High Flow Revascularization
This is a preview. Check to see if you have access to the full video. Check access
Giant ICA Bifurcation Aneurysm: Radial Artery Bypass
Please note the relevant information for patients undergoing cerebral bypass surgery is presented in another chapter. Please click here for patient-related content.
The advent of microneurovascular techniques began in the early 1960s when Woringer reported the first high-flow (HF) extracranial-intracranial (EC-IC) bypass procedure. Although Woringer's technique was not initially popularized because of its complexity and the associated high morbidity, his progress was a major evolution in the field of cerebral revascularization.
It was not until the early 1970s when further medical and surgical advancements renewed interest in this form of vascularization. In 1971, William Lougheed performed a common carotid artery (CCA) to intracranial internal carotid artery (ICH) bypass with an interposition saphenous vein graft. His success paved the way for other surgeons to refine its use for treatment of cerebral aneurysms, ischemic vascular disease, and skull base tumors.
Because of its technical complexity and limited surgical indications, EC-IC bypass is infrequently performed, even in modern day neurosurgery. There are numerous considerations for performing an EC-IC bypass, including optimal patient selection, technical performance, selection of the appropriate bypass procedure, and the individual patient’s anatomic constraints.
Classification of Revascularization Techniques
Cerebral revascularization has been described as involving almost every intracranial artery. In general, these techniques are classified as either low-flow or high-flow EC-IC, or IC-IC (in situ) bypasses. The indications for a particular technique are based on the anticipated recipient’s demand of cerebral blood flow, as well as the availability of an appropriate donor source. Low-flow donor vessels provide less than 50 mL/min (15–25 mL/min) of blood flow to the recipient vessel, while high-flow conduits provide more than 50 mL/min (70-140 mL/min) of blood flow.
Examples of a low-flow technique include the use of the superficial temporal artery (STA) or occipital artery (OA) as donor vessels to anastomose with and support various medium-size intracranial recipient arteries. One such example is STA to distal middle cerebral artery (MCA) (STA-MCA) anastomosis, although other recipient arteries, such as the distal superior cerebellar artery (SCA) or posterior cerebral artery (PCA), have also been used.
The STA-MCA bypass is the most widely used revascularization technique and is discussed in its own chapter. In situ, IC-IC bypasses are typically low flow and are especially favored during complex aneurysm surgery involving the anterior cerebral artery (A3-A3) and posterior inferior cerebellar artery (PICA-PICA). In situ bypasses have the advantages of using caliber-matched donor and recipient arteries, along with a relatively short graft that remains protected inside the cranium.
High-flow bypasses utilize larger caliber donor vessels with interposition grafts (usually nondominant radial artery or saphenous vein) and promote reliable flow replacement rather than augmentation (low-flow bypass). An example of a high-flow bypass involves a radial artery interposition graft, anastomosing the external carotid artery (ECA) branch with one of the M2s.
Indications for Revascularization
Cerebrovascular revascularization surgery is performed for two main general indications:
- Flow augmentation to treat refractory chronic cerebral ischemia in patients with Moyamoya disease or severe intracranial atherosclerosis
- Flow replacement when treating complex cerebrovascular pathology or skull base tumors requiring acute vessel sacrifice.
Low-flow bypasses are typically performed in cases of flow augmentation, whereas high-flow bypasses are used for flow replacement.
Although there is a seemingly sound neurophysiologic basis for the use of cerebral revascularization techniques, there is no class I evidence to support the use of EC-IC or IC-IC bypass for any indication. Moreover, there is a body of literature (EC-IC Bypass Study and the Carotid Occlusion Surgery Study) that suggests cerebral revascularization may have high morbidity and mortality, especially in inexperienced hands; therefore, current indications for bypass procedures remain relatively limited and controversial.
Despite unfavorable results from the aforementioned studies, the modern indications for high-flow EC-IC bypass include vessel sacrifice during intracranial aneurysm clip ligation procedures or complex skull base tumor resections, necessitating moderate to large size vessel sacrifice.
Complex Cerebral Aneurysms
Complex cerebral aneurysms include those that are giant (with aberrant branches originating from the wall of the aneurysm), multilobed, wide-necked, fusiform, calcified, or dolichoectatic. This subset of aneurysms are classified as such because of their atypical pathoanatomy that precludes successful treatment with primary microsurgical clip ligation or endovascular embolization techniques, in contrast to their saccular counterparts.
Successful aneurysm clip ligation requires surgical access to the aneurysm neck, preparation of the proximal vessel(s) for vascular control, preservation of the essential perforators and distal arterial branches, and a pliable and relatively distinct aneurysm neck that can be collapsed using clip blades.
These basic tenets of aneurysm surgery cannot be implemented for complex aneurysms that necessitate sacrifice of some of the parent or branching vessels. Endovascular techniques are also less successful in aneurysms with wide necks where outflow arteries are incorporated into the aneurysm wall. Cerebral revascularization may remain the last resort.
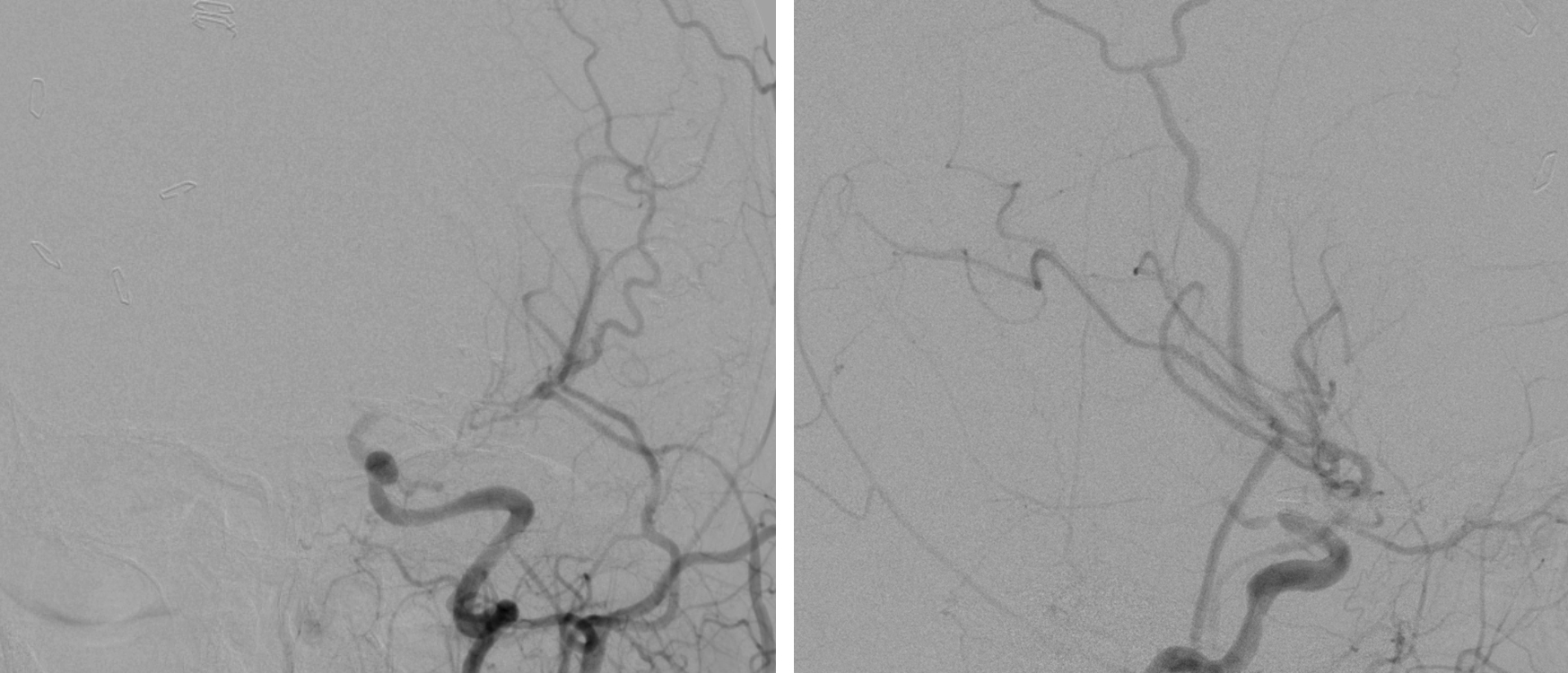
Figure 1: A 6-cm partially thrombotic and calcified left ICA bifurcation aneurysm is shown. Traditional clip ligation methodologies are not effective. This patient underwent a high-flow extracranial ICA-M2 bypass and Hunterian ligation of the ICA distal to the anterior choroidal artery. The flow into the aneurysm sac via the ipsilateral A1 was also clip occluded. Please see the intraoperative photos below for my surgical findings in this case.
Skull Base Tumors
In rare cases, skull base tumors encase neighboring arteries and require sacrifice of a major vessel to allow gross total tumor resection. The carotid artery is the most common vessel evaluated for sacrifice because of its strategic location within the skull base.
A relatively large subset of patients may tolerate carotid vessel occlusion and pass the balloon test occlusion (BTO). Despite favorable results from the BTO, up to 30% of patients still suffer from postoperative ischemia after carotid sacrifice. Revascularization is often performed prior to surgical or endovascular parent vessel occlusion to reduce these risks.
I employ revascularization exceedingly rarely for resection of skull base tumors because the risks outweigh the benefits. Most of these tumors are benign, and the residual tumor is amenable to radiosurgery.
Post-Traumatic Dissections and Pseudoaneurysms
Intracranial dissections and pseudoaneurysms may form spontaneously or after a traumatic event. Refractory or persistent cases of intracranial dissection or pseudoaneurysm not responsive to conservative therapy or amenable to endovascular treatment may require parent vessel sacrifice to reduce the risk of stroke or subarachnoid hemorrhage.
Although bypass for intracranial dissections and pseudoaneurysms is an effective treatment, newer endovascular stenting techniques have limited its application.
Athero-Occlusive Disease
Patients with medically refractory ischemic complications secondary to cerebral athero-occlusive disease benefit from flow augmentation. Symptoms often manifest as transient ischemic attacks or stroke, especially in patients with hypotension. Patients may present with extracranial or intracranial steno-occlusive disease, vasculitis, or Moyamoya disease.
In cases of steno-occlusive disease of the anterior circulation, EC-IC bypass may be considered for patients who fail medical and endovascular treatment. In the case of posterior circulation, and especially in vertebrobasilar occlusive disease, EC-IC bypass is often considered as a last resort.
Preoperative Graft Evaluation and Choice of Graft
Any patient scheduled to undergo an intracranial revascularization procedure should be rigorously evaluated preoperatively. This evaluation includes measuring the length and diameter of both radial arteries and saphenous veins. A Doppler ultrasound and an Allen's test assess the adequacy of ulnar collateral flow to the palmer arcades. In children under the age of 12, the radial artery diameter may be too small for intracranial use. Radial artery and saphenous vein grafts are the most effective high-flow grafts.
Although radial artery and saphenous vein grafts are used interchangeably for high flow bypasses, each has its advantages and disadvantages. Selection of the appropriate arterial or venous interposition graft typically depends on the type of the desired bypass.
Venous grafts can undergo proatherogenic changes after revascularization that may lead to a higher likelihood of graft thrombosis. Despite these theoretical risks and reports from the cardiac literature demonstrating higher patency rates of the radial artery grafts at 1 year after surgery, no such studies exist in the cerebrovascular literature.
Studies evaluating saphenous vein grafts for cerebral revascularization report patency rates of 86%, 82%, and 73% at 1, 5, and 13 years after surgery, respectively. These rates are still sufficiently high; therefore, the choice of radial artery rather than saphenous vein grafts are typically based on other considerations, such as surgeon’s preference and training bias. I prefer the radial artery grafts because they are better matched, both in caliber and wall thickness, for the medium-size intracranial arteries (M2 or P1 branches). These advantages facilitate durable distal anastomosis and reduce temporary occlusion time necessary for completion of the anastomosis.
Arterial grafts are also void of valves and varices that predispose the lumen to formation of thrombus and occlusion during manipulation. The strength of these grafts’ outer walls also minimizes the risk of torsion or kinking. The disadvantages of radial artery grafts are the potential morbidity associated with their harvest, their shorter length, and their potential association with vasospasm, which can lead to functional occlusion. Harvesting the maximal length of the radial artery is critical. Vasospasm can be prevented with calcium channel blockers or angioplasty, but remains a potential drawback of arterial grafts. The length of the radial artery graft can be the rate-limiting factor, leading to abortion of the procedure.
Saphenous vein anastomosis may be more technically difficult to perform because of its mismatch with the recipient vessel. Saphenous veins have thicker walls and larger diameters compared to the intracranial recipient vessels. In addition, there is high-flow mismatch through the graft; this phenomenon can lead to turbulent flow at the distal anastomotic site. On the other hand, it is possible to harvest up to 40 cm of a saphenous vein, more than adequate for any revascularization procedure.
Alternative high-flow grafts to the radial artery and saphenous vein do exist, but the choices are limited. A suitable graft must have an adequate vessel diameter (2-3 mm) and length of at least 20 cm. Anterior tibial artery grafts for high-flow cerebrovascular bypass have been considered. The lateral circumflex femoral artery may also be used as an alternative to the radial artery and saphenous vein. In general, these alternative vessels are more technically challenging to harvest and have higher rates of atherosclerosis, complicating their use.
Preoperative Cerebrovascular Assessment
Successful bypass surgery depends on a careful and detailed study of the collateral vessels and arterial variations within the circle of Willis and nearby the target pathology; therefore, catheter angiography is recommended for all patients scheduled for revascularization. Evaluation of the neck vessels and ECA, including superficial temporal artery, is indicated.
A balloon test occlusion (BTO) is recommended for arterial occlusion. Although BTO can assess collateral flow and tolerance to temporary occlusion, it cannot reliably predict the risk of ischemic complications after definitive or permanent arterial occlusion. However, it can confirm the need for a cerebrovascular bypass.
Tolerance to ICA occlusion is assessed after temporary endovascular balloon occlusion, during which the patient is assessed for any changes in neurologic, electrophysiologic, radiographic, or in response to provocative tests for a standard period of 15 minutes. If the patient remains neurologically intact without objective evidence of deterioration, the patient is deemed to have passed the ICA occlusion challenge.
As previously mentioned, BTO should be performed in conjunction with cerebral blood flow and hypotensive challenge studies to improve the reliability of occlusion tolerance. Patients who have a greater than 25% decrease in blood flow within the ipsilateral middle or anterior cerebral arteries after carotid occlusion are more likely to develop ischemic complications and require flow augmentation via revascularization. I recommend BTO over 30 minutes in conjunction with hypotensive challenge (mean arterial pressure reduced by 15 to 20 mm Hg) and cerebral blood flow studies (xenon computed tomography or CT perfusion). Arterial back-pressures can also be measured to indirectly assess the adequacy of collateral flow.
Patients who fail conventional BTO require high-flow EC-IC bypass. Patients who pass conventional BTO but demonstrate low back-pressures, perfusion deficits, or deteriorate with hypotensive challenge also benefit from high or low flow bypass procedures.
Newer methods for assessing cerebral blood flow via quantitative magnetic resonance (MR) angiography have also shown considerable promise. In a study of 16 patients by Charbel and colleagues, a greater than 20% decrease in blood flow through the ipsilateral MCA or ACA resulted in a 100% correlation with failure of BTO.
Preoperative Considerations
I prescribe aspirin (325 mg daily) a week before surgery to prevent postoperative graft thrombosis. I also recommend the use of a statin before surgery in patients with hypercholesterolemia because of its potential favorable effects on long-term graft patency.
Mean arterial pressures are monitored intraoperatively using a femoral artery sheath (also used for intraoperative angiography) to avoid a radial line, because both radial arteries will most likely be prepped and marked. Intraoperative neuromonitoring is instituted via electroencephalography, somatosensory evoked, motor evoked, and brainstem auditory evoked potentials. Electromyography may also be used to monitor cranial nerves that are at risk during surgery.
Brain relaxation is a crucial step in achieving the necessary wide microsurgical corridor for revascularization procedures. Mannitol (1g/kg), dexamethasone, and generous aspiration of cerebrospinal fluid are necessary to achieve adequate surgical exposure. A ventriculostomy drain or lumbar drain may also aid in brain relaxation.
Balanced neuroanesthesia is necessary. To prevent ischemic complications during temporary vessel occlusion, I recommend an increase in the fraction of inspired oxygen (FiO2) to 100%, mild hypothermia and barbiturate-induced burst suppression. Hypovolemia or hypotension should be strictly avoided. Normocapnia is maintained to avoid collateral vasoconstriction.
These measures will increase the tolerance of the brain to temporary regional circulatory arrest during anastomosis. In patients with unruptured aneurysms, systolic blood pressure is slightly increased to the upper range of normal during temporary occlusion to improve collateral perfusion.
Operative Anatomy
Bypass procedures involved steep learning curves and require expertise in neurovascular microsurgery and relevant operative anatomy.
Figure 2: Photographs of cadaveric specimens demonstrate a high-flow venous bypass (ECA/ICA–M2). The zygomatic arch is drilled to provide a conduit for the graft without its kinking. The M2 branch with the least number of side branches is temporarily trapped distal to the lenticulostriate perforating arteries. The distal anastomosis requires end-to-side technique using interrupted 8-0 or 9-0 nylon sutures (right upper photo-arrow). After completion of the intracranial anastomosis, the cervical ECA or ICA is occluded proximally and distally and the proximal end of the graft is anastomosed to the ICA in an end-to-side fashion or to the ECA in an end-to-end configuration using 7-0 nylon sutures (images courtesy of AL Rhoton, Jr).
HIGH-FLOW REVASCULARIZATION TECHNIQUE
Patient positioning during high-flow revascularization depends on the underlying location of the aneurysm and the relationship of the donor and recipient vessels. Care should be taken not to turn the patient’s neck excessively because this maneuver can potentially compress the vertebral arteries at the craniocervical junction.
If the lateral position is planned, a femoral artery sheath should be placed before turning the patient. The radial artery can be harvested with the patient in either in the supine or lateral position.
Figure 3: Patient positioning is tailored according to the location of the donor and recipient vessels, as well as the site designated for harvesting the graft. A 5-cm incision is made along the anterior edge of the sternocleidomastoid muscle to expose the internal and external carotid arteries in the neck. The interposition graft harvest, neck dissection, and craniotomy can be performed concurrently to advance operative efficiency.
Figure 4: I prefer the radial artery interposition graft for most high-flow revascularization procedures. Careful isolation and ligation of the small branches arising from this artery is imperative during its atraumatic harvest. The key component of this step is securing a graft of appropriate length to guarantee a tension-free anastomosis. I ask my peripheral vascular surgery colleagues to perform this part of the operation. Therefore, the details of the technique are not elaborated upon. Pressurized heparinized saline is used to dilate the graft (the pressure distention technique) after its extraction.
Cervical Exposure
The patient’s neck should always be prepped in preparation for an EC-IC bypass, securing proximal control. If the bypass procedure involves the extracranial carotid arteries, a 5-cm longitudinal incision should be made through the skin and platysma, along the anterior edge of the sternocleidomastoid muscle centered at the level of the carotid bifurcation.
The sternocleidomastoid muscle is then dissected free and retracted laterally to expose the carotid sheath, just medial to the jugular vein. The posterior belly of the digastric muscle and hypoglossal nerve are often encountered rostrally crossing the ICA and should be preserved.
The common facial vein may be encountered caudally and can be ligated and divided to aid in exposure of the CCA, ICA, and ECA. Each vessel should be isolated with vessel loops and exposed up to 4 cm of its length from the carotid bifurcation to permit sufficient space for anastomosis and temporary clip application. I recommend using the ECA as the site of proximal anastomosis to obviate the need for temporary ICA occlusion. However, this maneuver may lead to torsion of the graft based on the location of the ECA; in this situation, the ICA should be used.
For more technical tenets related to exposing the ICA bifurcation, please refer to the Carotid Endarterectomy chapter.
Craniotomy
A pterional craniotomy is designed based on the site of anastomosis and the underlying pathology. The craniotomy should be large enough to expose the recipient vessel and wide enough to relieve possible cerebral edema and mass effect via craniectomy.
A larger craniotomy or the addition of an orbitotomy may provide extended exposure. Careful and immaculate hemostasis must be obtained during the exposure and epidural dissection as 2000-3000 IU of intravenous heparin is often administered intraoperatively to prevent graft thrombosis.
Anastomoses
After the exposure of the donor (ECA/ICA) and recipient (M2) vessels has been completed, anastomosis may commence. The Sylvian fissure is widely split and the fontal lobe is untethered from its subfrontal arachnoid adhesions so that it can be mobilized away from the skull base.
I strongly recommend the execution of the intracranial anastomosis first to take advantage of the slack in the graft and the ability to rotate the graft during the anastomosis. The intracranial anastomosis is often more technically difficult because of the availability of the limited surgical corridor and carries the higher risk of thrombosis compared with its extracranial counterpart.
Figure 5: Immaculate hemostasis should be ensured within the surgical field. A colored background material (rubber dam) is placed under the recipient artery to provide contrast for visualization of the transparent arterial walls and to protect the underlying brain parenchyma. A drain under continuous suction and under the rubber dam may be used to keep the anastomotic site dry during liberal heparinized saline irrigation at the time of microsurgery.
Next, I mark the arteriotomy site using a sterile ink pen. The wide end of the graft is cleaned and stripped of its adventitia and then brought into the field. If saphenous vein is used, the wide end of the graft should be anastomosed with the recipient vessel to avoid valvulotomy and preserve the natural direction of blood flow within the interposition graft.
Prior to temporary occlusion (trapping) of the recipient artery (typically M2,) 2000-3000U of heparin is administered intravenously. Burst suppression is achieved via infusion of etomidate, FiO2 is increased to 100%, and blood pressure is slightly elevated to augment collateral perfusion. My goal is to keep temporary occlusion time under 30 to 40 minutes; however, this may be unachievable in more technically challenging cases, such as for the ECA-to-PCA anastomosis.
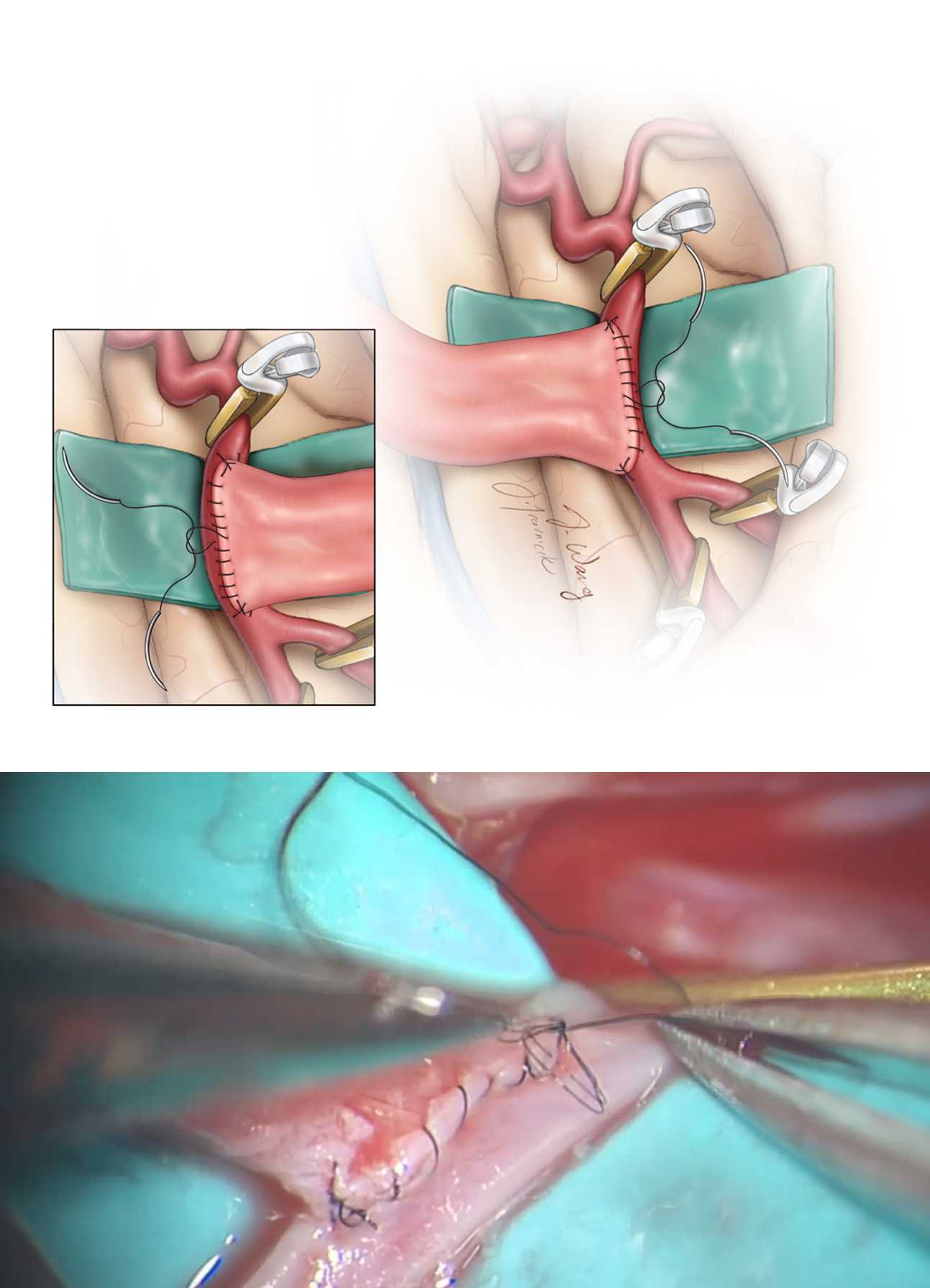
Figure 6: The recipient artery (M2) is trapped using small temporary clips; perforator-free zones, slightly distal to the sites of bifurcation, are used for obvious reasons. Next, the recipient vessel is arteriotomized with a micro-knife and the arteriotomy is lengthened using microscissors along the ink line.
The arteriotomy length should be approximately 2-3 times the diameter of the recipient vessel. The distal end of the graft’s lumen is expanded by “fish-mouthing” its opening. I use interrupted 8-0 or 9-0 nylon sutures for M2 or P2 anastomoses and 7-0 nylon sutures for proximal ICA anastomosis. Two sutures are first placed through either corners of the arteriotomy (toe and heel) to approximate and anchor the graft.
Next, the remainder of the anastomosis can be performed using a running or interrupted suturing technique. Prior to completion of the anastomosis closure, the lumens of the M2 and graft are flushed with heparinized saline. A temporary clip is placed on the graft distal to the anastomosis and flow is re-established through the recipient vessel to avoid prolonged occlusion time. Bleeding/oozing at the anastomosis is controlled using pieces of Surgicel and Gelfoam.
Figure 7: The first running suture anchors the graft to one end of the arteriotomy (heel) while a second suture anchors the graft to the other end of the arteriotomy (toe)(top illustration). The graft is flipped side to side to allow for completion of anastomosis on both walls. The loops of the sutures are then tightened before their final knot (bottom photo).
Next, the graft is tunneled over the root of the zygoma toward the cervical incision. During this step, I tunnel a hemostatic clamp through the insertion site of the temporalis muscle toward the mandibular angle, piercing through the masseter and parotid fascia, reaching the superior end of the cervical incision. A pediatric chest tube is then introduced and carried rostrally by the hemostatic clamp and serves as a rigid yet smooth tunnel for passage of the graft. The zygomatic arch may need to be drilled down to avoid kinking, twisting, or obstruction of the lumen of the graft and compromise of its flow. This drilling fashions a conduit for the graft when it is placed in the preauricular position.
Figure 8: The graft is tunneled from the cranial operative field into the cervical field using a pediatric chest tube. A notch is drilled in the zygoma before tunneling to prevent obstruction of the graft’s lumen. A slit is cut in the chest tube to allow the graft to be placed directly inside the tube; this landmark also maintains and confirms the alignment of the tube during its passage and prevents the graft from twisting. The tube is pulled through from the cervical field and the graft is removed from the tube.
The proximal anastomotic site is also prepared in a similar fashion with a colored background and drain. The interposition graft should be resized sharply, so that it is not under undue tension. Moreover, a redundant graft is prone to twisting, buckling, and resultant disruption of its flow after anastomosis. The ECA at the level of the bifurcation is first trapped using temporary clips, the distal end tied off, and then transected. Anastomosis to the ECA is performed in an end-to-end manner.
Figure 9: The cervical anastomosis is completed onto the CCA or ICA if the graft will be under less torsion in this alignment and configuration. The CCA may also be used as the donor vessel in patients with relatively inaccessible “high-riding” bifurcations. The left upper image demonstrates the use of a vascular punch to create the oval opening in the sidewall of the CCA. The location of the oval opening and vascular loops is evident (right upper image). The anastomosis is complete (lower images).
The arteriotomy site on the donor vessel is marked with an ink pen and the graft is prepared for anastomosis by “fish-mouthing” its end to increase the anastomotic surface area. An end-to-end anastomosis is performed using 7-0 nylon sutures. Prior to closing the last knot, a temporary clip is placed on the graft just distal to the anastomosis and the lumen is copiously irrigated with heparinized saline.
Flow is re-established in the proximal ECA by removing the temporary clip on the ECA to allow any arterial emboli and debris to be washed out. The ECA is then reclamped and the last knot is laid down. The distal temporary clip on the graft is removed first followed by the proximal one. The bleeding points or oozing are treated with application of Surgicel or Gelfoam and gentle tamponade. In cases of vigorous bleeding, additional sutures may be applied. A suction drain should be placed in the patient’s neck during closure to prevent a postoperative hematoma.
Intraoperative Assessment of Flow
The most important step after anastomosis is confirmation of bypass patency. Blood flow through the graft may be initially assessed through visual and tactile inspection for pulsatility.
Figure 10: Microdoppler ultrasonography is used to assess flow in the vessels (top image). Fluorescein or indocyanine green (ICG) angiography is more reliable as a minimally invasive and rapid technique to evaluate bypass flow intraoperatively (bottom image). Fluorescence angiography is easy to perform and can help identify areas of poor flow, stenosis, or occlusion.
The Charbel Micro-flowprobe (Transonic Systems, Ithaca, NY) is another minimally invasive tool that can quantitatively assess real-time blood flow through the graft intraoperatively. In contrast, microdoppler ultrasonography provides only a qualitative assessment.
Strategies for Facing Intraoperative Graft Failure
If the graft is occluded on intraoperative fluorescence angiography, both anastomoses sites and the tunneling of the graft should be inspected. If the patient has passed the BTO, it is possible that the contralateral competitive flow is overwhelming the flow in the interposition graft and revascularization is not needed.
If neuromonitoring does not detect any impending neurologic decline and careful inspection does not demonstrate any technical error, it may be best to leave the graft in place.
If changes in somatosensory or motor evoked potentials are detected and the graft is not functional, I reopen the distal (intracranial) anastomosis site followed by the proximal (extracranial) anastomosis site and irrigate all sites with heparinized saline solution. Both anastomoses are then reconstructed. Despite a second effort, if the interposition graft is not viable, not under tension or twisted, I reassess the safety of performing the bypass and consider closure of the intracranial arteriotomy without revascularization.
Postoperative Considerations
Evaluation in the intensive care unit includes hourly palpation and microdoppler ultrasonographic monitoring of the graft during the first postoperative day. This monitoring is subsequently spaced out to every 4 and 8 hours by the second and third postoperative days, respectively. Any concern regarding graft patency necessitates an immediate CT or catheter angiogram; otherwise a regular CT scan is obtained 24 hours after surgery.
Figure 11: The postoperative angiogram images for the patient in Figure 1 demonstrate a patent interposition graft and exclusion of the aneurysm.
During the first 48 hours after surgery, systemic hypertension is avoided to prevent hyperperfusion complications. In the case of radial artery grafts, perfusion of the hand is also assessed for the first 24 hours after the operation. Patients remain on subcutaneous heparin (5000 U every 8 hours) for the first 3 days and aspirin (325 mg daily) indefinitely. Follow-up CT angiogram imaging is again performed on follow-up at 3 months, 1 year, and every 2-5 years thereafter based on the underlying vascular pathology.
Bypass Patency
Recent advancements in EC-IC bypass techniques have significantly reduced morbidity and mortality rates to less than 7% and 2%, respectively, and have also increased graft patency rates from 66% to up to 95% in experienced hands.
For posterior circulation anastomosis, these rates are slightly lower. Thrombosis, sluggish flow, and intimal desquamation on the graft wall have been associated with lower patency rates; therefore, care must be taken to avoid mechanical trauma during surgery. Most graft failures occur within the first week after surgery and are likely related to surgical technique or coagulopathy. Almost all the grafts that are patent one week after surgery remain so at the 6-month follow-up evaluation.
New Anastomosis Technique
When compared with its low-flow counterpart, the high-flow EC-IC bypass has been correlated with higher risks of ischemic complications because larger and more proximal intracranial arteries are temporarily occluded during the performance of the anastomosis. To avoid cerebral ischemia during temporary occlusion, Tulleken and colleagues have described a novel method of anastomosis that can potentially decrease this risk.
Their technique uses an excimer laser beam to create an opening in the recipient vessel wall and thereby is called excimer laser-assisted nonocclusive anastomosis (ELANA). After the intracranial anastomosis has been performed, the cervical recipient is grafted without a need for temporary occlusion. The ELANA technique facilitates bypasses connected to larger and more proximal arteries with potentially no increased risk.
Pearls and Pitfalls
- High-flow EC–IC bypass is an important technique in the armamentarium of the cerebrovascular surgeon in providing flow replacement in cases of planned vessel sacrifice for various intracranial pathologies.
- Graft selection and bypass strategies are critical for successful high-flow EC–IC bypass.
Contributors: Tevfik Yılmaz, MD, Yiping Li, MD, and Mustafa K. Başkaya, MD
References
Alamanda VK, Tomycz L, Velez D, Singer RJ. Direct, high-flow bypass for a pediatric giant, fusiform aneurysm of the inferior division of M2: Case report and review of literature. J Surg Tech Case Rep. 2012;4:53-57.
Başkaya MK, Kiehn MW, Ahmed AS, Ateş O, Niemann DB. Alternative vascular graft for extracranial-intracranial bypass surgery: Descending branch of the lateral circumflex femoral artery. Neurosurg Focus. 2008;24:E8.
Hage ZA, Amin-Hanjani S, Charbel FT. Cerebral revascularization: State of the art: Part I—flow augmentation. Contemp Neurosurg. 2013;35:1–8
Hage ZA, Amin-Hanjani S, Charbel FT. Cerebral revascularization: State of the art: Part II—flow replacement. Contemp Neurosurg. 2013;35:1–8
Iihara K, Okawa M, Hishikawa T, Yamada N, Fukushima K, Iida H, Miyamoto S. Slowly progressive neuronal death associated with postischemic hyperperfusion in cortical laminar necrosis after high-flow bypass for a carotid intracavernous aneurysm. J Neurosurg. 2010; 112:1254-1259.
Kocaeli H, Andaluz N, Choutka O, Zuccarello M. Use of radial artery grafts in extracranial-intracranial revascularization procedures. Neurosurg Focus. 2008;24:E5.
Li Y, Cikla U, Baggott C, Yilmaz T, Chao C, Baskaya MK. Surgical treatment of adult Moyamoya disease with combined STA-MCA bypass and EDAS: Demonstration of technique in video presentation. Turk Neurosurg. 2015;25:126-131.
Mura J, Malogo-Tavares W, Figueiredo EG. Basic aspects of high flow extracranial–intracranial bypass: part I. Contemp Neurosurg. 2010;32:1–4
Quiñones-Hinojosa A, Du R, Lawton MT. Revascularization with saphenous vein bypasses for complex intracranial aneurysms. Skull Base. 2005;15:119-132.
Ramanathan D, Starnes B, Hatsukami T, Kim LJ, Di Maio S, Sekhar L. Tibial artery autografts: Alternative conduits for high flow cerebral revascularizations. World Neurosurg. 2013;80:322-327.
Rodríguez-Hernández A, Josephson SA, Langer D, Lawton MT. Bypass for the prevention of ischemic stroke. World Neurosurg. 2011;76(6 Suppl):S72-579.
Sanai N, Lawton MT. In situ bypass for complex intracranial aneurysms: Part I. Contemp Neurosurg. 2009;31:1–6.
Sia SF, Morgan MK. High flow extracranial-to-intracranial brain bypass surgery. J Clin Neurosci. 2013;20:1-5.
Tulleken CA, Streefkerk HJ, van der Zwan A. Construction of a new posterior communicating artery in a patient with poor posterior fossa circulation: technical case report. Neurosurgery. 2002;50:415-419.
Wanibuchi M, Mikuni N Cerebrovascular high-flow bypass for skull base pathologies. J Vasc Med Surg. 2013, 1:2.
Please login to post a comment.