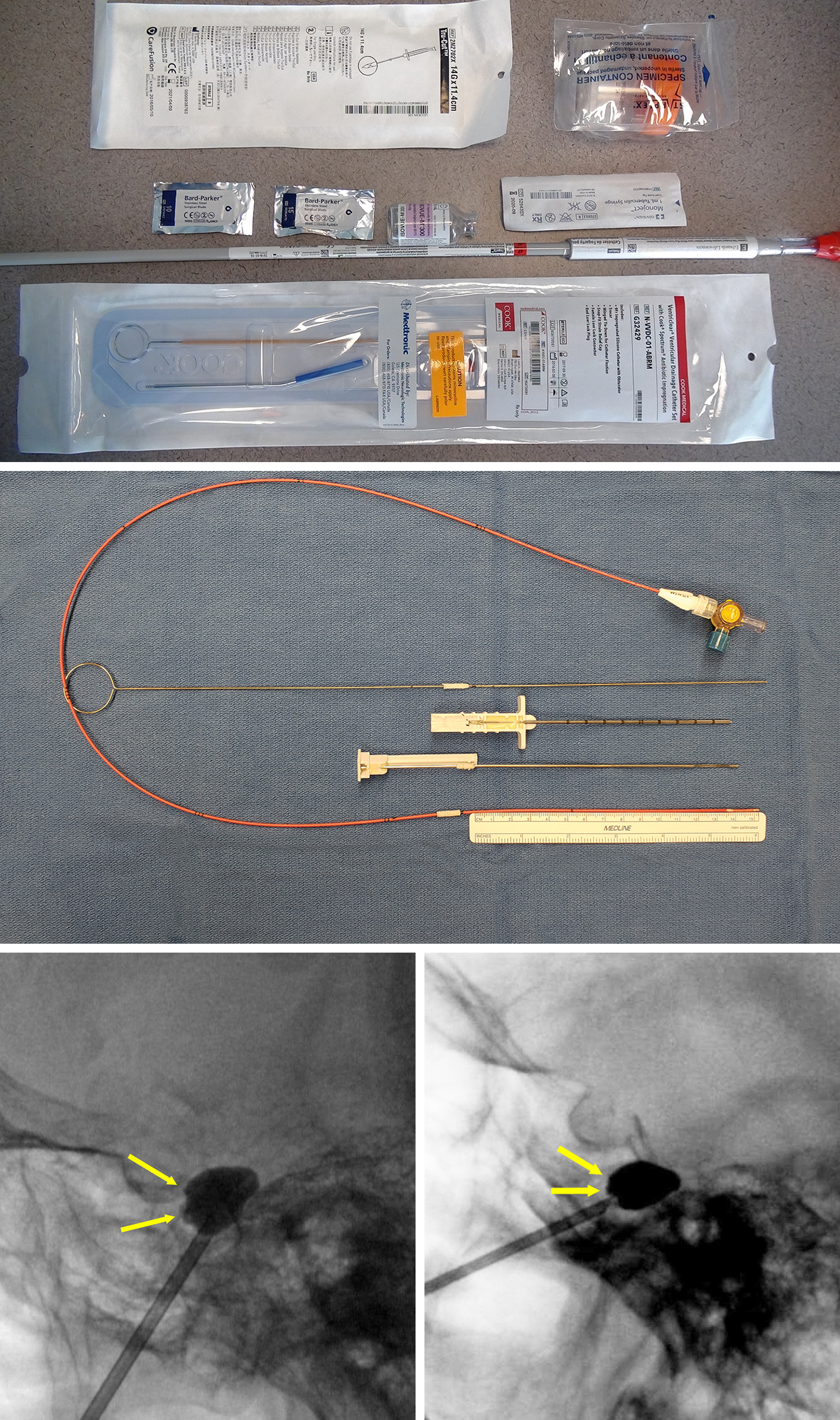
Percutaneous Balloon Compression Using a Kit Prepared by us in the Absence of a Commercially Available Kit
Figure 1: The packaged components of the customized kit described in the above video are shown in the top image. The prepared components are also shown in the middle image. The ideal shapes of the balloons using the technique described in the above video are demonstrated (bottom row). The balloons are herniating slightly into the three foramina of the trigeminal nerve. These ideal shapes are not consistently achievable or necessary for a good outcome.
This is a preview. Check to see if you have access to the full video. Check access
Retrogasserian Balloon Compression Rhizotomy: Technique
The idea that balloon compression can be used for treatment of trigeminal neuralgia (TN) originated from the works of two different surgeons who attempted to decompress the gasserian ganglion.
First, in 1952, Taarnhöj decompressed the posterior gasserian ganglion in 10 patients by dividing the dura through a subtemporal approach.
Later, Shelden and colleagues decompressed the nerve more distally, at the foramina ovale and rotundum. This led to the hypothesis that the operative trauma to the ganglion, rather than decompression, is responsible for pain relief. To test this hypothesis, Shelden and colleagues performed rhizotomies of the trigeminal retrogasserian root and published satisfactory results.
The open technique was transformed into the percutaneous technique by Mullan and Lichtor in 1983 and later modified by Brown in 1996. Nerve compression, manually or by balloon, injures medium and large myelinated fibers while sparing small myelinated and unmyelinated fibers. This injury to the medium and large fibers is responsible for disruption of the ephaptic transmission of pain. Balloon compression is particularly useful in patients with V1 TN because of the ability of this percutaneous modality to preserve the corneal reflex.
Contralateral master weakness is a relative contraindication for this technique because balloon compression causes temporary and (rarely) permanent masseter weakness. Bilateral pterygoid/masseter muscle weakness is not disabling, but it may cause moderate mastication dysfunction.
For more details on indications, limitations, and outcomes of the different percutaneous procedures, please refer to the chapter on General Considerations and Indications.
Operative Procedure
Please refer to the chapter on Placement of the Needle within the Foramen Ovale for further details regarding cannulation of the foramen.
Balloon compression is my preferred percutaneous procedure because it is technically efficacious and, more importantly, since patient cooperation is not required, the patient is anesthetized and comfortable. After intubation, a transcutaneous or transesophageal pacemaker or cardioversion device may be placed in anticipation of a strong trigeminal depressor response.
I have used the commercially available Mullan Percutaneous Trigeminal Ganglion Microcompression Set (Cook Medical, Bloomington, IN) although currently this kit is not available; please refer to the first video in this chapter for details of a customized kit. The Mullan set consists of an access needle with stylet, a blunt obturator, and a microcompression balloon catheter. Alternatively, a 13- or 14-gauge blunt needle with a pointed noncutting stylet can be used and the foramen ovale is accessed using Hartel’s anatomic landmarks.
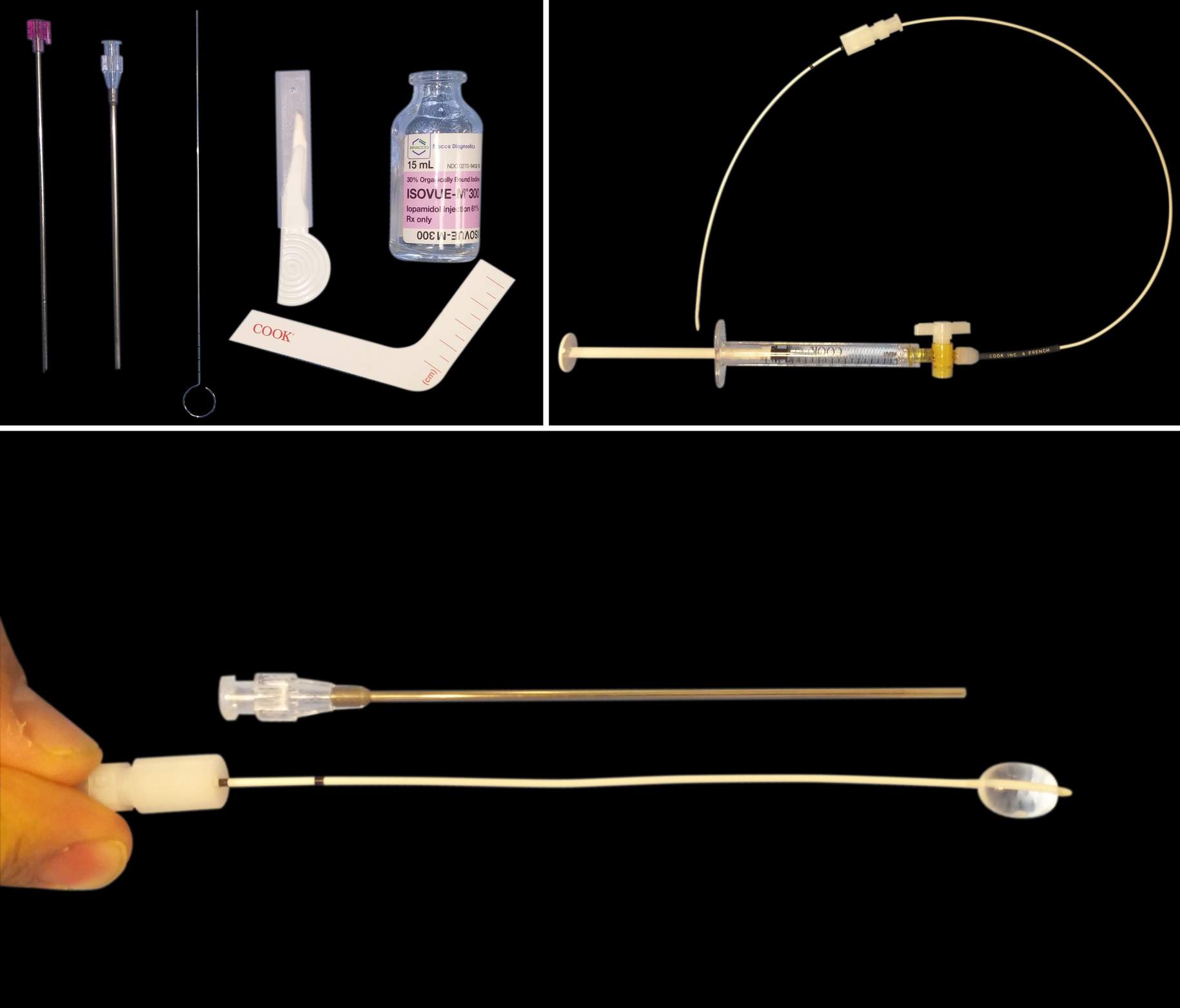
Figure 2: The contents of the Mullan Percutaneous Trigeminal Ganglion Microcompression Set. Note that the set includes an access needle with stylet, blunt and sharp obturators, and a microcompression balloon catheter. A small scalpel used to create a skin stab incision is not shown. Due to the large caliber of the blunt needle, direct entry through the skin with the needle tip is not advised.
Figure 3: Another demonstration of the instruments (upper image). The relation of the distal and proximal black lines marked on the catheter to the hub of the access needle indicate the position of the balloon at the tip of the needle and its final position, respectively.
Once the needle has reached a satisfactory position within the Gasserian cistern and its final location has been confirmed with fluoroscopy, the straight obturator is used to create the path for the balloon. The operator’s attention then turns toward preparing the balloon. If a commercially available set is not used, a Fogarty embolectomy balloon catheter (4F; Edwards Lifesciences, Irvine, CA) is prepared in advance and filled with contrast material to check the integrity of the balloon. The depth of the catheter in relation to the needle tip is marked. The catheter is usually inserted about 17 mm deeper than the needle tip.
The blunt obturator is then removed, and the balloon catheter is passed with its tip into the porous trigeminus along the edge of the petrous bone and dorsal to the Meckel’s cave. I place the balloon as close to the skull base as possible because inflation of the balloon along the superior portions of the Gasserian cistern often leads to the balloon’s entrance over the petrous ridge into the posterior fossa.
Figure 4: The needle tip is situated close to the skull base without exiting the foramen (top image). Using the syringe filled with the contrast agent iohexal, I then inflate the balloon slowly, under X-ray guidance, and watch for development of a pear-shaped balloon after 0.5 mL of contrast injection. The final location of the balloon demonstrates the slight extension of the balloon into the foramen rotundum (blue arrow, bottom image). Development of a pear-shaped balloon confirms correct placement of the balloon in the Meckel’s cave, bounded inferiorly by the petrous bone and superiorly by the dural edge.
Figure 5: In this patient, the location of the needle within the foramen is confirmed (left). Note the slight extension of the balloon into all three foramina of the trigeminal nerve (arrows, right).
Once the pear shape of the balloon is confirmed, the balloon can then be inflated to a pressure of approximately 1,000 to 1,200 mm Hg and compression maintained for 60 to 180 seconds. I usually do not measure the pressure and rather subjectively assess the development of resistance while injecting the contrast (0.75-1 ml) through the syringe. Once I feel a resistance against more injection, I stop because forceful injection leads to rupture of the balloon and the need for its replacement. The balloon is inflated for 120 to 180 seconds for patients who are undergoing repeat operations.
Figure 6: Overinflation of the balloon in the superior direction leads to cranial nerve (CN) VI palsy due to compression of this nerve in the cavernous sinus. The reason for undesirable balloon morphology may be misplacement of the catheter tip lateral to the porus trigeminus and into the middle fossa. It is also possible that the balloon is inflating short of the porus and over the ganglion. The catheter should then be removed and the stylet reused to guide the catheter more medially. Alternatively, the needle may be repositioned more medially to achieve the desirable result.
After the desired compression, the contrast material is suctioned back into the syringe, and the access needle and balloon catheter are removed in one piece. Pressure is applied to the skin puncture site. After extubation, some patients may experience severe, deep, burning pain, which usually subsides spontaneously within a few hours. Patients may be observed as inpatients for 24 hours or discharged home the same day.
Pearls and Pitfalls
- Upon penetrating the foramen, I do not advance the needle deep within the Meckel’s cave because a more shallow penetration keeps the inflated balloon within the Gasserian cistern and avoids its overinflation and displacement over the petrous ridge.
- Due to the larger caliber of the balloon compression access needle compared with the needles used for radiofrequency and glycerol rhizotomy, vascular injuries caused by the balloon compression access needle can potentially be more consequential.
Please login to post a comment.