Interhemispheric Craniotomy Free
This is a preview. Check to see if you have access to the full video. Check access
Interhemispheric Dissection for Reaching the Ventricular System
General Considerations
The anterior or posterior interhemispheric craniotomy provides access to deep midline parafalcine and paraventricular spaces through the natural interhemispheric fissure. Although working in this natural plane has numerous benefits, such as a minimal need for brain retraction and transgression, the working corridor can be deep and narrow, making surgery in this region technically challenging.
This craniotomy is situated around the coronal suture (when using a frontal interhemispheric route) or behind the central lobule (when using the superior parietal interhemispheric route) to protect the sensorimotor cortices and dominant numerous parasagittal veins, which are typically 3-4 cm posterior to the coronal suture.
Sacrifice of the large parasagittal bridging veins may lead to venous infarction and hemiparesis. Fixed retractors must be avoided through the use of dynamic or gravity induced retraction (with the patient in a lateral position) and early cerebrospinal fluid (CSF) drainage (via lumbar drainage or a ventriculostomy) to mobilize the hemisphere away from the midline.
Modifications of the interhemispheric route may expand the traditional confinements of the operative corridor through this pathway.
Figure 1: The contralateral transfalcine “cross-court” corridor (green zone) affords more flexible working angles for lesions that extend laterally. This modification of the ipsilateral interhemispheric route reduces retraction on the ipsilateral hemisphere (red zone) while reaching the lateral pole of the tumor.
In this chapter, I will highlight nuances of techniques for optimizing the interhemispheric approach and its modifications.
Indications for the Approach
The typical pathologies uncovered through this approach include parafalcine meningiomas, medial hemispheric gliomas, distal anterior cerebral artery aneurysms, metastases, arteriovenous malformations, and tumors in and near the anterior third ventricle such as colloid cysts, hypothalamic hamartomas, and craniopharyngiomas.
For posterior third ventricular masses, the craniotomy is centered over the coronal suture and a more posterior callosotomy is necessary. Posterior thalamic tumors and pineal region masses with predominantly superior extension are also reasonable candidates for the posterior interhemispheric transcallosal intervenous (working around the internal cerebral veins) route.
The use of this approach to access a pericallosal aneurysm depends on the location of the aneurysm relative to the genu of the corpus callosum. For aneurysms that are below the genu, a low interhemispheric approach is preferred in order to secure proximal vascular control.
The lateral trajectory of the interhemispheric approach is limited, and I do not advise its use for lesions primarily affecting the ipsilateral thalamus or caudate nucleus. I prefer the contralateral interhemispheric or ipsilateral transcortical corridors for such laterally located lesions.
Preoperative Considerations
For large tumors such as parafalcine meningiomas, intraoperative CSF drainage facilitates brain relaxation and mobilization of the tumor and its devascularization at the level of the falx early in surgery. A lumbar drain is the method of choice for this purpose because the basal cisterns and the ventricles are often not readily accessible during dissection of the interhemispheric fissure.
The superior sagittal sinus and corresponding bridging veins should be evaluated on preoperative magnetic resonance images, and if necessary, a magnetic resonance venogram or computed tomography angiogram should be performed. Although the involved venous structures along the anterior third of the sagittal sinus are considered safe for ligation, the risk of significant venous infarcts persists. Therefore, manipulation and sacrifice of these venous structures must be kept to a minimum.
If there are numerous large parasagittal veins draining into the sagittal sinus overlying the parafalcine tumor, it would be ill-advised to ligate these veins; instead, a contralateral interhemispheric transfalcine approach can be an option. Parafalcine meningiomas typically do not require ligation of the superior sagittal sinus, but if they are found to infiltrate the sinus, appropriate precautions for avoidance and management of air embolism is mandatory preoperatively.
In patients with large tumors, mannitol 1g/kg is administered during skin incision. If a lumbar drain is available, 30-40 cc of CSF is drained gradually during craniotomy.
Operative Anatomy
An understanding of parasagittal venous anatomy is important for execution of this approach.
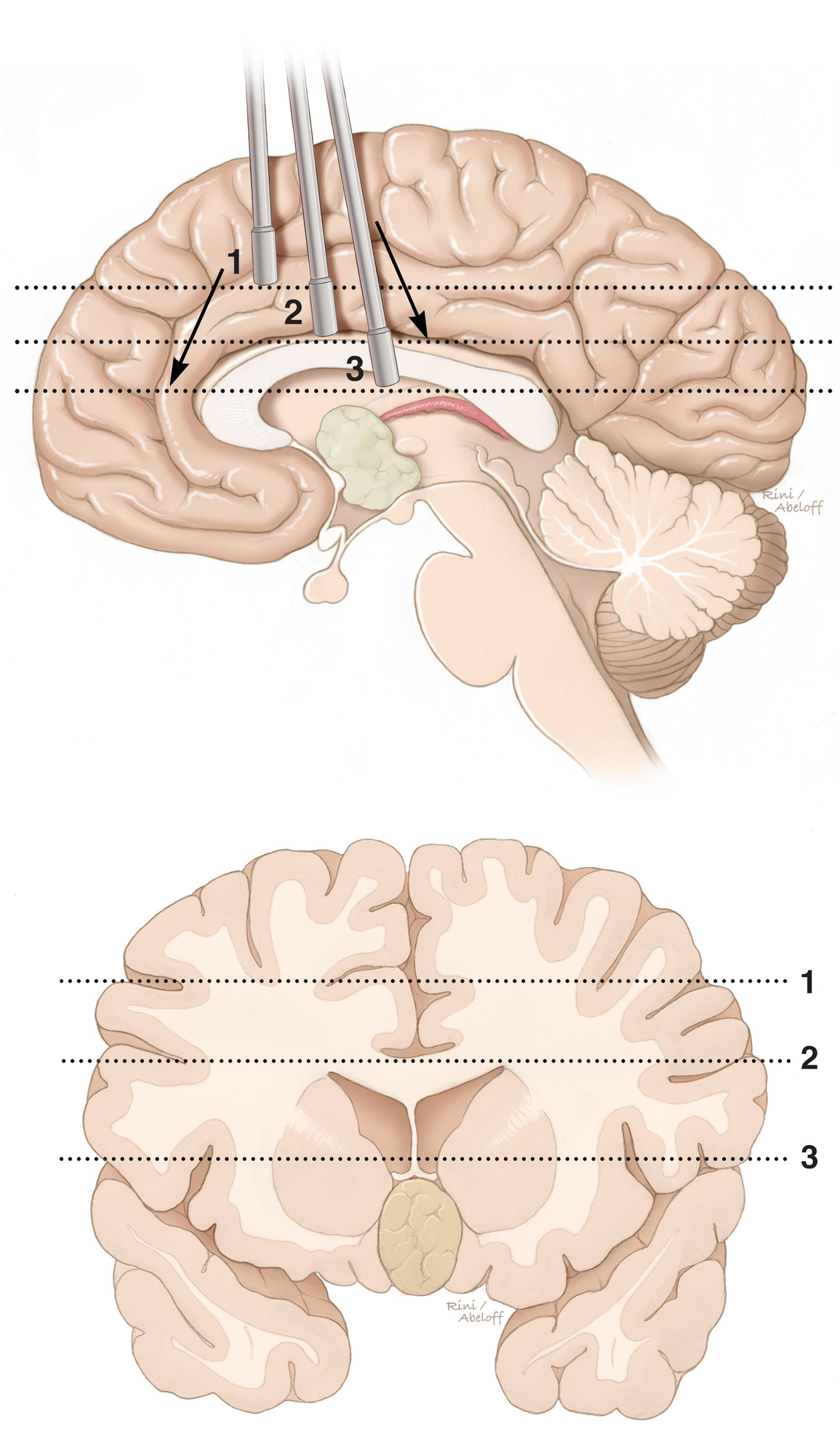
Figure 2: A coronal non-operative view of the surgical trajectory for the interhemispheric corridor toward the midline deep surgical targets is demonstrated. Important landmark structures include the cingulum (1), corpus callosum (2) and fornices (3). The cerebrovascular structures in each dissection level should be carefully preserved. The diencephalic deep veins are of special importance to avoid surgical morbidity.
Click here to view the interactive module and related content for this image.
Figure 3: The venous anatomy around the coronal suture. The parasagittal veins are sparse anterior to the coronal suture. Therefore, an interhemispheric craniotomy, mostly anterior to the suture, avoids these important veins. A large bridging vein just posterior to this suture drains the frontal lobes (Images courtesy of AL Rhoton, Jr).
Click here to view the interactive module and related content for this image.
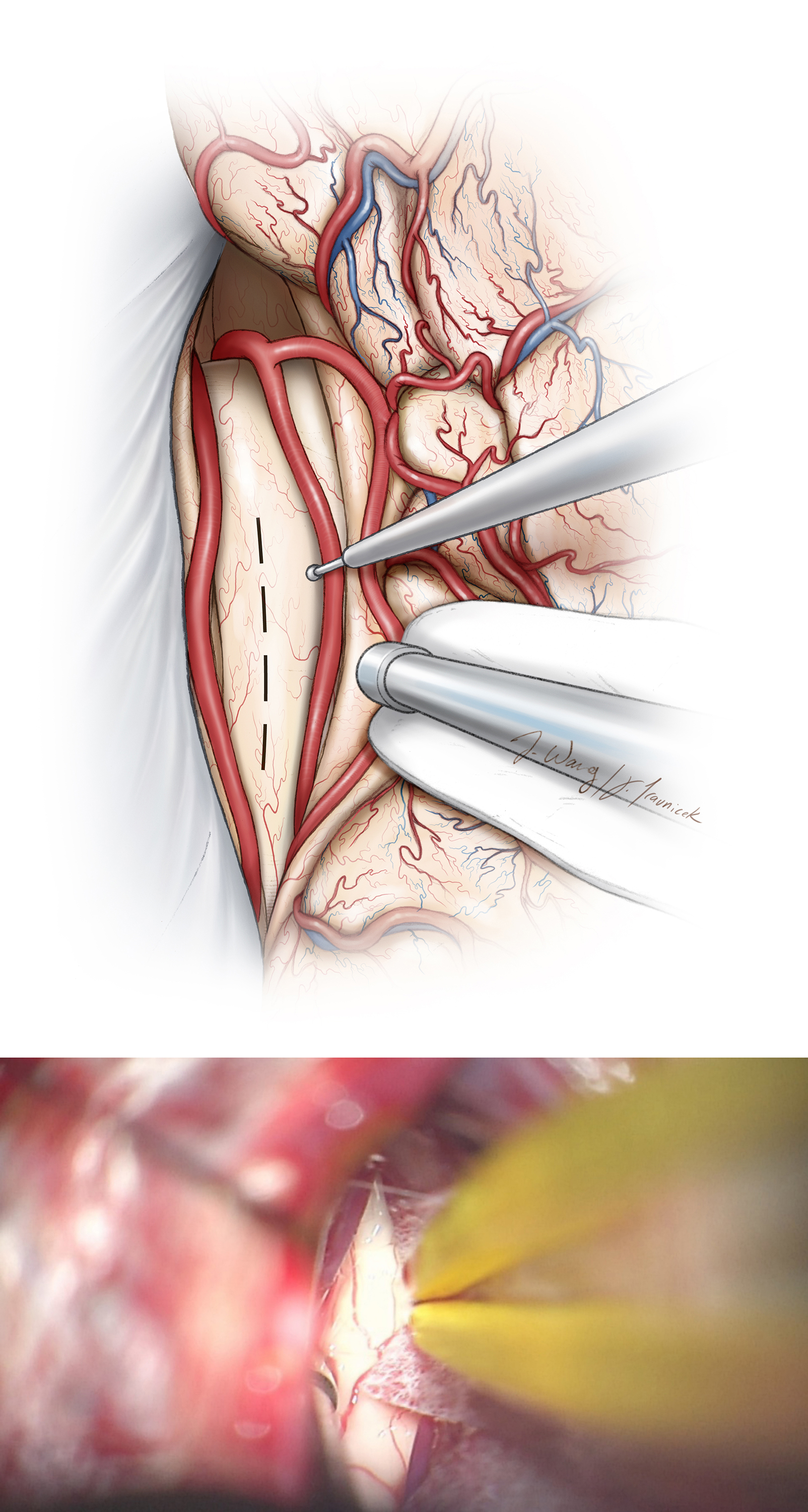
Figure 4: Superior view of the interhemispheric fissure. The right frontal lobe is retracted laterally to expose the bilateral distal anterior cerebral artery (A.C.A.) branches and the corpus callosum, which is bright white compared with the cingulate cortex (upper images). The cortices of bilateral cingula can be very adherent to each other and may be mistaken for the corpus callosum.
The callosomarginal artery may be used as a road map to reach the pericallosal arteries. Notice that this view (left lower image) was achieved without sacrificing any bridging veins, but instead through untethering them from their surrounding arachnoid membranes. Callosotomy allows exposure of the ventricle (right lower image)(Images courtesy of AL Rhoton, Jr).
INTERHEMISPHERIC CRANIOTOMY
Figure 5: The patient may be placed supine or in the lateral position. The supine position more readily orients the operator to the midline structures (right lower image), whereas the lateral position (left lower image) allows gravity retraction to mobilize the dependent (ipsilateral) hemisphere. In the case of a pericallosal aneurysm, the patient’s head is extended to achieve proximal control between the anterior communicating artery and the genu of corpus callosum. In the case of a tumor, the lesion should be positioned as high as possible within the operative field.
Figure 6: A slightly flexed neck position is reasonable for a pericallosal aneurysm just above the level of the genu (left image). The location of the lesion in relation to the genu determines the degree of neck extension. A colloid cyst at the foramen of Monro is accessible through the transcallosal approach (right image). The transcallosal route provides a panoramic view of the choroid plexus and internal cerebral and thalamostriate veins.
Figure 7: For the anterior interhemispheric approach, the skin incision is made in a curvilinear (blue) or horseshoe (green) fashion behind the hairline. The location of the linear incision is determined by the exact location of the lesion. The horseshoe incision is one-third behind and two-thirds anterior to the coronal suture and crosses the midline. Bone removal over the superior sagittal sinus will allow lateral mobilization of the sinus using retraction sutures in the falx to expand the interhemispheric corridor. For larger tumors, a U-shaped incision is more appropriate. Notice the location of the pins of the skull clamp.
Figure 8: A right paramedian craniotomy is outlined for pericallosal aneurysms (left image) or may be applied for intraventricular tumors (right image). Neuronavigation is helpful in planning the craniotomy and callosotomy. Note that the burr holes are placed on the venous sinus, and the width of the sinus is partially exposed to allow gentle rotation of the dural sinus after dural opening.
Figure 9: After I complete two burr holes over the sinus, I use a #3 Penfield dissector to generously separate the dura from the inner table of the calverium underneath the craniotomy and especially over the sinus. The final bone cut is made along the sinus to allow timely elevation of the flap if injury to the sinus occurs. Large strips of surgicel or gelfoam should be available to cover the sinus for hemostasis. Cerebrospinal fluid drainage through the lumbar drain allows the sinus and dura to fall away from the inner table of the skull and prevents unintentional sinus injury or durotomies.
Figure 10: The dura is opened in a U-shaped flap based on the sagittal sinus (top image-supine position). Retraction sutures in the superior falx rotate the venous sinus laterally and expand the interhemispheric reach. Some small bridging veins may be sacrificed, but the larger ones should be preserved. Note that gravity retraction facilitates mobilization of the dependent hemisphere away from the midline (bottom image-lateral position).
Figure 11: The subdural portion of the dissection is completed along the falx and the ipsilateral callosomarginal artery is traced along the midline to the level of the cingulum (top image). This artery will define the midline dissection planes so the surgeon can avoid subpial injury to the adherent cortices of the cingula through meticulous and sharp microsurgical techniques (bottom image).
Figure 12: Note the difference in color between the cingulate gyrus (small arrow) and the corpus callosum (large arrow). Very adherent cingulate cortices may be mistaken as corpus callosum. The corpus callosum is glistening white and stands out from the surrounding cortical tissue. Releasing CSF from the lumbar drain will ease this interhemispheric dissection. The operator should watch for the pericallosal arteries and avoid inadvertently injuring them with the tip of the microscissors.
Figure 13: The corpus callosum is widely exposed in the midline between the paired pericallosal arteries. Adherent arachnoid membranes of the cingula are sharply and widely split anteriorly and posteriorly to minimize retraction on the medial hemispheres. At times, pericallosal arteries may be displaced to one side or they may also adhere together, making their separation difficult.
Figure 14: In the case of a colloid cyst, a 1.5-cm callosotomy will provide wide visualization of the foramen of Monro and the choroid, internal cerebral, and thalamostriate veins. Neuronavigation guides the precise location of the callosotomy. If the septum pellucidum herniates into the operative field and obstructes intraventricular viewing, its fenstration will relieve this herniation and clear the view. This herniation is caused by biventricular obstruction at the level of the foramen of Monro.
Figure 15: The roadmap through the interhemispheric trajectory toward the midline chambers is demonstrated. Note the sagittal perspective in the above image. It is easy for the surgeon to become disoriented and travel too anteriorly or posteriorly (arrows) along the interhemispheric space. Navigation can keep the surgeon on track. The hashed lines correspond to the landmark levels of dissection in the coronal illustration (bottom image). These levels include the cingulum (1), corpus callosum (2) and fornices (3). If the surgeon is not directing the center of dissection toward the surgical target, additional disruption of normal tissues is later necessary for re-directing the center of dissection.
Hemorrhagic Colloid Cyst: Transcallosal Interforniceal Approach
Figure 16: If the contralateral hemisphere must be accessed, I make a T-shaped incision within the falx and reflect the falcine flaps using stay sutures (inset image). This cross-court trajectory (green arrow) expands the lateral operative angles. The above sketch shows the posterior interhemisperic transfalcine transprecuneus approach for reaching lesions within the atrium.
The Posterior Interhemisperic Transfalcine Transprecuneus Approach for Reaching Lesions within the Atrium
Closure
Once hemostasis is achieved, the dura is closed in a watertight fashion. Surgicel or gelfoam on the superior sagittal sinus should not be removed. A ventricular catheter may be required briefly during the postoperative period to clear ventricular debris if the ventricles were entered during surgery.
Postoperative Considerations
Patients are observed in the Intensive Care Unit for 1 or 2 days before they are transferred to the wards. Hypertension and overmedication with narcotics must be avoided. The ventriculostomy catheter is usually removed on the 2nd postoperative day.
Pearls and Pitfalls
- Placement of the patient in the lateral position during surgery is advantageous for gravity retraction, but may disorient some operators regarding the normal ventricular anatomy.
- Extension of the craniotomy across the superior sagittal sinus allows placement of retraction sutures along the superior falx and gentle rotation of the venous sinus to expand the interhemispheric operative corridor.
- Meticulous and sharp microsurgical maneuvers will enable the surgeon to avoid subpial injury to the cortices of the cingula. Aggressive retraction must be avoided by obtaining CSF drainage through a lumbar drain or a ventriculostomy catheter.
References
Lawton M. Seven Aneurysms: Tenets and Techniques for Clipping. New York: Thieme Medical Publishers, 2011.
Pires de Aguiar PH, Tahara A, Maldaun MV, Agner C. Falx meningiomas, in DeMonte F, McDermott M, Al-Mefty O (eds): Al-Mefty’s Meningiomas, 2nd ed. New York: Thieme Medical Publishers, 2011.
Rhoton AL Jr. The lateral and third ventricles. Neurosurgery 51(Supp 1)S207-271, 2002.
Please login to post a comment.