Geniculate Neuralgia
This is a preview. Check to see if you have access to the full video. Check access
Nervus intermedius transection for geniculate neuralgia: Technique
Geniculate neuralgia, also called nervus intermedius neuralgia or primary otalgia, is a very rare type of facial neuralgia characterized by intermittent episodes of pain located deep in the ear and lasting for seconds or minutes. This neuralgic syndrome is often triggered by sensory or mechanical stimulation of the posterior wall of the external auditory canal. Fewer than 150 cases of this disorder have been reported in the English literature, so accurate data about prevalence, diagnosis, and treatment are not available.
The nervus intermedius takes its name from its intermediate position between the facial and superior vestibular nerves. It was first identified in 1563, and in 1777, Heinrich August Wrisberg named it the “portio media inter comunicantem faciei et nervum auditorium.” This nerve, often called the Wrisberg nerve, carries parasympathetic fibers to the lacrimal and nasopalatine glands and transmits sensory information from the tongue and various skin areas of the nose and concha of the ear. It travels alongside the motor component of the facial nerve and is considered part of this nerve.
The nervus intermedius consists of fibers derived from three distinct nuclei: 1) parasympathetic secretory fibers from the superior salivary nucleus, 2) sensory fibers from the gustatory (superior pole of the solitary nucleus) nucleus in the medulla, and 3) fibers for cutaneous sensation from the dorsal part of the trigeminal tract. The parasympathetic efferent fibers pass to the geniculate ganglion, with or without synapses at the ganglion, before innervating the sublingual and submandibular salivary glands, as well as the main and ancillary lacrimal glands, via the superior petrosal nerve.
The special sensory afferent fibers bring impulses from the taste receptors located in the anterior two-thirds of the tongue, the floor of the mouth, and part of the palate, via the chorda tympani, to the solitary nucleus. The cutaneous somatic afferent fibers bring impulses from the sensory receptors located in the concha of the auricle, behind the ear, in the posterior wall of the external auditory canal, and in the outer layer of the tympanic membrane.
The course of the nervus intermedius and the motor root of the facial nerve can be divided into cisternal, meatal, labyrinthal, and extracranial parts. The average length of each of the three segments is approximately 2 cm. The first segment adheres to the vestibulocochlear nerve at the nerve root; the second segment runs separately between cranial nerves (CN’s) VII and VIII; and the third segment joins the motor root of the facial nerve within the internal auditory canal.
Diagnosis and Evaluation
Diagnosis of geniculate neuralgia, like other cranial nerve compression syndromes, is strictly clinical because no imaging or testing modality has been found to reliably reach the diagnosis.
Although the clinical presentation of geniculate neuralgia is varied, it classically manifests as acute paroxysmal stabbing pain centered within the ear. It may be localized in the auditory canal, pinna, retroauricular region, or even the soft palate, and may sometimes radiate to the temporal region or the angle of the mandible. The pain may be triggered by sensory or mechanical stimuli such as water in the shower, a breeze of air, or other cutaneous stimuli touching the posterior wall of the auditory canal. The pain may be associated with disorders of lacrimation, gustatory sensation, and salivation.
For a correct diagnosis, all other possible non-neuralgic causes of otalgia must be eliminated. These include otitis externa or media; a malignancy of the pinna, external auditory canal, temporal bone, or nasopharynx; lesions of dental origin; temporomandibular joint diseases; vascular lesions; referred pain from nasopharyngeal and laryngeal lesions; intracranial lesions in the cerebellopontine angle; and rare syndromes such as Eagle syndrome. Therefore, thorough neurologic, dental, and other comprehensive otolaryngological examinations must be performed.
It is also important to differentiate geniculate neuralgia from other forms of neuralgia. The sensation of the ear is supplied by CN’s V, VII, IX, and X, as well as by the 2nd and 3rd cervical nerves, so it is not uncommon to see an overlap among other facial neuralgias. The two most likely differential diagnoses of geniculate neuralgia are trigeminal neuralgia and glossopharyngeal neuralgia. Characteristics of the pain can be similar to those of geniculate neuralgia—only the location and distribution of the pain enable a reliable differentiation between them.
As part of the diagnostic workup when assessing a patient with suspected geniculate neuralgia, a fine-cut magnetic resonance image (MRI) of the cerebellopontine angle must be obtained. This may identify a vascular loop compressing the CN VII/VIII Complex. Other tests that may help exclude other causes of otalgia include pure tone audiometry, auditory evoked brainstem responses, and vestibular function tests.
Indications for Surgery
It is important to re-emphasize that most patient with intractable ear pain do not have geniculate neuralgia. I am very selective in offering operative interventions to patients suffering from geniculate neuralgia. Experience is paramount in selection of appropriate candidates.
The first-line treatment for geniculate neuralgia is medical therapy, with surgery reserved for refractory cases. Commonly used medications include carbamazepine, gabapentin, and lamotrigine. As these drugs affect different sites of action, combination drug therapy may benefit patients who are nonresponsive to standard regimens of single-drug therapy. An alternative to medical therapy is regional nerve blocks.
Surgical Procedure
Surgical options can be considered in situations of drug intolerance, inefficacy, allergies, or side effects. The two most common surgical procedures include transection of the intracisternal segment of the nervus intermedius and microvascular decompression (MVD) of the nerve at its root entry zone near the brainstem.
I prefer sectioning the cisternal segment of the nervus intermedius through a retromastoid craniotomy. The following discussion describes the methodology.
Preoperative Considerations
As stated above, a comprehensive otolaryngological work-up is necessary to exclude all other causes for geniculate neuralgia and must be completed before operative intervention is offered to the patient. The pain should be neuralgic and not neuropathic. The risk of postoperative intractable vertigo due to manipulation of CN VIII is significant, and therefore only patients with “certain” diagnosis should undergo surgery. Cutaneous triggers are mandatory for consideration of surgery.
Brainstem auditory evoked responses (BAERs) should be routinely monitored intraoperatively.
Operative Anatomy
The following images demonstrate the relevant operative anatomy.
Click here to view the interactive module and related content for this image.
Figure 1: Exposure of the cranial nerves within the cerebellopontine angle after a right-sided retrosigmoid approach (A). The nervus intermedius is located between the superior vestibular nerve and the facial nerve (B). Another view of the nervus intermedius is demonstrated (C). The superior and inferior vestibular nerves have been divided to expose the facial and cochlear nerves (D). A labyrinthine branch of the anterior inferior cerebellar artery (AICA) is also apparent (Images courtesy of AL Rhoton, Jr).
Click here to view the interactive module and related content for this image.
Figure 2: Left retrosigmoid exposure. Note the cleavage plane between the superior and inferior vestibular nerves (C). Posterior view of the internal auditory canal (D). Note the intimate relationship of the nervus intermedius with the facial nerve. An enlarged view of the nerves within the meatus (E). The cleavage plane between the superior and inferior vestibular nerves has been extended to visualize individual nerve bundles (F)(Images courtesy of AL Rhoton, Jr).
NERVUS INTERMEDIUS TRANSECTION
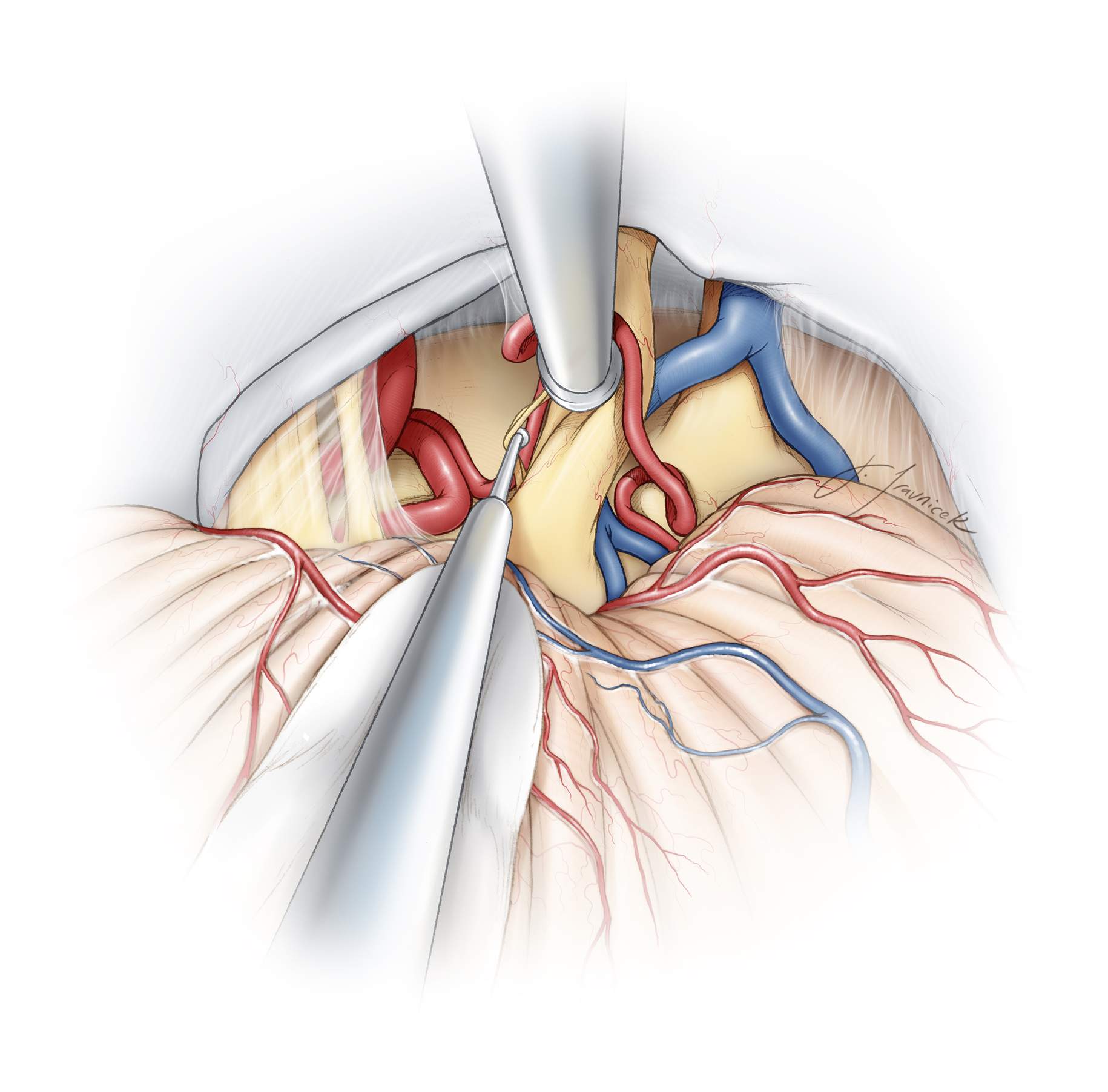
The retromastoid craniotomy for nervus intermedius sectioning is the same as the one for microvascular decompression for trigeminal neuralgia. I use the supralateral cerebellar approach to expose the superior aspect of the CN VII/VIII complex.
Please refer to the chapter on Retromastoid Craniotomy for a detailed description of the approach.
Figure 3: The operative corridors and trajectories for accessing the cerebellopontine angle: The surgical corridors for microvascular decompression for trigeminal neuralgia (supralateral cerebellar approach-blue arrow) and hemifacial spasm, and glossopharyngeal neuralgia (infralateral cerebellar or infrafloccular approach-green arrow) are illustrated. I use the supralateral cerebellar corridor to access the nervus intermedius.
INTRADURAL PROCEDURE
There is a significant overlap among the pain syndromes of geniculate neuralgia, trigeminal neuralgia, and glossopharyngeal neuralgia. Consequently, my operative philosophy for geniculate neuralgia is to explore CN V for MVD, section the nervus intermedius, and explore CN’s IX and X for MVD.
The relevant details of exposure for the CN’s V-X have been previously discussed in the chapters of MVD for Trigeminal Neuralgia and Hemifacial Spasm.
A piece of glove (cut slightly larger than the cottonoid patty) acts as a rubber dam. It protects the cerebellar hemisphere against the rough surface of the cottonoid as the rubber dam slides over the cerebellum while dissection is continued to expose the cerebellopontine angle. I identify the junction of the petrous bone and tentorium and advance the cottonoid over the rubber dam near the turn of the petrous bone toward the lower aspect of CN V and upper aspect of CN VII/VIII.
Medial retraction of the cerebellum parallel to CN VII/VIII complex is avoided to prevent direct transmission of retraction to these nerves. The alternating intermittent vectors of retraction are parallel to CN’s V and IX. Note that I do not apply fixed retractors, but instead use the suction apparatus to mobilize the cerebellar hemisphere in a dynamic fashion during dissection. Along with generous opening of the regional arachnoid membranes over the cranial nerves, this maneuver minimizes the risk of hearing loss. Dynamic retraction of the suction apparatus allows intermittent exposure only where needed. Aggressive retraction of fixed retractors often provides exposure at places that may not be necessary.
Figure 5: After exposure of CN’s V-X, first, the root entry zone of the trigeminal nerve is examined thoroughly to exclude the presence of any convincing compressive arterial loop. If there is no offending arterial loop, I consider the large veins causing discoloration on the nerve to potentially be the source of the neurovascular conflict.
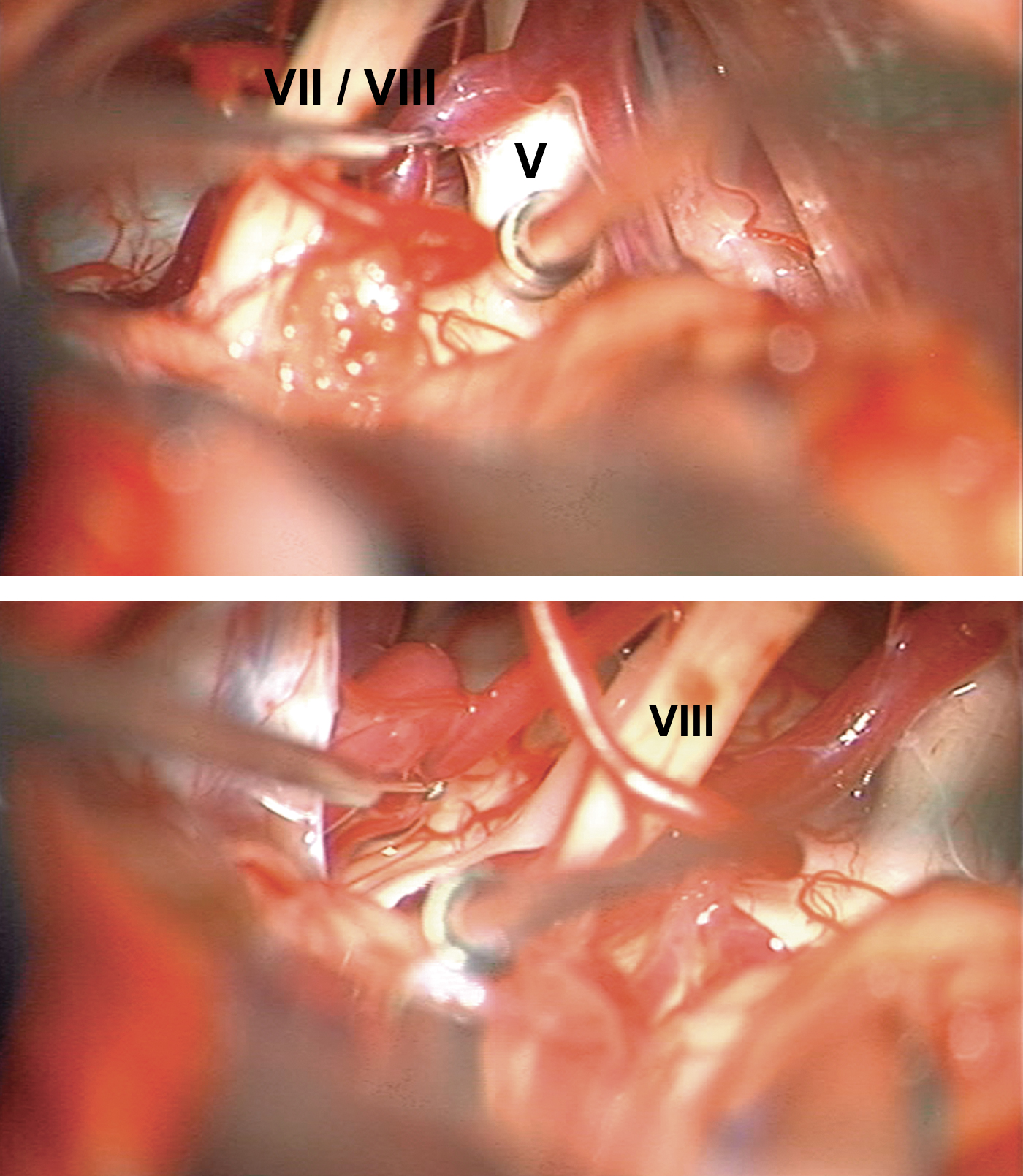
Figure 6: Intraoperative images demonstrating exposure and inspection of the left trigeminal nerve root entry zone (top image). The brainstem at the level of the superior and inferior aspects of CN’s VII/VIII is then examined for any obvious compressive vessel (bottom image). Please see images C and D below for the next steps.
Figure 7: Using a fine dissector under magnification, I carefully and gently mobilize CN’s VII or VIII and look around their edges for the nervus intermedius, which should be located between the superior vestibular and facial nerves. Any significant manipulation of the vestibular nerves will significantly increase the risk of disabling postoperative vertigo and balance dysfunction.
Figure 8: Most often, I find the nervus intermedius between and along the inferior aspect of the CN VII/VIII complex using a fine ball-tipped dissector. This nerve often consists of 1-4 fine strands. The cochlear nerve is carefully tracked using BAERs monitoring.
Figure 9: This intraoperative view illustrates exposure of the nervus intermedius and its separation from the CN VII/VIII complex using a ball-tipped dissector.
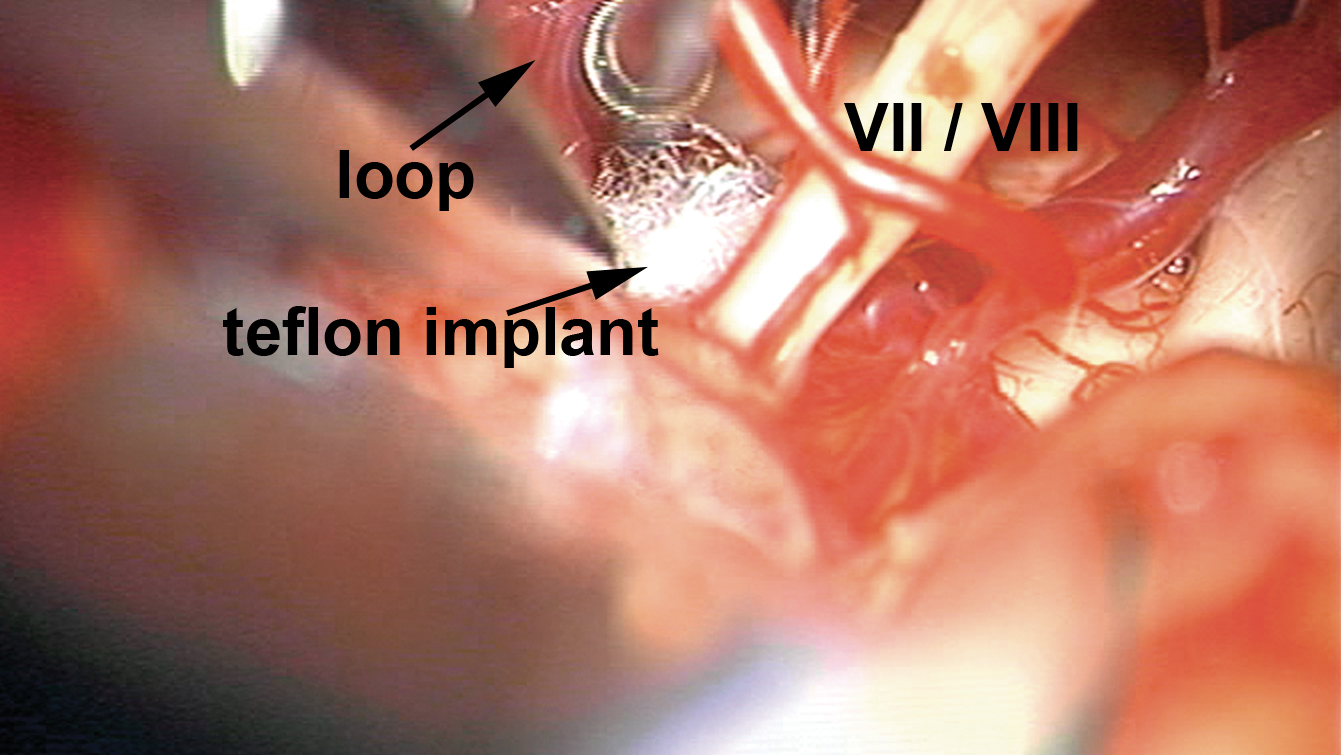
Figure 10: The nervus intermedius is then divided using microscissors. A fine dissector keeps the nerve away from CN’s VII/VIII while it is cut.
Figure 11: Once the nervus intermedius is divided, it is advisable to ensure that no offending vascular loop is abutting the CN VII/VIII complex near the brainstem. If a vascular loop is identified, it is mobilized along its entire length using multiple pieces of shredded Teflon. It is important to mobilize any offending vessels along the root exit zones of CN’s IX-X as well (inset). Atypical forms of glossopharyngeal neuralgia may present as geniculate neuralgia.
Figure 12: This intraoperative view discloses placement of pieces of shredded Teflon implant between the offending vascular loop and CN’s VII-X.
MVD for Geniculate Neuralgia: Alternative Operative Findings
Closure
The dura is approximated primarily. I do not routinely perform a watertight dural closure and have experienced a very low rate of cerebrospinal fluid leakage through the incision or the nose. Mastoid air cells are rewaxed thoroughly (“wax in, wax out”) and the bone flap is replaced or a methyl methacrylate cranioplasty is performed. The muscle and scalp are closed in anatomic layers. Please refer to the Retromastoid Craniotomy chapter for more details regarding closure.
Postoperative Considerations
After surgery, patients are usually admitted to the ICU for an overnight observation and then transferred to the regular ward for a couple of days before they can be discharged home. Special attention should be paid to hemodynamic parameters, neurologic examination, and wound care.
Reported side effects of nervus intermedius sectioning include decreases in lacrimation, salivation, and taste. Postoperative vertigo may occur and may be disabling, requiring rehabilitation therapy. Most patients will have relief of their pain if they were appropriately selected for surgery.
Pearls and Pitfalls
- Geniculate or nervus intermedius neuralgia is a rare type of facial neuralgia characterized by intermittent episodes of pain located deep in the ear that last for seconds or minutes, and often triggered by sensory or mechanical stimulation of the posterior wall of the external auditory canal.
- The symptoms of geniculate neuralgia overlap with those of trigeminal and glossopharyngeal neuralgia. Pathologies of the ear, temporomandibular joint, and nasopharynx should be ruled out through otolaryngological consultation.
- Retraction of the cerebellum parallel to the path of CN VIII should be minimized. Sharp arachnoid dissection and strategic dynamic cerebellar retraction will facilitate cerebellar mobilization without placing the cranial nerves at risk. These maneuvers will allow adequate exposure to permit safe inspection of the cranial nerves and sectioning of the nervus intermedius. The root entry/exit zones of CN’s V-X should be inspected.
Contributor: Aqueel Pabaney, MD
References
Headache Classification Subcommittee of the International Headache Society. The International Classification of Headache Disorders: 2nd edition. Cephalagia 2004;24(Suppl 1):9–160
Pulec JL. Geniculate neuralgia: diagnosis and surgical management. Laryngoscope 1976;86:955–964
Pulec JL. Geniculate neuralgia: Long-term results of surgical treatment. Ear Nose Throat J 2002;81:30-33.
Rhoton AL Jr. The cerebellopontine angle and posterior fossa cranial nerves by the retrosigmoid approach. Neurosurgery 2000;47(Suppl 3):S93-129.
Rupa V, Saunders RL, Weider DJ. Geniculate neuralgia: The surgical management of primary otalgia. J Neurosurg 1991;75:505–511.
Sachs E Jr. The role of the nervus intermedius in facial neuralgia. Report of four cases with observations on the pathways for taste, lacrimation, and pain in the face. J Neurosurg 1968;28:54–60
Tang IP, Freeman SR, Kontorinis G, Tang MY, Rutherford SA, King AT, Lloyd SK. Geniculate neuralgia: A systematic review. J Laryngol Otol 2014;128:394-399.
Tubbs RS, Mosier KM, Cohen-Gadol AA. Geniculate neuralgia: Clinical, radiologic, and intraoperative correlates. World Neurosurg 2013;80:e353-357.
Tubbs RS, Steck DT, Mortazavi MM, Cohen-Gadol AA. The nervus intermedius: A review of its anatomy, function, pathology, and role in neurosurgery. World Neurosurg 2013;79:763-767.
Please login to post a comment.