Extradural Clinoidectomy Free
This is a preview. Check to see if you have access to the full video. Check access
Extradural Clinoidectomy: Expanding the Paraclinoid Space
General Considerations
Anterior clinoidectomy is an important tool for neurovascular and skull base surgery. This technique is cardinal for expanding access to the proximal carotid artery, optic nerve, sella and the central skull base. The goal of anterior clinoidectomy is to reveal the more proximal ophthalmic and clinoidal segments of the internal carotid artery (ICA) while skeletonizing the proximal optic nerve. This maneuver expands the optico-carotid and carotid-oculomotor windows and therefore the operative corridor to the interpeduncular cisterns—both the carotid artery and optic nerve are partially untethered or liberated and can be more safely mobilized.
Controversy surrounds the value of clinoidectomy for “appropriately selected” cases. Moreover, there is no consensus on the indications and benefits of an extradural versus intradural clinoidectomy. Many modified variations of this osteotomy have complicated its technical complexity and further dampened some surgeons’ enthusiasm for adopting this technique. This chapter aims to clarify and simplify the appropriate indications for clinoidectomy.
The indications and advantages of an extradural clinoidectomy are:
- The extradural space allows a more “aggressive” osteotomy of the medial sphenoid wing and clinoid while protecting the intradural neurovascular structures during drilling.
- This maneuver is less selective and more inclusive for some pathologies.
- It is more beneficial for resection of medial sphenoid wing meningiomas as it allows devascularization of the tumor and decompression of the optic nerve early in the surgery. The tumor-infiltrated clinoid can be removed. With early decompression of the nerve, further tumor manipulation may not place the nerve at risk of traction injury.
- This maneuver is also used as part of the extradural middle fossa approach to the lesions of the cavernous sinus.
The indications and advantages of the intradural clinoidectomy are:
- The intradural clinoidectomy allows a relatively limited osteotomy of the clinoid process while the intradural structures are at risk during drilling and exposed to bone dust.
- This maneuver is more selective and the osteotomy can be tailored to the underlying pathology.
- This procedure is desirable for clip ligation of ophthalmic and paraclinoid artery aneurysms because bone removal can be tailored while carefully monitoring the aneurysm to prevent manipulations that could potentially place the aneurysm at risk of intraoperative rupture. A partial clinoidectomy may also be necessary for proximal posterior communicating artery aneurysms.
An intradural clinoidectomy may be associated with a smaller risk of cerebrospinal fluid (CSF) rhinorrhea for two reasons. First, by performing an early intradural inspection of the pathoanatomy, a clinoidectomy may be deemed unnecessary. Second, a partial clinoidectomy tailored to the pathology at hand may obviate the need for a complete clinoidectomy. These two factors may lead to a decreased need for osteotomy and subsequent violation of the sphenoid and even the ethmoid sinuses. The risk of oculomotor nerve injury may also be slightly decreased with extradural clinoid resection. This difference may be due to medial bone removal early in surgery during an intradural versus extradural clinoidectomy.
Ultimately, the surgeon’s preference and comfort level dictate which side of the dura is entered to execute an anterior clinoidectomy. I prefer the extradural approach because of my experience level with this procedure. I also prefer to avoid drilling within the intradural space if possible to minimize the risk of injury to neighboring structures.
Preoperative Considerations
A lumbar drain is recommended for an extradural clinoidectomy since early intradural CSF decompression for mobilization of the dura is impossible during this procedure. The extent of aeration of the clinoid (pneumatized clinoid) may be evaluated on a preoperative computed tomography (CT) scan and predicts the need for more robust plugging of the bony defect after the clinoidectomy to avoid a CSF fistula.
Clinoid pneumatization is the most frequently encountered anatomical variation of the anterior clinoid process in up to 28% of the patients scheduled for paraclinoid aneurysm surgery. Pneumatization occurs through paranasal sinus extensions into the anterior clinoid process, such as the ethmoid sinus over the anterior root, the sphenoid sinus over the optic strut or both. By far, pneumatization over the anterior root is the most frequently encountered. Furthermore, it can be observed uni- or bilaterally.
Besides investigating clinoid pneumatization, thin-slice bone window CT scan is useful to identify ossification of the clinoidal ligaments, specially the carticoclinoid and the interclinoid ligaments. In the first case, a complete or incomplete bony ring is formed with an osseus bridge from the tip of the anterior to the middle clinoid process, which is referred to as caroticoclinoidal foramen (CCF). CCFs occur in up to 17% of the patients, either uni- or bilaterally.
On the other hand, the ossification of the interclinoid ligament generates the interclinoid osseus bridge (IOB). IOB is the least frequent anatomical variation of the anterior clinoid process with an estimated occurrence of 2.8%. Removal of the anterior clinoid process in such situations is extremely demanding and a combined extradural and intradural clinoidectomy is advised in order not to severe the internal carotid artery or even the optic or oculomotor nerves.
Adherence of the aneurysm dome to the dura overlying the clinoid is a contraindication for an extradural clinoidectomy. In addition, both erosion of the clinoid by the aneurysm dome and the presence of the carotidoclinoid foramen demand an intradural technique.
Extension of the aneurysm neck proximal to the outer dural ring should be assessed on a preoperative CT angiogram. Although following clinoidectomy, opening of the outer dural ring provides access to an additional few millimeters of the aneurysm neck, significant extension of certain types of paraclinoid aneurysm necks into the cavernous sinus preclude the use of an open microsurgical route for clip ligation.
Figure 1: A coronal CT angiogram demonstrates the need for a clinoidectomy to expose the neck of this ophthalmic artery aneurysm. The neck may be partially eroding through the clinoid but the dome is not involved.
Figure 2: Medial sphenoid wing meningioma and associated hyperostosis (tumor-infiltrated) clinoid on MR (black arrow) and CT (white arrow) imaging.
Operative Anatomy
The frontotemporal dura defines the superior and lateral borders to the clinoid, whereas the periorbita and optic strut limit the anterior and inferior borders. The clinoid segment of the internal carotid artery (ICA) provides the posterior limit inferomedially. Inferolaterally, the neurovascular structures of the cavernous sinus lie under a layer of periosteal dura that emerges anteriorly into the superior orbital fissure.
The corresponding dural elements in the region related to the anterior clinoid include the falciform ligament, the distal dural ring, and the carotid-oculomotor membrane. The distal ring defines the border at which the ICA enters the intradural compartment. The plane of this ring slants downward from anterior to posterior and in a lateral to medial directions. The diverticulum medial to the ICA created by this slant is called the carotid cave. The falciform ligament and distal dural ring may be incised to liberate the optic nerve and the ICA, respectively.
The oculomotor nerve travels within the superalateral wall of the cavernous sinus and courses anteriorly just below the anterior clinoid process to enter the superior orbital fissure. Therefore, significant manipulation of the anterior clinoid process during its removal in this inferior direction should be avoided.
Click here to view the interactive module and related content for this image.
Figure 3: Sequential photographs of the clinoid and sellar region demonstrating the osseus relationships of the anterior clinoid process. In D, a superior view shows a complete interclinoid bridge on the left side (Intercl. Bridge) and a complete caroticoclinoidal foramen (Caroticoclin. For.) on the right side of the specimen (red arrow). Ant.: anterior; Car.: carotid; Clin.: clinoid; Em. V.: emissary vein; Fiss.: fissure; For.: foramen; Gr.: greater; Lac.: lacrimal; Less.: lesser; Mid.: middle; Orb.: orbital; Pit.: pituitary; Post.: posterior; Sphen.: sphenoid; Sulc.: sulcus; Sup.: superior; Tuberc.: tuberculum sellae (Images courtesy of AL Rhoton Jr).
Figure 4: A detailed view demonstrates the relationships of the anterior clinoid to the clinoidal ligaments. A complete caroticoclinoidal foramen is identified on the left side, together with an ipsilateral incomplete interclinoid bridge. The tip of the anterior clinoid process (red) has a bridge (green) that connects it to the middle clinoid process (yellow). The osseous spike displayed in blue represents the incomplete interclinoid bridge connected to the posterior clinoid process. Ant.: anterior; CCF: caroticoclinoidal foramen; Interclin.: interclinoidal.(Images courtesy of AL Rhoton Jr.)
Figure 5: Thin-slice CT (bone window) of an incomplete caroticoclinoidal foramen (white arrow) and also an incomplete interclinoidal bridge (yellow arrow) in a patient affected by a medial sphenoid wing meningioma is demonstrated.
Click here to view the interactive module and related content for this image.
Figure 6: The view gained by a clinoidectomy. Note the extended view of the clinoidal segment of the ICA (left image). The proximity of the optic nerve to the clinoid places it at risk during drilling. The superior and lateral borders of the clinoid space are provided by the frontotemporal dura. The periorbita, optic strut, and sphenoid bone are the anterior and inferior limits.
The relationships of other relevant vital structures (note the cranial nerves within the lateral wall of the cavernous sinus) are presented after other overlying dura and bone are removed (right image). These vital structures are at risk during mobilization of the process (Images courtesy of AL Rhoton, Jr).
Given the large number of neurovascular structures in this region, the importance of any additional space through mobility of any nerves or key vessels is immediately apparent for operative access. A major impediment to learning this technique is a lack of three-dimensional understanding of the clinoid and the surrounding vital structures. I will attempt to simplify the germane operative anatomy.
The following images emphasize three osteotomies required for disconnection of the clinoid:
- Osteotomy along the medial sphenoid wing to disconnect the lateral connection
- Osteotomy along the orbital roof to disconnect the anterior and medial connections
- Drilling within the clinoid to create an “egg shell” and disconnect the anteroinferior connection to the optic strut
After the completion of the above three steps, the shell of the clinoid can be mobilized and dissected away from the clinoidal ligaments.
At the level of the superior orbital fissure, the outer and inner layers of the lateral wall of the cavernous sinus are distinguishable and can be bluntly and gently dissected from each other. The inner layer contains the cranial nerves, and the outer layer is formed by the temporal fossa dura. Near the superior orbital fissure, the periosteal layer of the dura is in continuity with the periosteal layer of the periorbita. Therefore, the dural fold along the lateral edge of the superior orbital fissure appears as a periosteal layer formed by the fusion of the periorbital and temporal dura.
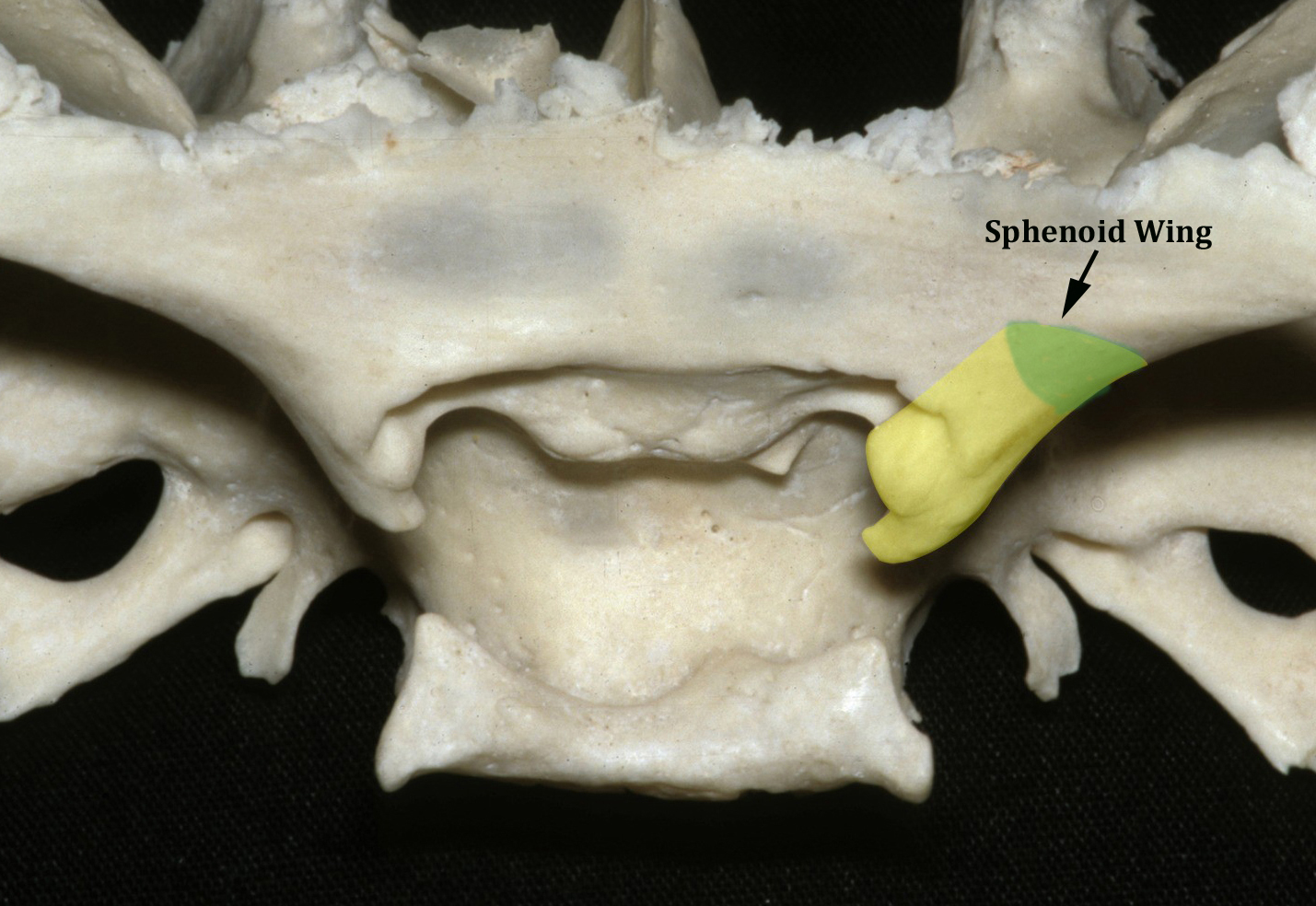
Figure 7: The first step involves an osteotomy along the medial sphenoid wing to disconnect the lateral connection of the clinoid and skeletonize the superior orbital fissure (shown in green)(Image courtesy of AL Rhoton, Jr).
Figure 8: The second step involves an osteotomy along the roof of the optic nerve and frontal bone medially (shown in pink) to disconnect the anterior and medial connections of the clinoid. This decompression of the nerve protects the nerve from any traction injury during mobilization of the clinoid. The last osteotomy involves drilling within the clinoid to create an “egg shell” and disconnect the anteroinferior connection to the optic strut (shown in green)(Images courtesy of AL Rhoton, Jr).
EXTRADURAL ANTERIOR CLINOIDECTOMY
Extradural clinoidectomy follows a pterional or orbitozygomatic craniotomy. I often use extradural anterior clinoidectomy in conjunction with extended pterional craniotomy. Please refer to the Orbitozygomatic Craniotomy chapter for further details regarding incorporation of extradural clinoidectomy in this skull base approach. For the use of clinoidectomy for aneurysms, please refer to the paraclinoid aneurysm chapter.
Figure 9: A standard extended pterional craniotomy has been completed. The pterion, and the greater and lesser sphenoid wings are resected and only a thin cortical bone covers the periorbita. Next, the dura is elevated from the posterior roof of the orbit to allow mobilization of the frontal dura over the clinoid. The dura is progressively mobilized away from the medial sphenoid wing toward the anterior clinoid process.
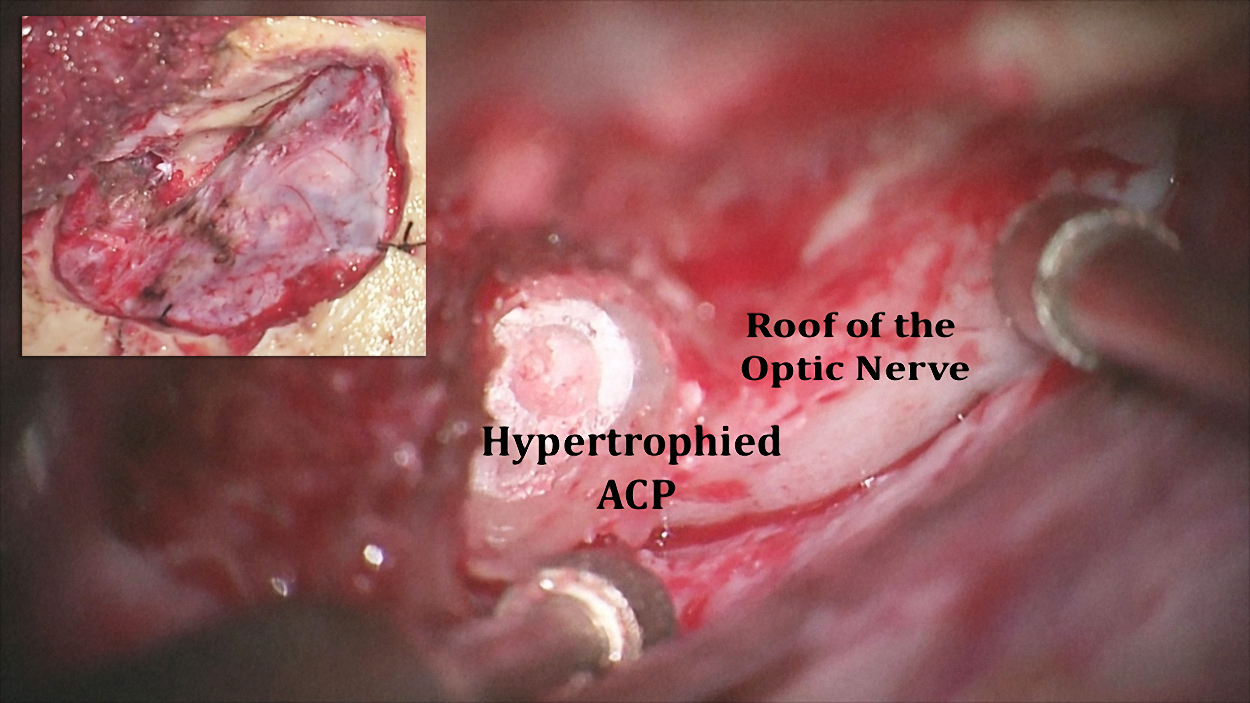
Figure 10: The extended pterional craniotomy and drilling of the orbital roof are demonstrated (inset image). Upon resection of the lesser sphenoid wing, the left hypertrophied anterior clinoid process (ACP) in a patient with a medial sphenoid wing meningioma is apparent.
Figure 11: Upon mobilization of the dura over the medial sphenoid wing, further progress to expose the clinoid is interrupted due to tethering of the dura over the superior orbital fissure by the lateral frontotemporal dural fold (also referred to as the orbitotemporal periosteal fold) containing the meningoortbital band (inset image). I section this band for ~5mm. I then bluntly elevate the temporal fossa dura away from the lateral wall of the cavernous sinus along the superior orbital fissure near the sphenoid ridge. This key maneuver reveals a cleavage plane between the temporal fossa dura and a thin layer of connective tissue covering the superior orbital fissure.
Once the orbitotemporal periosteal fold is sectioned, the orbitomeningeal artery is identified, coagulated, and severed. The lacrimal nerve travels just medial to this cleavage plane; the cranial nerves within the cavernous sinus are also just medial to this nerve. Therefore, sectioning of the orbitotemporal periosteal fold beyond 5mm should be avoided. Cerebrospinal fluid drainage through the lumbar drain obviates the need for fixed retractors on frontal and temporal lobes.
Figure 12: Using blunt dissection, I extend the cleavage plane between the temporal fossa dura and the inner layer of the lateral wall of the cavernous sinus. This maneuver allows excellent exposure of the posterior aspect of the clinoid process. Osteotomy of the medial portion of the sphenoid wing disconnects the clinoid from its lateral attachment (inset; the region of osteotomy is shown in red).
Figure 13: Before the clinoid process is manipulated, the dorsal and lateral walls of the optic canal are unroofed using a small diamond drill under continuous irrigation to avoid heat injury to the nerve. The cortical bone over the nerve is “egg-shelled” and a fine curette is used to remove this thin layer of bone (left inset image). Direct drilling over the nerve is prohibited. This osteotomy (right inset image, red) disconnects the process from its frontal attachment and avoids compression or traction injury on the nerve during manipulation of the clinoid.
The suction apparatus maintains dynamic retraction on the dura.
Figure 14: With a clear view of the optic nerve, I use the diamond burr to core out the central cancellous bone and “egg-shell” the remaining cortical bone of the clinoid process. This maneuver disconnects the final attachment of the process to the optic strut (inset image). The cranial nerve III should be protected during anterolateral drilling.
Figure 15: The remaining shell of the clinoid is fractured by a curette and delivered. Careful blunt dissection and manipulation of this remaining portion is often required for its release from the inter- and petroclinoid ligaments. A clear view of the optic nerve allows the surgeon to avoid injuring it. A pituitary rongeur is used to pull out the loose fragment (lower left inset image). Venous bleeding from the cavernous sinus is easily controlled by judicial packing of thrombin-soaked gelfoam. Overpachking is not advised so that the additional space gained by the clinoidectomy is not obliterated.
Figure 16: Completed view of an extradural anterior clinoidectomy with localization of the clinoidal ICA through the dura. An intradural view of the extent of bony removal is evident (inset image). During the subsequent intradural portions of the operation, the falciform ligament and the distal dural ring can be transected to liberate and mobilize the optic nerve and carotid artery at the skull base, respectively.
Figure 17: Intraoperative photo demonstrates the extradural exposure of the left optic nerve after clinoidectomy (top image). Intradural transection of the falciform ligament reveals the length of the optic nerve as it enters the orbit (bottom image). The area of compression and discoloration of the nerve by the ligament is apparent (*).
Resection of a Hypertrophied Clinoid Process
Closure
If there is concern about a pneumatized anterior clinoid process, a small piece of temporalis muscle may be placed within the clinoidectomy bony defect and reinforced with fibrin glue after dural closure.
Postoperative Considerations
The patient is monitored for CSF rhinorrhea, changes in visual acuity, and diplopia. Postoperative rhinorrhea is first managed by temporary lumbar drainage. This maneuver is often effective for cessation of the leak. If this is not effective, the patient is returned to the operating room for repacking of the clinoidectomy defect.
Pearls and Pitfalls
- Be aware of clinoid pneumatization and ligament ossification before deciding to complete a clinoidectomy.
- I section the lateral orbitotemporal periosteal fold for ~5mm. I then bluntly elevate the temporal fossa dura away from the lateral wall of the cavernous sinus along the superior orbital fissure near the sphenoid ridge. This maneuver provides an excellent view of the clinoid process and is the key maneuver in execution of a clinoidectomy.
- Egg-shelling the clinoid process is a safe method of clinoidectomy.
- The oculomotor nerve courses immediately below the anterior clinoid process and can be easily injured in removing the lower edge and posterior tip of the clinoid.
- Excessively hyperostotic tumors make drilling a tedious endeavour: I suggest an intradural clinoidectomy in these cases.
- En bloc resection of the clinoid process should be avoided.
Contributor: Marcus A. Acioly, MD, PhD
References
Kattner KA, Fukushima T. Management of vascular invasion during radical resection of medial sphenoid wing meningiomas. Skull Base. 2001;11(2):99-104.
Kulwin C, Tubbs RS, Cohen-Gadol AA. Anterior clinoidectomy: Description of an alternative hybrid method and a review of the current techniques with an emphasis on complication avoidance. Surg Neurol Int. 2011;2:140.
Lehmberg J, Krieg SM, Meyer B. Anterior clinoidectomy. Acta Neurochir (Wien). 2014 Feb;156(2):415-419.
Ota N, Tanikawa R, Miyazaki T, Miyata S, Oda J, Noda K, Tsuboi T, Takeda R, Kamiyama H, Tokuda S. Surgical microanatomy of the anterior clinoid process for paraclinoid aneurysm surgery and efficient modification of extradural anterior clinoidectomy. World Neurosurg. 2015;83(4):635-643.
Rhoton AL Jr. Aneurysms. Neurosurgery. 2002;51(Suppl 4):1-S121-158.
Rhoton AL Jr. The cavernous sinus, the cavernous venous plexus, and the carotid collar. Neurosurgery. 2002;51(4 Suppl):S375-410.
Please login to post a comment.